Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Bottlenecks in lung cancer diagnostics cause poorer prognosis in this cancer – experience of a single oncology centre
1
Department of Pneumonology, Oncology and Allergology, Medical University, Lublin, Poland
These authors had equal contribution to this work
Corresponding author
Karolina Nalewaj
Department of Pneumonology, Oncology and Allergology, Medical University of Lublin, Poland, Jaczewskiego 8, 20-090, Lublin, Poland
Department of Pneumonology, Oncology and Allergology, Medical University of Lublin, Poland, Jaczewskiego 8, 20-090, Lublin, Poland
KEYWORDS
lung cancerantibioticsdelayslung cancer diagnosispulmonary infection and delayed cancer diagnosisrole of GPs in lung cancer diagnosislung cancer symptomsNSLCprimary care
TOPICS
ABSTRACT
Introduction and objective:
Lung cancer remains the leading cause of death from malignant tumours worldwide. Delays in the diagnosis of lung cancer in primary and specialist health care result in a high stage of the disease, lack of possibility of radical treatment, and the shortening of the life expectancy of patients. The aim of the study is to determine factors contributing to delays in the diagnosis of lung cancer in patients in the Lublin Province in south-east Poland. The study focuses on factors that influence the overall survival of patients.
Material and methods:
An anonymous survey was conducted among 249 patients diagnosed with lung cancer. 150 of the hospitalized patients were men (60.24%) and 99 women (39.76%). Data analysis was performed using Statistica software.
Results:
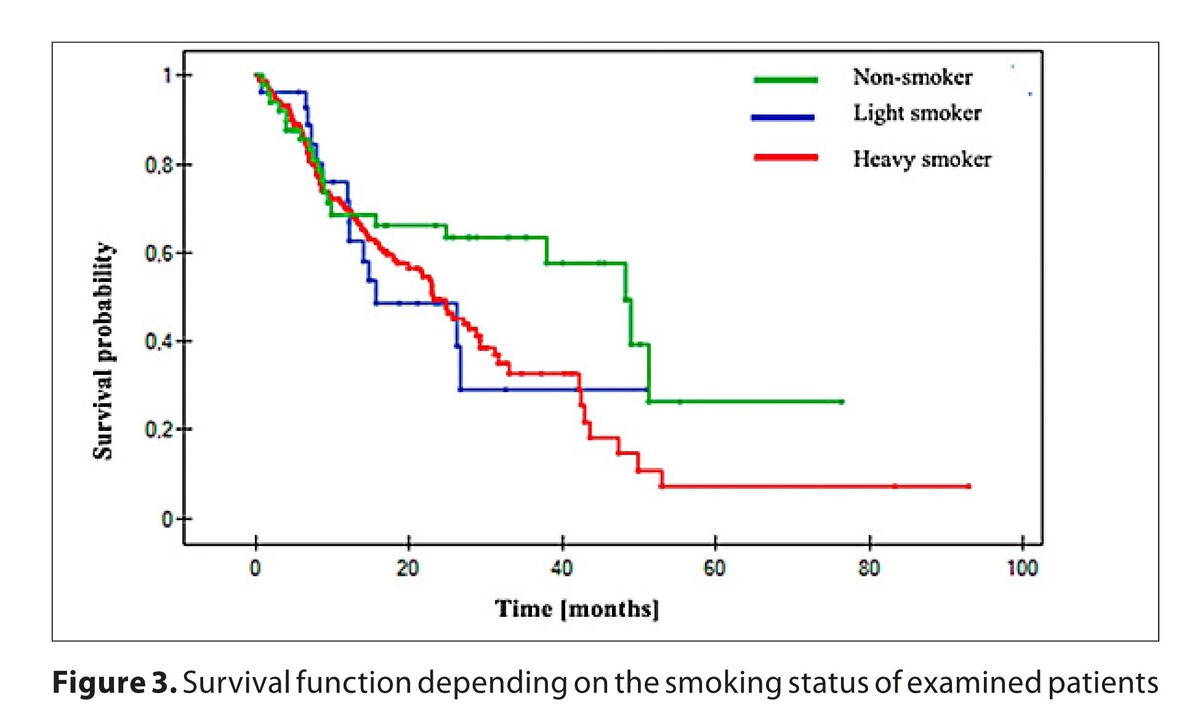
The average time from the first symptoms to diagnosis was 13.5 weeks. Patients with respiratory infections and treated with antibiotics up to 6 months before diagnosis experienced a significantly (p<0.00001) longer wait to final diagnosis. The median survival time for all patients was 25.7 months. A long time from first symptoms to diagnosis had a significant (p=0.046) impact on the estimated survival time.
Conclusions:
The results of the study showed that delays in the diagnosis of patients with lung cancer hospitalized in the Lublin Province were significant and contributed to shortening the survival time. It is necessary to introduce an algorithm for the diagnosis path of patients with symptoms of lung cancer
Lung cancer remains the leading cause of death from malignant tumours worldwide. Delays in the diagnosis of lung cancer in primary and specialist health care result in a high stage of the disease, lack of possibility of radical treatment, and the shortening of the life expectancy of patients. The aim of the study is to determine factors contributing to delays in the diagnosis of lung cancer in patients in the Lublin Province in south-east Poland. The study focuses on factors that influence the overall survival of patients.
Material and methods:
An anonymous survey was conducted among 249 patients diagnosed with lung cancer. 150 of the hospitalized patients were men (60.24%) and 99 women (39.76%). Data analysis was performed using Statistica software.
Results:
The average time from the first symptoms to diagnosis was 13.5 weeks. Patients with respiratory infections and treated with antibiotics up to 6 months before diagnosis experienced a significantly (p<0.00001) longer wait to final diagnosis. The median survival time for all patients was 25.7 months. A long time from first symptoms to diagnosis had a significant (p=0.046) impact on the estimated survival time.
Conclusions:
The results of the study showed that delays in the diagnosis of patients with lung cancer hospitalized in the Lublin Province were significant and contributed to shortening the survival time. It is necessary to introduce an algorithm for the diagnosis path of patients with symptoms of lung cancer
REFERENCES (34)
1.
Wojciechowska U, Barańska K, Miklewska M, et al. Cancer incidence and mortality in Poland in 2020. Cancers J Oncol. 2023;73(3):129–145. doi:10.5603/NJO.2023.0026.
2.
Wojciechowska U, Barańska K, Miklewska M, et al. Cancer incidence and mortality in Poland in 2023. Cancers J Oncol. 2024;74(2):75–93. doi:10.5603/njo.99065.
3.
Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74(3):229–263. doi:10.3322/caac.21834.
4.
Thandra KC, Barsouk A, Saginala K, et al. Epidemiology of lung cancer, Contemp Oncol (Pozn). 2021;25(1):45–52. doi:10.5114/wo.2021.103829.
5.
Lewandowska A, Lewandowski T, Zych B, et al. Risk factors for the diagnosis of lung cancer in Poland: a large-scale, population-based case-control study. Asian Pac J Cancer Prev. 2022;23(10):3299–3307. doi:10.31557/APJCP.2022.23.10.3299.
6.
Saab MM, O’Driscoll M, FitzGerald S, et al. Primary healthcare professionals’ perspectives on patient help-seeking for lung cancer warning signs and symptoms: a qualitative study. BMC Prim Care. 2022;23(1):119. doi:10.1186/s12875-022-01730-x.
7.
Domagala-Kulawik J, Trojnar A. Lung cancer in women in 21th century. J Thorac Dis. 2020;12(8):4398–4410. doi:10.21037/jtd-20-287.
8.
Nalewaj KP, Krawczyk P, Chmielewska I, et al. Delays in the diagnosis of lung cancer patients in Poland. Oncol Clin Pract. 2023;19(1):22–27. doi:10.5603/OCP.2022.0052.
9.
Bradley SH, Kennedy MP, Neal RD. Recognising lung cancer in primary care. Adv Ther. 2019;36(1):19–30. doi:10.1007/s12325-018-0843-5.
10.
Naqvi KF, Mazzone SB, Shiloh MU. Infectious and inflammatory pathways to cough. Annu Rev Physiol. 2023;85:71–91. doi:10.1146/annurev-physiol-031422-092315.
11.
Haastrup PF, Jarbøl DE, Balasubramaniam K, et al. Predictive values of lung cancer alarm symptoms in the general population: a nationwide cohort study. NPJ Prim Care Respir Med. 2020;30(1):15. doi:10.1038/s41533-020-0173-3.
12.
Li R, Li J, Zhou X. Lung microbiome: new insights into the pathogenesis of respiratory diseases. Signal Transduct Target Ther. 2024;9(1):19. doi:10.1038/s41392-023-01722-y.
13.
Prado MG, Kessler LG, Au MA, et al. Symptoms and signs of lung cancer prior to diagnosis: case-control study using electronic health records from ambulatory care within a large US-based tertiary care centre. BMJ Open. 2023;13(4):e068832. doi:10.1136/bmjopen-2022-068832.
14.
Barahman M, Shamsaei G, Kashipazha D, et al. Paraneoplastic neurological syndromes of small cell lung cancer. Postep Psychiatr Neurol. 2024;33(2):80–92. doi:10.5114/ppn.2024.141157.
15.
Wickramasinghe B, Renzi C, Barclay M, et al. Pre-diagnostic prescribing patterns in dyspnoea patients with as-yet-undiagnosed lung cancer: A longitudinal study of linked primary care and cancer registry data. Cancer Epidemiol. 2023;86:102429. doi:10.1016/j.canep.2023.102429.
16.
Weinberg FD, Zhao L, Chellappa N, et al. Characterization of pneumonia and other factors leading to poorer survival across all age groups in patients with non-small cell lung cancer (NSCLC). J Thorac Dis. 2021;13(2):986–994. doi:10.21037/jtd-20-2891.
17.
Purdie S, Creighton N, White KM, et al. Pathways to diagnosis of non-small cell lung cancer: a descriptive cohort study. NPJ Prim Care Respir Med. 2019;29(1):2. doi:10.1038/s41533-018-0113-7.
18.
Lancaster HL, Heuvelmans MA, Oudkerk M. Low-dose computed tomography lung cancer screening: clinical evidence and implementation research. J Intern Med. 2022;292(1):68–80. doi:10.1111/joim.13480.
19.
Aguiar WWS, Bonomi DO, Martins NF, et al. Lung cancer screening: a mini review of the major trials and guidelines. Rev Assoc Med Bras 2024;70(suppl 1):e2024S111. doi:10.1590/1806-9282.2024S111.
20.
Price S, Spencer A, Zhang X, et al. Trends in time to cancer diagnosis around the period of changing national guidance on referral of symptomatic patients: a serial cross-sectional study using UK electronic healthcare records from 2006–17. Cancer Epidemiol. 2020;69:101805. doi:10.1016/j.canep.2020.101805.
21.
Osowiecka K, Rucinska M, Nowakowski JJ, et al. How long are cancer patients waiting for oncological therapy in Poland? Int J Environ Res Public Health. 2018;15(4):577. doi:10.3390/ijerph15040577.
22.
Swann R, McPhail S, Witt J, et al. National Cancer Diagnosis Audit Steering Group. Diagnosing cancer in primary care: results from the National Cancer Diagnosis Audit. Br J Gen Pract. 2018;68(666):e63–e72. doi:10.3399/bjgp17X694169.
23.
Ellis PM, Vandermeer R. Delays in the diagnosis of lung cancer. J Thorac Dis. 2011;3(3):183–8. doi:10.3978/j.issn.2072-1439.2011.01.01.
24.
Guirado M, Fernández ME, Fernández VA, et al. Clinical impact of delays in the management of lung cancer patients in the last decade: systematic review. Clin Transl Oncol. 2022;24(8):1549–1568. doi:10.1007/s12094-022-02796-w.
25.
Tsai CH, Kung PT, Kuo WY, et al. Effect of time interval from diagnosis to treatment for non-small cell lung cancer on survival: a national cohort study in Taiwan. BMJ Open. 2020;10(4):e034351. doi:10.1136/bmjopen-2019-034351.
26.
Bergman M, Fountoukidis G, Smith D, et al. Effect of smoking on treatment efficacy and toxicity in patients with cancer: a systematic review and meta-analysis. Cancers (Basel). 2022;14(17):4117. doi:10.3390/cancers14174117.
27.
Schane RE, Ling PM, Glantz SA. Health effects of light and intermittent smoking: a review. Circulation. 2010;121(13):1518–22. doi:10.1161/CIRCULATIONAHA.109.904235.
28.
Hung HY, Tseng YH, Chao HS, et al. Multidisciplinary team discussion results in survival benefit for patients with stage III non-small-cell lung cancer. PLoS One. 2020;15(10):e0236503. doi:10.1371/journal.pone.0236503.
29.
Sagan A, Kowalska-Bobko I, Gałązka-Sobotka, et al. Assessing recent efforts to improve organization of cancer care in Poland: what does the evidence tell us? Int J Environ Res Public Health. 2022;19(15):9369. doi:10.3390/ijerph19159369.
30.
Guo H, Li H, Zhu L, et al. “How long have I got?” in stage IV NSCLC. Patients with at least 3 months up to 10 years survival, accuracy of long-, intermediate-, and short-term survival prediction is not good enough to answer this question. Front Oncol. 2021;11:761042. doi:10.3389/fonc.2021.761042.
31.
American Cancer Society. Cancer Facts & Figures 2024. Atlanta: American Cancer Society; 2024. Available from: https://www.cancer.org/cancer/....
32.
Schussler O, Bobbio A, Dermine H, et al. Twenty-year survival of patients operated on for non-small-cell lung cancer: the impact of tumor stage and patient-related parameters. Cancers (Basel). 2022;14(4):874. doi:10.3390/cancers14040874.
33.
Alifano M, Mansuet-Lupo A, Lococo F, et al. Systemic inflammation, nutritional status and tumor immune microenvironment determine outcome of resected non-small cell lung cancer. PLoS ONE. 2014;9:e106914. doi:10.1371/journal.pone.0106914.
34.
Kasymjanova G, Small D, Cohen V, et al. Lung cancer care trajectory at a Canadian centre: an evaluation of how wait times affect clinical outcomes. Curr Oncol. 2017;24(5):302–309. doi:10.3747/co.24.3611.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.