Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Socio-economic determinants of childhood vaccination coverage in high-income countries – a scoping review
1
Department of Environmental Hazards Prevention, Allergology and Immunology, Doctoral School, Medical University, Warsaw, Poland
Corresponding author
Paulina Maria Nowicka
Department of Environmental Hazards Prevention, Allergology and Immunology, Doctoral School, Medical University of Warsaw, Poland
Department of Environmental Hazards Prevention, Allergology and Immunology, Doctoral School, Medical University of Warsaw, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Vaccination remains a cornerstone of global public health, projected to prevent 51 million deaths between 2021–2030. Recent surges in vaccine-preventable diseases, including record measles cases in the USA, a rising number of pertussis outbreaks in Europe and the Americas, increased pneumococcal infections in Australia, signal deteriorating vaccination coverage in high-income countries. These emerging threats highlight the urgent need to examine the socio-economic variables associated with routine childhood immunization. The aim of this scoping review is to identify the socio-economic determinants of childhood vaccine coverage in high-income countries.
Review methods:
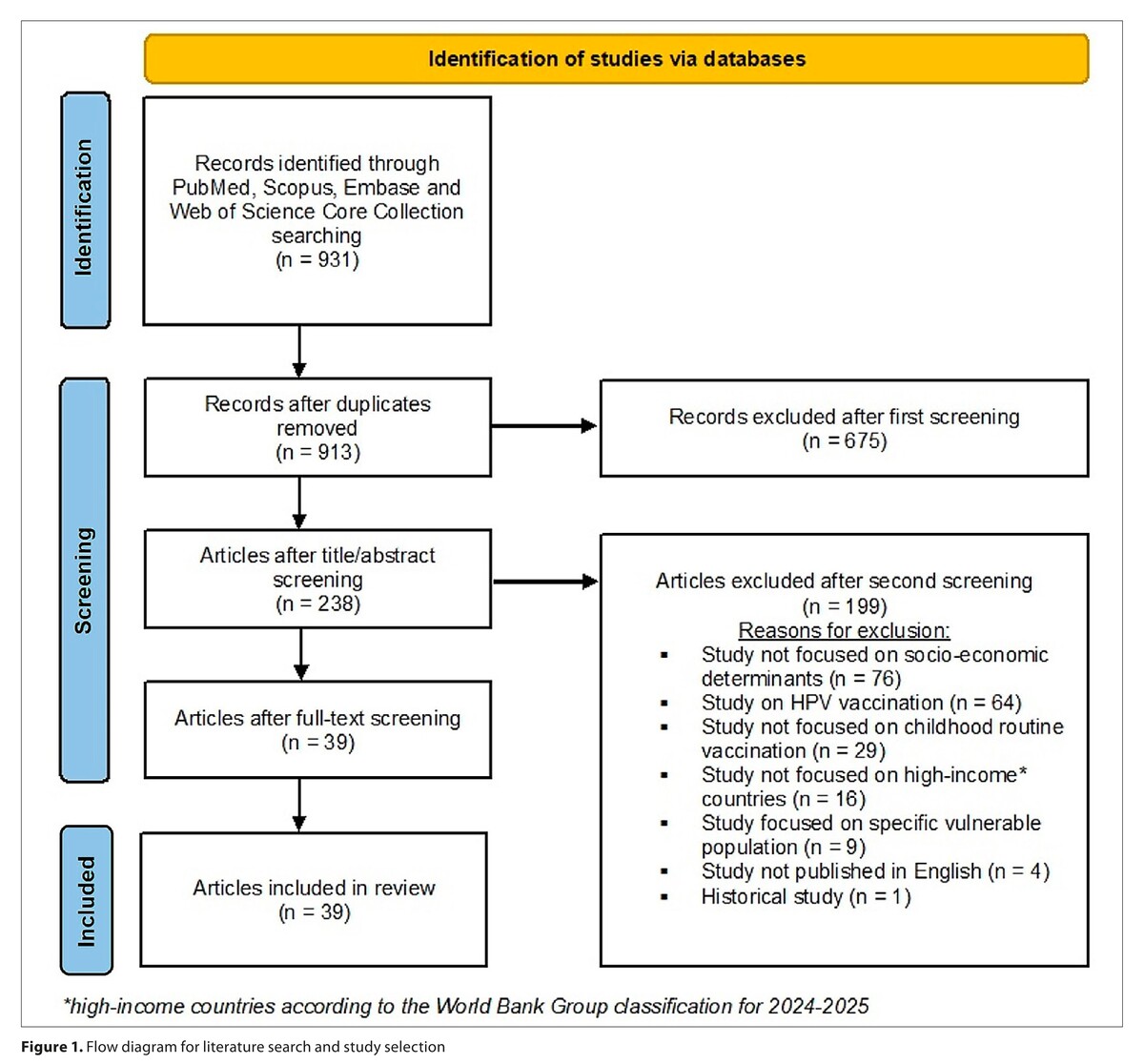
Four databases: PubMed, Scopus, Embase and the Web of Science Core Collection were searched for relevant studies published between January 2016 – July 2025.
Brief description of the state of knowledge:
Thirty-nine studies met the inclusion criteria. Childhood vaccination was associated with a variety of socio-economic factors. Key determinants of childhood vaccination coverage were: parental education, geographic location, ethnicity, household size and household income and insurance. While higher education, income, institutional support and living in an urban area were generally associated with higher coverage, hesitancy among educated and affluent groups also appeared. Lower vaccination coverage was associated with larger families, minority status, single parenthood, lack of insurance, deprivation, institutional district, and certain individual factors.
Summary:
The review underscores that vaccination coverage reflects broader societal systems, economic security, healthcare infrastructure, cultural context, and trust in institutions. Structural advantages in high-income countries may mask underlying inequities. Addressing these dimensions is essential for closing immunization gaps.
Vaccination remains a cornerstone of global public health, projected to prevent 51 million deaths between 2021–2030. Recent surges in vaccine-preventable diseases, including record measles cases in the USA, a rising number of pertussis outbreaks in Europe and the Americas, increased pneumococcal infections in Australia, signal deteriorating vaccination coverage in high-income countries. These emerging threats highlight the urgent need to examine the socio-economic variables associated with routine childhood immunization. The aim of this scoping review is to identify the socio-economic determinants of childhood vaccine coverage in high-income countries.
Review methods:
Four databases: PubMed, Scopus, Embase and the Web of Science Core Collection were searched for relevant studies published between January 2016 – July 2025.
Brief description of the state of knowledge:
Thirty-nine studies met the inclusion criteria. Childhood vaccination was associated with a variety of socio-economic factors. Key determinants of childhood vaccination coverage were: parental education, geographic location, ethnicity, household size and household income and insurance. While higher education, income, institutional support and living in an urban area were generally associated with higher coverage, hesitancy among educated and affluent groups also appeared. Lower vaccination coverage was associated with larger families, minority status, single parenthood, lack of insurance, deprivation, institutional district, and certain individual factors.
Summary:
The review underscores that vaccination coverage reflects broader societal systems, economic security, healthcare infrastructure, cultural context, and trust in institutions. Structural advantages in high-income countries may mask underlying inequities. Addressing these dimensions is essential for closing immunization gaps.
REFERENCES (51)
1.
Carter A, Msemburi W, Sim SY, et al. Modeling the Impact of Vaccination for the Immunization Agenda 2030: Deaths Averted Due to Vaccination Against 14 Pathogens in 194 Countries from 2021–2030. 2021. https://doi.org/10.2139/ssrn.3....
2.
World Health Organization. Increases in vaccine-preventable disease outbreaks threaten years of progress, warn WHO, UNICEF, Gavi. 2025. https://www.who.int/news/item/... (access: 2025.07.18).
3.
U.S. Measles Cases Hit Highest Level Since Declared Eliminated in 2000, https://publichealth.jhu.edu/i... (access: 2025.07.18).
4.
ECDC. Diphtheria strain involved in outbreaks among vulnerable populations across Europe between 2022 and 2025, https://www.ecdc.europa.eu/en/... (access: 2025.07.18).
5.
Khalil A, Samara A, Campbell H, et al. Recent increase in infant pertussis cases in Europe and the critical importance of antenatal immunizations: We must do better…now. Int J Infect Dis. 2024;146:107148. https://doi.org/10.1016/j.ijid....
6.
Pan American Health Organization, Epidemiological alert – Pertussis (whooping cough) in the Region of the Americas – 22 July 2024, https://www.paho.org/sites/def... (access: 2025.07.18).
7.
Japan Institute for Health Security, Risk assessment: Pertussis outbreak situation in Japan, 2025, https://id-info.jihs.go.jp/dis... (access: 2025.07.18).
8.
This disease can kill within days. Cases are surging across Australia, https://www.sbs.com.au/news/ar... (access: 2025.07.18).
9.
de Figueiredo A, Simas C, Karafillakis E, et al. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet 2020;396:898–908. https://doi.org/10.1016/S0140-....
10.
World Health Organization, Social determinants of health, https://www.who.int/news-room/... (access: 2025.07.18).
12.
Bocquier A, Ward J, Raude J, et al. Socioeconomic differences in childhood vaccination in developed countries: a systematic review of quantitative studies. Exp Rev. Vaccines 2017;16(11):1107–118. https://doi.org/10.1080/147605....
13.
Gellert FR, Gonzalez C, Mokdad AH. Bridging the gap: A mixed-methods analysis of Canadian and U.S. immunization programs for enhancing racial equity in childhood vaccinations. Vaccine.2025;57:127249. https://doi.org/10.1016/j.vacc....
14.
Nowicka PM, Lewandowski Z, Gujski M, et al. Socio-economic determinants of the second-dose measles vaccination coverage in Poland. Ann Agric Environ Med. 2025. https://doi.org/10.26444/aaem/....
15.
Scronias D, Fressard L, Fonteneau L, et al. Persistence of major socio-economic inequalities in childhood measles-mumps-rubella vaccination coverage and timeliness under vaccination mandates, France, 2015 to 2024. Euro Surveill. 2025;30(16):2400674. https://doi.org/10.2807/1560-7....
16.
Jary H, Pullen A, Howett D, et al. Sociodemographic inequalities in the epidemiology and vaccine uptake within a large outbreak of measles in Birmingham, England, 2023 to 2024. Euro Surveill. 2025;30(16):2400652. https://doi.org/10.2807/1560-7....
17.
Anzà D, Esposito M, Bertolazzi G, et al. Determinants of Rotavirus Vaccine Acceptance in an Area of Southern Italy with Low Vaccination Coverage: A Case-Control Study by the Health Belief Model Questionnaire. Vaccines (Basel). 2025;13(1):63. https://doi.org/10.3390/vaccin....
18.
Mercogliano M, Valdecantos RL, Fevola G, et al. An ecological analysis of socio-economic determinants associated with paediatric vaccination coverage in the Campania Region: A population-based study, years 2003–2017. Vaccine X. 2024;18:100482. https://doi.org/10.1016/j.jvac....
19.
La Fauci G, Soldà G, Di Valerio Z, et al. Rates and determinants of Rotavirus vaccine uptake among children in Italy: a cross-sectional study within the 2022 OBVIOUS* project. BMC Public Health. 2024;24(1):770. https://doi.org/10.1186/s12889....
20.
Jacques M, Lorton F, Dufourg MN, et al. Determinants of incomplete vaccination in children at age two in France: results from the nationwide ELFE birth cohort. Eur J Pediatr. 2023;182(3):1019–1028. https://doi.org/10.1007/s00431....
21.
Arzilli G, Stacchini L, Casigliani V, et al. Assessing vaccine hesitancy and health literacy using a new Italian vaccine confidence index and a modified Italian medical term recognition test: A cross-sectional survey on Italian parents. Hum Vaccin Immunother. 2023;19(3):2271765. https://doi.org/10.1080/216455....
22.
Michels SY, Niccolai LM, Hadler JL, et al. Failure to Complete Multidose Vaccine Series in Early Childhood. Pediatrics. 2023;152(2):e2022059844. https://doi.org/10.1542/peds.2....
23.
Perry M, Cottrell S, Gravenor MB, et al. Determinants of Equity in Coverage of Measles-Containing Vaccines in Wales, UK, during the Elimination Era. Vaccines (Basel). 2023;11(3):680. https://doi.org/10.3390/vaccin....
24.
Ilesanmi MM, Abonyi S, Pahwa P, et al. Trends, barriers and enablers to measles immunisation coverage in Saskatchewan, Canada: A mixed methods study. PLoS One. 2022;17(11):e0277876. https://doi.org/10.1371/journa....
25.
Shen AK, Grundmeier RW, Michel JJ. Trends in Vaccine Refusal and Acceptance using Electronic Health Records from a Large Pediatric Hospital Network, 2013–2020: Strategies for Change. Vaccines (Basel). 2022;10(10):1688. https://doi.org/10.3390/vaccin....
26.
Varbanova V, Verelst F, Hens N, et al. Determinants of basic childhood vaccination coverage in European and OECD countries. Hum Vaccin Immunother. 2022;18(6):2123883. https://doi.org/10.1080/216455....
27.
Vidal Fuertes C, Johns NE, Goodman TS, et al. The Association between Childhood Immunization and Gender Inequality: A Multi-Country Ecological Analysis of Zero-Dose DTP Prevalence and DTP3 Immunization Coverage. Vaccines (Basel). 2022;10(7):1032. https://doi.org/10.3390/vaccin....
28.
Tandy CB, Odoi A. Geographic disparities and predictors of vaccination exemptions in Florida: a retrospective study. Peer J. 2022;10:e12973. https://doi.org/10.7717/peerj.....
29.
Tal O, Ne’eman Y, Sadia R, et al. Parents’ attitudes toward children’s vaccination as a marker of trust in health systems. Hum Vaccin Immunother. 2021;17(11):4518–4528. https://doi.org/10.1080/216455....
30.
Marek L, Hobbs M, Wiki J, et al. Spatial-temporal patterns of childhood immunization in New Zealand (2006–2017): An improving pattern but not for all? Eur J Public Health. 2021;13;31(3):561–566. https://doi.org/10.1093/eurpub....
31.
Marek L, Hobbs M, McCarthy J, et al. Investigating spatial variation and change (2006–2017) in childhood immunisation coverage in New Zealand. Soc Sci Med. 2020;264:113292. https://doi.org/10.1016/j.socs....
32.
Bertoncello C, Ferro A, Fonzo M, et al. Socioeconomic Determinants in Vaccine Hesitancy and Vaccine Refusal in Italy. Vaccines (Basel). 2020;8(2):276. https://doi.org/10.3390/vaccin....
33.
Santorelli G, West J, Mason D, et al. Factors associated with the uptake of the UK routine childhood immunization schedule in a bi-ethnic population. Eur J Public Health. 2020;30(4):697–702. https://doi.org/10.1093/eurpub....
34.
Morrison M, Castro LA, Ancel Meyers L. Conscientious vaccination exemptions in kindergarten to eighth-grade children across Texas schools from 2012 to 2018: A regression analysis. PLoS Med. 2020;17(3):e1003049. https://doi.org/10.1371/journa....
35.
Carpiano RM, Polonijo AN, Gilbert N, et al. Socioeconomic status differences in parental immunization attitudes and child immunization in Canada: Findings from the 2013 Childhood National Immunization Coverage Survey (CNICS). Prev Med. 2019;123:278–287. https://doi.org/10.1016/j.ypme....
36.
Sugishita Y, Kurita J, Akagi T, et al. Determinants of Vaccination Coverage for the Second Dose of Measles-Rubella Vaccine in Tokyo, Japan. Tohoku J Exp Med. 2019;249(4):265–273. https://doi.org/10.1620/tjem.2....
37.
Rafferty E, Guo X, McDonald B, et al. Measurement of coverage, compliance and determinants of uptake in a publicly funded rotavirus vaccination programme: a retrospective cohort study. BMJ Open. 2019;9(11):e031718. https://doi.org/10.1136/bmjope....
38.
Haider EA, Willocks LJ, Anderson N. Identifying inequalities in childhood immunisation uptake and timeliness in southeast Scotland, 2008–2018: A retrospective cohort study. Vaccine. 2019;37(37):5614–5624. https://doi.org/10.1016/j.vacc....
39.
Tur-Sinai A, Gur-Arie R, Davidovitch N, et al. Vaccination uptake and income inequalities within a mass vaccination campaign. Isr J Health Policy Res. 2019;8(1):63. https://doi.org/10.1186/s13584....
40.
Oster NV, Williams EC, Unger JM, et al. Sociodemographic, clinical and birth hospitalization characteristics and infant Hepatitis B vaccination in Washington State. Vaccine. 2019;37(38):5738–5744. https://doi.org/10.1016/j.vacc....
41.
Toffolutti V, McKee M, Melegaro A, et al. Austerity, measles and mandatory vaccination: cross-regional analysis of vaccination in Italy 2000–14. Eur J Public Health. 2019;29(1):123–127. https://doi.org/10.1093/eurpub....
42.
Kiely M, Boulianne N, Talbot D, et al. Impact of vaccine delays at the 2, 4, 6 and 12 month visits on incomplete vaccination status by 24 months of age in Quebec, Canada. BMC Public Health. 2018;18(1):1364. https://doi.org/10.1186/s12889....
43.
Suppli CH, Dreier JW, Rasmussen M, et al. Sociodemographic predictors are associated with compliance to a vaccination-reminder in 9692 girls age 14, Denmark 2014–2015.Prev Med Rep. 2018;10:93–99. https://doi.org/10.1016/j.pmed....
44.
Lu PJ, Yankey D, Jeyarajah J, et al. Association of Health Insurance Status and Vaccination Coverage among Adolescents 13–17 Yearsof Age. J Pediatr. 2018;195:256–262.e1. https://doi.org/10.1016/j.jped....
45.
Danchin MH, Costa-Pinto J, Attwell K, et al. Vaccine decision-making begins in pregnancy: Correlation between vaccine concerns, intentions and maternal vaccination with subsequent childhood vaccine uptake. Vaccine. 2018;36(44):6473–6479. https://doi.org/10.1016/j.vacc....
46.
Nic Lochlainn LM, Woudenberg T, van Lier A, et al. A novel measles outbreak control strategy in the Netherlands in 2013–2014 using a national electronic immunization register: A study of early MMR uptake and its determinants. Vaccine. 2017;35(43):5828–5834. https://doi.org/10.1016/j.vacc....
47.
Anello P, Cestari L, Baldovin T, et al. Socioeconomic factors influencing childhood vaccination in two northern Italian regions. Vaccine. 2017;35(36):4673–4680. https://doi.org/10.1016/j.vacc....
48.
Stein-Zamir C, Israeli A. Age-appropriate versus up-to-date coverage of routine childhood vaccinations among young children in Israel. Hum Vaccin Immunother. 2017;13(9):2102–2110. https://doi.org/10.1080/216455....
49.
Gilbert NL, Gilmour H, Wilson SE, et al. Determinants of non-vaccination and incomplete vaccination in Canadian toddlers. Hum Vaccin Immunother. 2017;13(6):1–7. https://doi.org/10.1080/216455....
50.
Hill HA, Elam-Evans LD, Yankey D, et al. Vaccination Coverage Among Children Aged 19–35 Months – United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65(39):1065–1071. https://doi.org/10.15585/mmwr.....
51.
Bernstein S, North A, Schwartz J, et al. State-Level Voting Patterns and Adolescent Vaccination Coverage in the United States, 2014. Am J Public Health. 2016;106(10):1879–81. https://doi.org/10.2105/AJPH.2....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.