Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Granularity matters – measles first- and second-dose vaccination coverage in Poland, 2014–2018
1
Department of Environmental Hazards Prevention, Allergology and Immunology, Doctoral School, Medical University, Warsaw, Poland
2
Department of Epidemiology and Biostatistics, Medical University, Warsaw, Poland
3
Department of Public Health, Medical University of Warsaw, Poland
4
Department of Environmental Hazards Prevention, Allergology and Immunology, Medical University, Warsaw, Poland
Corresponding author
Paulina Maria Nowicka
Department of Environmental Hazards Prevention, Allergology and Immunology, Doctoral School, Medical University of Warsaw, Poland
Department of Environmental Hazards Prevention, Allergology and Immunology, Doctoral School, Medical University of Warsaw, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Vaccination coverage of ≥95% is essential to interrupt measles transmission. Accurate measurement of vaccine uptake is critical for identifying vulnerable populations and guiding public health interventions. The aim of the study is to: present differences in the sufficient measles vaccination (MCV) coverage in Poland, measured at different granularity level, and to identify clusters with sufficient/insufficient MCV coverage.
Material and methods:
Data on MCV coverage was extracted from annual reports collected by sanitary-epidemiological stations in Poland between 2014–2018. Spatial analysis using Local Moran’s I was performed to identify neighbouring poviats with similar MCV rates and outlier areas with markedly dissimilar values.
Results:
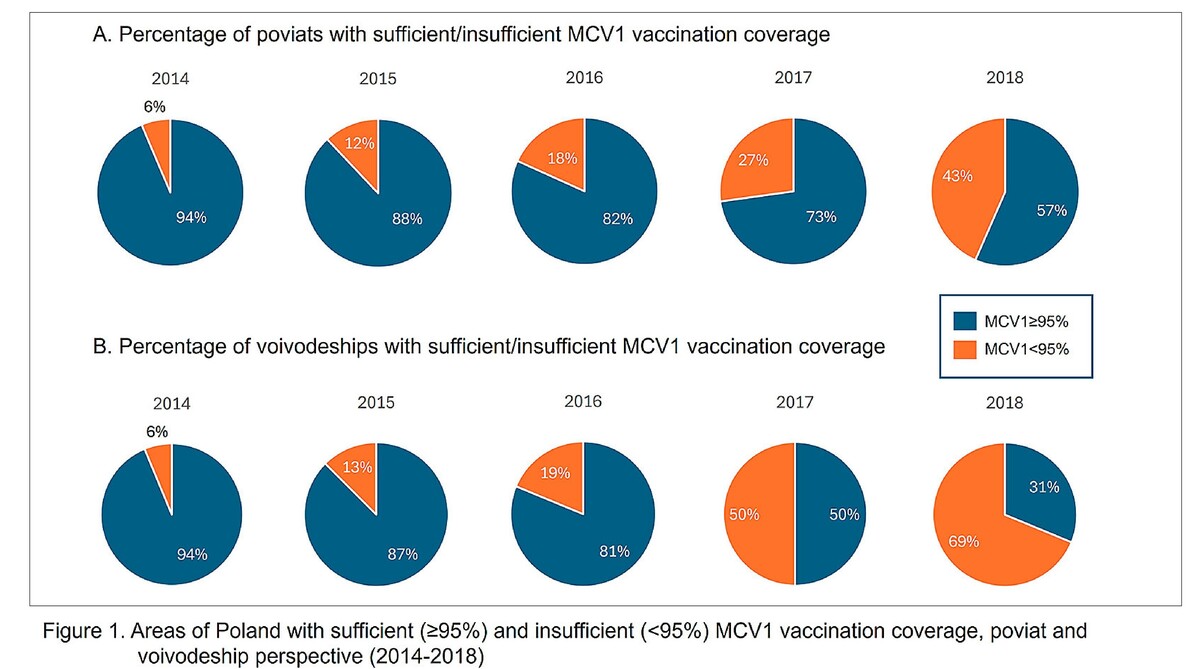
MCV coverage in Poland exhibited substantial spatial and temporal variability. The first dose of measles vaccination (MCV1) coverage ranged from 89% – 99% at the voivodeship level and from 80% to 100% at the poviat level, while the second dose measles vaccination (MCV2) coverage ranged from 84% – 99% and from 32.3% – 100%, respectively. Spatial disparities were particularly pronounced in several voivodeships, with Mazowieckie consistently demonstrating both the highest positive and negative deviations between poviat-level and voivodeship-level coverage. Statistically significant local spatial autocorrelation was observed in an increasing number of poviats for MCV1, rising from 14 in 2014 to 47 in 2018. For MCV2, the number of poviats with significant clustering fluctuated, peaking at 27 in 2015.
Conclusions:
The use of fine-grained poviat-level data revealed disparities in MCV coverage and localized gaps that would be obscured at the voivodeship level, underscoring the importance of high-resolution spatial analysis for guiding targeted vaccination efforts and improving public health equity.
Vaccination coverage of ≥95% is essential to interrupt measles transmission. Accurate measurement of vaccine uptake is critical for identifying vulnerable populations and guiding public health interventions. The aim of the study is to: present differences in the sufficient measles vaccination (MCV) coverage in Poland, measured at different granularity level, and to identify clusters with sufficient/insufficient MCV coverage.
Material and methods:
Data on MCV coverage was extracted from annual reports collected by sanitary-epidemiological stations in Poland between 2014–2018. Spatial analysis using Local Moran’s I was performed to identify neighbouring poviats with similar MCV rates and outlier areas with markedly dissimilar values.
Results:
MCV coverage in Poland exhibited substantial spatial and temporal variability. The first dose of measles vaccination (MCV1) coverage ranged from 89% – 99% at the voivodeship level and from 80% to 100% at the poviat level, while the second dose measles vaccination (MCV2) coverage ranged from 84% – 99% and from 32.3% – 100%, respectively. Spatial disparities were particularly pronounced in several voivodeships, with Mazowieckie consistently demonstrating both the highest positive and negative deviations between poviat-level and voivodeship-level coverage. Statistically significant local spatial autocorrelation was observed in an increasing number of poviats for MCV1, rising from 14 in 2014 to 47 in 2018. For MCV2, the number of poviats with significant clustering fluctuated, peaking at 27 in 2015.
Conclusions:
The use of fine-grained poviat-level data revealed disparities in MCV coverage and localized gaps that would be obscured at the voivodeship level, underscoring the importance of high-resolution spatial analysis for guiding targeted vaccination efforts and improving public health equity.
REFERENCES (31)
1.
Bednarczyk RA. Novel, Granular Methods to Monitor Vaccine Uptake and Associated Factors Within States. Am J Public Health. 2024;114(4):359–360. doi:10.2105/AJPH.2024.307594 (access: 2025.07.26).
2.
Sheng K, Chen K, Chen Y, et al. Innovative vaccine research through the lens of implementation science: fulfilling the strategic goals of the Immunization Agenda 2030. BMC Glob. Public Health. 2025;3(19). https://doi.org/10.1186/s44263... (access: 2025.07.26).
3.
Modlin J, Schaffner W, Orenstein W, et al. Triumphs of Immunization. J Infect Dis. 2021;224(4):307–S308. https://doi.org/10.1093/infdis... (access: 2025.07.26).
4.
Orenstein WA, Ahmed R. Simply put: Vaccination saves lives. Proc Natl Acad Sci U S A. 2017;114:4031–4033. doi:10.1073/pnas.1704507114 (access: 2025.07.26).
5.
Piot P, Larson HJ, O’Brien KL, et al. Immunization: vital progress, unfinished agenda. Nature 2019;575:119–129. https://doi.org/10.1038/s41586... (access: 2025.07.26).
6.
Ellwanger JH, Veiga ABG, Kaminski VL, et al. Control and prevention of infectious diseases from a One Health perspective. Genet Mol Biol. 2021;44:e20200256. doi:10.1590/1678-4685-GMB-2020-0256 (access: 2025.07.26).
7.
Bechini A, Boccalini S, Ninci A, et al. Childhood vaccination coverage in Europe: impact of different public health policies. Expert Rev Vaccines. 2019;18(7):693–701 doi:10.1080/14760584.2019.1639502 (access: 2025.07.27).
8.
World Health Organization. Immunization coverage. https://www.who.int/news-room/.... (access: 2025.08.01).
9.
World Health Organization Regional Office for Europe. Eliminating measles and rubella in the WHO European Region: Integrated guidance for surveillance, outbreak response and verification of elimination. 2024. https://www.who.int/europe/pub... (access: 2025.08.15).
10.
Pan American Health Organization. Ten countries in the Americas report measles outbreaks in 2025. https://www.paho.org/en/news/1... (access: 2025.08.15).
11.
European Centre for Disease Prevention and Control. Measles and Rubella monthly report. 31 July, 2025 (access: 2025.08.15).
12.
World Health Organization. European Immunization Agenda 2030. https://www.who.int/europe/pub... (access: 2025.08.01).
13.
Evans S, Schmitt J, Kalra D. Policy brief: Improving national vaccination decision-making through data. Front. Public Health. 2014;12. https://doi.org/10.3389/fpubh.....
14.
Montalti M, Kawalec A, Leoni E, et al. Measles Immunization Policies and Vaccination Coverage in EU/EEA Countries over the Last Decade. Vaccines. 2020;8(1):86. https://doi.org/10.3390/vaccin... (access: 2025.08.15).
15.
Partouche H, Gilberg S, Renard V, et al. Mandatory vaccination of infants in France: Is that the way forward? Eur J Gen Pract. 2019 Jan;25(1):49–54. doi:10.1080/13814788.2018.1561849 (access: 2025.08.15).
16.
Regulation of the Minister of Health and Social Welfare of 22 December 1975 on mandatory vaccinations. Journal of Laws 1976 No. 1 item 8.
17.
Announcement of the Speaker of the Sejm of the Republic of Poland of May 23, 2024, on the announcement of the consolidated text of the Act on the prevention and combating of infections and infectious diseases in humans. Journal of Laws of 2024, item 924.
18.
Regulation of the Minister of Health of 27 September 2023 on mandatory vaccinations. Journal of Laws of 2023, item 2077.
19.
Posobkiewicz M, Kalinowska-Morka J, Świekatowski B. Państwowa Inspekcja Sanitarna – 60 lat istnienia i 95-lecie funkcjonowania służb sanitarnych w Polsce. Przegl Epidemiol. 2015;69:113–119. https://www.przeglepidemiol.pz... (access: 2025.08.17).
20.
Regulation of the Council of Ministers of 19 December 2017 on the statistical research program of public statistics for 2018. Journal of Laws 2017, item 2471.
21.
National Institute of Public Health – National Institute of Hygiene – National Research Institute, Chief Sanitary Inspectorate. Vaccinations in Poland in 2018. Warsaw 2019. https://wwwold.pzh.gov.pl/oldp... (access: 2025.08.17).
24.
Lieu TA, Ray GT, Klein NP, et al. Geographic Clusters in Underimmunization and Vaccine Refusal. Pediatrics. 2015;135(2):280–289. https://doi.org/10.1542/peds.2... (access: 2025.09.25).
25.
Alvarez-Zuzek LG, Zipfel CM, Bansal S. Spatial clustering in vaccination hesitancy: The role of social influence and social selection. PLoS Comput Biol. 2022;18(10):e1010437. https://doi.org/10.1371/journa... (access: 2025.09.25).
26.
Kang B, Goldlust S, Lee EC. Spatial distribution and determinants of childhood vaccination refusal in the United States. Vaccine. 2023;41(20):3189–3195. doi:10.1016/j.vaccine.2023.04.019 (access: 2025.09.25).
27.
Cadena J, Falcone D, Marathe A, et al. Discovery of under immunized spatial clusters using network scan statistics, BMC Med Inform Decis Mak. 2019;19:28. doi:10.1186/s12911-018-0706-7 (access: 2025.09.25).
28.
Masters NB, Eisenberg MC, Delamater PL. Fine-scale spatial clustering of measles nonvaccination that increases outbreak potential is obscured by aggregated reporting data, Proc Natl Acad Sci USA. 2020:117(455):285514. doi:10.1073/pnas.2011529117.
29.
Mercogliano M, Valdecantos RL, Fevola G, et al. An ecological analysis of socio-economic determinants associated with paediatric vaccination coverage in the Campania Region: A population-based study, years 2003–2017. Vaccine X. 2024;18:100482. doi:10.1016/j.jvacx.2024.100482 (access: 2025.08.17).
30.
Varbanova V, Verelst F, Hens N, et al. Determinants of basic childhood vaccination coverage in European and OECD countries. Hum Vaccin Immunother. 2022;18(6):2123883. doi:10.1080/21645515.2022.2123883 (access: 2025.08.17).
31.
Suppli CH, Dreier JW, Rasmussen M, et al. Sociodemographic predictors are associated with compliance to a vaccination-reminder in 9692 girls age 14, Denmark 2014–2015. Prev Med Rep. 2018;10:93–99. doi:10.1016/j.pmedr.2018.02.005 (access: 2025.08.17).
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.