Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Predictive factors for severe obstructive sleep apnea – a single-hospital retrospective study
1
First Department of General and Transplant Surgery and Nutritional Treatment, Medical University, Lublin, Poland
2
Doctoral School, Medical University, Lublin, Poland
3
Department of Clinical Neuropsychiatry, Medical University, Lublin, Poland
Corresponding author
Aleksander Janusz Ryczkowski
First Department of General and Transplant Surgery and Nutritional Treatment, Medical University of Lublin, Jaczewskiego 8, 20-090, Lublin, Poland
First Department of General and Transplant Surgery and Nutritional Treatment, Medical University of Lublin, Jaczewskiego 8, 20-090, Lublin, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Severe obstructive sleep apnea (OSA), defined by the Apnea Hypopnea Index as AHI ≥30, is associated with increased cardiovascular, metabolic, and neurocognitive risks but is frequently overlooked in primary care. The aim of this study is to identify the predictors of severe OSA, and to derive a simple, easy-to-use a clinical model as a guide for pre-specialist triage.
Material and methods:
A retrospective single-centre study was carried out of 278 consecutively hospitalized adults assessed for sleep-disordered breathing (Lublin, 2018–2020). Polygraphy/polysomnography provided AHI and oximetry indices. Receiver operating characteristics (ROC) analyses identified thresholds for continuous variables; predictors were tested in univariate and multivariable logistic regression. Primary outcome: severe OSA (AHI ≥30).
Results:
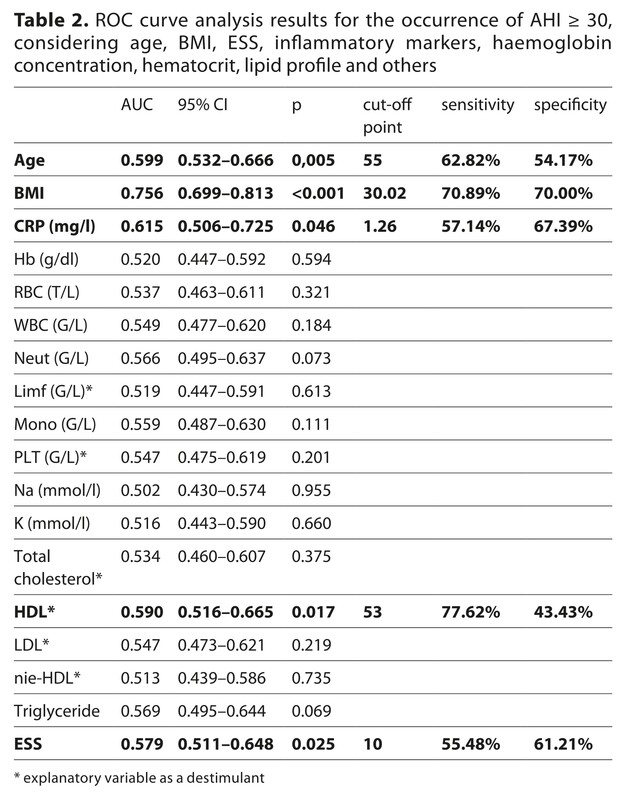
Severe OSA occurred in 56.8% of patients (158/278). ROC analysis suggested cut-offs at: age ≥55 years, body mass index (BMI) ≥30 kg/m², Epworth Sleepiness Scale (ESS) ≥10, and High Dense Lipoprotein (HDL) ≤53 mg/dL (best performance for BMI: area under curve (AUC) 0.756; sensitivity 70.9%, specificity 70.0%). In multivariable models, independent predictors included: BMI ≥30 (OR 5.37, 95% CI 2.70–10.70), age ≥55 (OR 2.66, 95% CI 1.36–5.20), and ESS ≥10 (OR 2.77, 95% CI 1.46–5.21). A three-item rule (age, BMI, ESS) produced predicted probabilities over 50% for several combinations, and overall discrimination was approximately 0.75.
Conclusions:
Obesity is the strongest predictor of severe OSA, with additional influences from older age and daytime sleepiness. A simple three-item rule may assist primary care in triaging referrals for sleep testing; external validation is necessary.
Severe obstructive sleep apnea (OSA), defined by the Apnea Hypopnea Index as AHI ≥30, is associated with increased cardiovascular, metabolic, and neurocognitive risks but is frequently overlooked in primary care. The aim of this study is to identify the predictors of severe OSA, and to derive a simple, easy-to-use a clinical model as a guide for pre-specialist triage.
Material and methods:
A retrospective single-centre study was carried out of 278 consecutively hospitalized adults assessed for sleep-disordered breathing (Lublin, 2018–2020). Polygraphy/polysomnography provided AHI and oximetry indices. Receiver operating characteristics (ROC) analyses identified thresholds for continuous variables; predictors were tested in univariate and multivariable logistic regression. Primary outcome: severe OSA (AHI ≥30).
Results:
Severe OSA occurred in 56.8% of patients (158/278). ROC analysis suggested cut-offs at: age ≥55 years, body mass index (BMI) ≥30 kg/m², Epworth Sleepiness Scale (ESS) ≥10, and High Dense Lipoprotein (HDL) ≤53 mg/dL (best performance for BMI: area under curve (AUC) 0.756; sensitivity 70.9%, specificity 70.0%). In multivariable models, independent predictors included: BMI ≥30 (OR 5.37, 95% CI 2.70–10.70), age ≥55 (OR 2.66, 95% CI 1.36–5.20), and ESS ≥10 (OR 2.77, 95% CI 1.46–5.21). A three-item rule (age, BMI, ESS) produced predicted probabilities over 50% for several combinations, and overall discrimination was approximately 0.75.
Conclusions:
Obesity is the strongest predictor of severe OSA, with additional influences from older age and daytime sleepiness. A simple three-item rule may assist primary care in triaging referrals for sleep testing; external validation is necessary.
REFERENCES (23)
1.
Punjabi NM. The Epidemiology of Adult Obstructive Sleep Apnea. Proc Am Thorac Soc. 2008;5(2):136–143.doi:10.1513/pats.200709-155MG.
2.
Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med Rev. 2017;34:70–81. doi:10.1016/j.smrv.2016.07.002.
3.
Tregear S, Reston J, Schoelles K, Phillips B. Obstructive Sleep Apnea and Risk of Motor Vehicle Crash: Systematic Review and Meta-Analysis. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2009;5(6):573–581.
4.
Pocobelli G, Akosile MA, Hansen RN, et al. Obstructive sleep apnea and risk of motor vehicle accident. Sleep Med. 2021;85:196–203. doi:10.1016/j.sleep.2021.07.019.
5.
Salari N, Khazaie H, Abolfathi M, et al. The effect of obstructive sleep apnea on the increased risk of cardiovascular disease: a systematic review and meta-analysis. Neurol Sci. 2022;43(1):219–231. doi:10.1007/s10072-021-05765-3.
6.
Ge X, Han F, Huang Y, et al. Is Obstructive Sleep Apnea Associated with Cardiovascular and All-Cause Mortality? PLOS ONE. 2013;8(7):e69432. doi:10.1371/journal.pone.006943.
7.
Riha RL, Celmina M, Cooper B, et al. ERS technical standards for using type III devices (limited channel studies) in the diagnosis of sleep disordered breathing in adults and children. Eur Respir J. 2023;61(1). doi:10.1183/13993003.00422-2022.
8.
Alenezi MA, Alabdulathim S, Alhejaili SAM, et al. The Association Between Obesity and the Development and Severity of Obstructive Sleep Apnea: A Systematic Review. Cureus. 2024;16(9):e69962. doi:10.7759/cureus.69962.
9.
Esmaeili N, Gell L, Imler T, et al. The relationship between obesity and obstructive sleep apnea in four community-based cohorts: an individual participant data meta-analysis of 12,860 adults. eClinicalMedicine. 2025;83:103221. doi:10.1016/j.eclinm.2025.103221.
10.
Shiina K. Obstructive sleep apnea -related hypertension: a review of the literature and clinical management strategy. Hypertens Res. 2024;47(11):3085–3098. doi:10.1038/s41440-024-01852-y.
11.
Malhotra A, Bednarik J, Chakladar S, et al. Tirzepatide for the treatment of obstructive sleep apnea: Rationale, design, and sample baseline characteristics of the SURMOUNT -OSA phase 3 trial. Contemp Clin Trials. 2024;141:107516. doi:10.1016/j.cct.2024.107516.
12.
Lee YC, Lu CT, Chuang LP, et al. Pharmacotherapy for obstructive sleep apnea – A systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2023;70:101809. doi:10.1016/j.smrv.2023.101809.
13.
Iftikhar IH, Reynolds AM, AlBisher E, et al. Aerobic exercise training and obstructive sleep apnea: dose-response meta-analyses. Sleep Breath Schlaf Atm. 2024;28(6):2355–2366. doi:10.1007/s11325-024-03158-2.
14.
Antonaglia C, Passuti G. Obstructive sleep apnea syndrome in non-obese patients. Sleep Breath. 2022;26(2):513–518. doi:10.1007/s11325-021-02412-1.
15.
Feltner C, Wallace IF, Aymes S, et al. Screening for Obstructive Sleep Apnea in Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2022;328(19):1951–1971. doi:10.1001/jama.2022.18357.
16.
Yang Y, Sun X, Liang J, et al. Optimizing Obstructive Sleep Apnea Risk Assessment in Hypertension: Development of a Predictive Nomogram in China. Nat Sci Sleep. 2025;17:285–295. doi:10.2147/NSS.S486186.
17.
Hou H, Zhao Y, Yu W, et al. Association of obstructive sleep apnea with hypertension: A systematic review and meta-analysis. J Glob Health. 8(1):010405. doi:10.7189/jogh.08.010405.
18.
Siddiquee AT, Kim S, Thomas RJ, Lee MH, Ku Lee S, Shin C. Obstructive sleep apnoea and long-term risk of incident diabetes in the middle-aged and older general population. ERJ Open Res. 2023;9(2):00401–02022. doi:10.1183/23120541.00401-2022.
19.
Soler X, Liao SY, Marin JM, et al. Age, gender, neck circumference, and Epworth sleepiness scale do not predict obstructive sleep apnea (OSA) in moderate to severe chronic obstructive pulmonary disease (COPD): The challenge to predict OSA in advanced COPD. PLOS ONE. 2017;12(5):e0177289. doi:10.1371/journal.pone.0177289.
20.
Garlicka A. Possibilities of predicting severe stages of obstructive sleep apnea and deep desaturation using criteria available to primary care physicians. thesis. Chair and Department of Family Medicine; 2021.
21.
Tong J, Yu Q, Li Y, Du J, Qiu J. Obstructive sleep apnea and cardiovascular events in acute coronary syndrome: a meta-analysis. Coron Artery Dis. 2023;34(3):177–184. doi:10.1097/MCA.0000000000001207.
22.
Kovbasyuk Z, Ramos-Cejudo J, Parekh A, et al. Obstructive Sleep Apnea, Platelet Aggregation, and Cardiovascular Risk. J Am Heart Assoc. 2024;13(15):e034079. doi:10.1161/JAHA.123.034079.
23.
Yuan F, Hu Y, Xu F, Feng X. A review of obstructive sleep apnea and lung cancer: epidemiology, pathogenesis, and therapeutic options. Front Immunol. 2024;15. doi:10.3389/fimmu.2024.1374236.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.