Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Acne therapy, probiotics and their influence on the microbiota
1
Faculty of Medicine, Medical University, Lublin, Poland
2
Department of Dermatology, Venereology and Paediatric Dermatology, Medical University, Lublin, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Many drugs that affect the skin microbiota are used in acne therapy. In recent years, many studies have proved that different groups of drugs change the composition of the microbiota in different ways. The aim of the study is to compare the impact of individual groups of drugs on the microbiota.
Review methods:
The Pubmed and Google Scholar databases were used to search for articles published from 2016–2024.
Brief description of the state of knowledge:
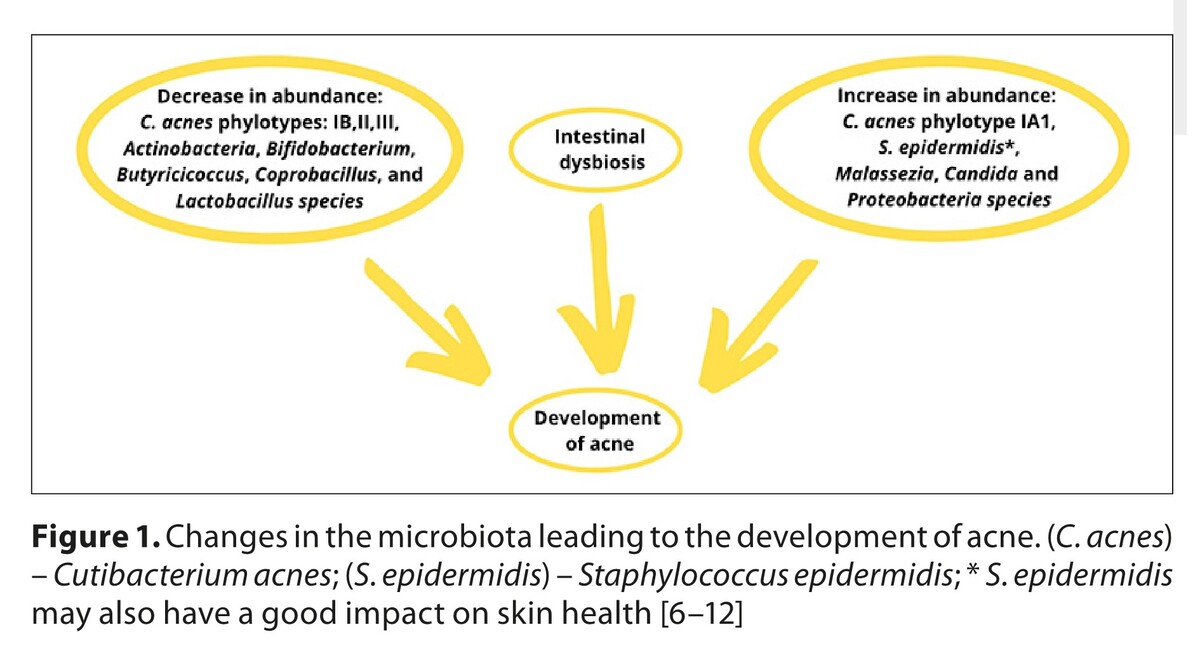
Drugs such as benzoyl peroxide, antibiotics, photodynamic therapy, and retinoids, cause clinical improvement of acne in patients and reduce the population of Cutibacterium acnes, but their influence on the diversity of the microbiota is different. A major problem today is the increase in bacterial resistance to antibiotics. As a result, new generation antibiotics have been created, which can be an effective tool in the fight against resistance. Currently, probiotics can be added to conventional therapy, some of which, e.g. PEG-8 Laurate, have a synergistic effect with other forms of treatment. Moreover, probiotics are becoming a promising form of treatment, modifying intestinal and skin microflora, impacting immune function, and restoring balance.
Summary:
Acne treatment significantly alters the composition of the human microbiota, which is why it is important to restore the natural composition of the microbiota in the treatment of this disease. Therefore, treatment options should be sought that will change the composition of the microbiota towards that of healthy people
Many drugs that affect the skin microbiota are used in acne therapy. In recent years, many studies have proved that different groups of drugs change the composition of the microbiota in different ways. The aim of the study is to compare the impact of individual groups of drugs on the microbiota.
Review methods:
The Pubmed and Google Scholar databases were used to search for articles published from 2016–2024.
Brief description of the state of knowledge:
Drugs such as benzoyl peroxide, antibiotics, photodynamic therapy, and retinoids, cause clinical improvement of acne in patients and reduce the population of Cutibacterium acnes, but their influence on the diversity of the microbiota is different. A major problem today is the increase in bacterial resistance to antibiotics. As a result, new generation antibiotics have been created, which can be an effective tool in the fight against resistance. Currently, probiotics can be added to conventional therapy, some of which, e.g. PEG-8 Laurate, have a synergistic effect with other forms of treatment. Moreover, probiotics are becoming a promising form of treatment, modifying intestinal and skin microflora, impacting immune function, and restoring balance.
Summary:
Acne treatment significantly alters the composition of the human microbiota, which is why it is important to restore the natural composition of the microbiota in the treatment of this disease. Therefore, treatment options should be sought that will change the composition of the microbiota towards that of healthy people
REFERENCES (49)
1.
Mohsin N, Hernandez LE, Martin MR, et al. Acne treatment review and future perspectives. Dermatol Ther. 2022;35(9):e15719. https://doi.org/10.1111/dth.15....
2.
Dessinioti C, Katsambas A. The Microbiome and Acne: Perspectives for Treatment. Dermatol Ther (Heidelb). 2024;14(1):31–44. https://doi.org/10.1007/s13555....
3.
Siddiqui R, Makhlouf Z, Khan NA. The increasing importance of the gut microbiome in acne vulgaris. Folia Microbiol (Praha). 2022;67(6):825–835. https://doi.org/10.1007/s12223....
4.
Nast A, Dréno B, Bettoli V, et al. European evidence-based (S3) guideline for the treatment of acne – update 2016 – short version. J Eur Acad Dermatol Venereol. 2016;30(8):1261–1268. https://doi.org/10.1111/jdv.13....
5.
Xu J, Mavranezouli I, Kuznetsov L, et al. Guideline Committee. Management of acne vulgaris: summary of NICE guidance. BMJ. 2021;374:n1800. https://doi.org/10.1136/bmj.n1....
6.
Chilicka K, Dzieńdziora-Urbińska I, Szyguła R, et al. Microbiome and Probiotics in Acne Vulgaris-A Narrative Review. Life (Basel). 2022;12(3):422. https://doi.org/10.3390/life12....
7.
Xu H, Li H. Acne, the Skin Microbiome, and Antibiotic Treatment. Am J Clin Dermatol. 2019;20(3):335–344. https://doi.org/10.1007/s40257....
8.
Dreno B, Dekio I, Baldwin H, et al. Acne microbiome: From phyla to phylotypes. J Eur Acad Dermatol Venereol. 2024;38(4):657–664. https://doi.org/10.1111/jdv.19....
9.
Dréno B, Dagnelie MA, Khammari A, et al. The Skin Microbiome: A New Actor in Inflammatory Acne. Am J Clin Dermatol. 2020;21(Suppl 1):18–24. https://doi.org/10.1007/s40257....
10.
Lee YB, Byun EJ, Kim HS. Potential Role of the Microbiome in Acne: A Comprehensive Review. J Clin Med. 2019;8(7):987. https://doi.org/10.3390/jcm807....
11.
Ellis SR, Nguyen M, Vaughn AR, et al. The Skin and Gut Microbiome and Its Role in Common Dermatologic Conditions. Microorganisms. 2019;7(11):550. https://doi.org/10.3390/microo....
12.
Mahmud MR, Akter S, Tamanna SK, et al. Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut Microbes. 2022;14(1):2096995. https://doi.org/10.1080/194909....
13.
Huang C, Zhuo F, Han B, et al. The updates and implications of cutaneous microbiota in acne. Cell Biosci. 2023;13(1):113. https://doi.org/10.1186/s13578....
14.
Zhou L, Chen L, Liu X, et al. The influence of benzoyl peroxide on skin microbiota and the epidermal barrier for acne vulgaris. Dermatol Ther. 2022;35(3):e15288. https://doi.org/10.1111/dth.15....
15.
Thompson KG, Rainer BM, Antonescu C, et al. Minocycline and Its Impact on Microbial Dysbiosis in the Skin and Gastrointestinal Tract of Acne Patients. Ann Dermatol. 2020;32(1):21–30. https://doi.org/10.5021/ad.202....
16.
Guo Y, Zeng M, Yuan Y, et al. Photodynamic therapy treats acne by altering the composition of the skin microbiota. Skin Res Technol. 2023;29(1):e13269. https://doi.org/10.1111/srt.13....
17.
Tao S, Wang Z, Quan C, et al. The effects of ALA-PDT on microbiota in pilosebaceous units of patients with severe acne: A metagenomic study. Photodiagnosis Photodyn Ther. 2021;33:102050. https://doi.org/10.1016/j.pdpd....
18.
Kelhälä HL, Aho VTE, Fyhrquist N, et al. Isotretinoin and lymecycline treatments modify the skin microbiota in acne. Exp Dermatol. 2018;27(1):30–36. https://doi.org/10.1111/exd.13....
19.
Pécastaings S, Roques C, Nocera T, et al. Characterisation of Cutibacterium acnes phylotypes in acne and in vivo exploratory evaluation of Myrtacine®. J Eur Acad Dermatol Venereol. 2018;32 Suppl 2:15–23. https://doi.org/10.1111/jdv.15....
20.
Shao X, Chen Y, Zhang L, et al. Effect of 30% Supramolecular Salicylic Acid Peel on Skin Microbiota and Inflammation in Patients with Moderate-to-Severe Acne Vulgaris. Dermatol Ther (Heidelb). 2023;13(1):155–168. https://doi.org/10.1007/s13555....
21.
Bilal H, Xiao Y, Khan MN, et al. Stabilization of Acne Vulgaris-Associated Microbial Dysbiosis with 2% Supramolecular Salicylic Acid. Pharmaceuticals (Basel). 2023;16(1):87. https://doi.org/10.3390/ph1601....
22.
Coughlin CC, Swink SM, Horwinski J, et al. The preadolescent acne microbiome: A prospective, randomized, pilot study investigating characterization and effects of acne therapy. Pediatr Dermatol. 2017;34(6):661–664. https://doi.org/10.1111/pde.13....
23.
Ahluwalia J, Borok J, Haddock ES, et al. The microbiome in preadolescent acne: Assessment and prospective analysis of the influence of benzoyl peroxide. Pediatr Dermatol. 2019;36(2):200–206. https://doi.org/10.1111/pde.13....
24.
Chien AL, Tsai J, Leung S, et al. Association of Systemic Antibiotic Treatment of Acne With Skin Microbiota Characteristics. JAMA Dermatol. 2019;155(4):425–434. https://doi.org/10.1001/jamade....
25.
Park SY, Kim HS, Lee SH, et al. Characterization and Analysis of the Skin Microbiota in Acne: Impact of Systemic Antibiotics. J Clin Med. 2020;9(1):168. https://doi.org/10.3390/jcm901....
26.
Nolan ZT, Banerjee K, Cong Z, et al. Treatment response to isotretinoin correlates with specific shifts in Cutibacterium acnes strain composition within the follicular microbiome. Exp Dermatol. 2023;32(7):955–964. https://doi.org/10.1111/exd.14....
27.
McCoy WH 4th, Otchere E, Rosa BA, et al. Skin Ecology during Sebaceous Drought-How Skin Microbes Respond to Isotretinoin. J Invest Dermatol. 2019;139(3):732–735. https://doi.org/10.1016/j.jid.....
28.
Salmanian M, Shirbeigi L, Hashem-Dabaghian F, et al. The Effects of Myrtle (Myrtus communis) and Clindamycin Topical Solution in the Treatment of Mild to Moderate Acne Vulgaris: A Comparative Split-Face Study. J Pharmacopuncture. 2020;23(4):220–229. https://doi.org/10.3831/kpi.20....
29.
Clark AK, Haas KN, Sivamani RK. Edible Plants and Their Influence on the Gut Microbiome and Acne. Int J Mol Sci. 2017;18(5):1070. Published 2017 May 17. https://doi.org/10.3390/ijms18....
30.
Nascimento T, Gomes D, Simões R, et al. Tea Tree Oil: Properties and the Therapeutic Approach to Acne-A Review. Antioxidants (Basel). 2023;12(6):1264. Published 2023 Jun 12. https://doi.org/10.3390/antiox....
31.
Dontje AEWK, Schuiling-Veninga CCM, van Hunsel FPAM, et al. The Therapeutic Potential of Essential Oils in Managing Inflammatory Skin Conditions: A Scoping Review. Pharmaceuticals (Basel). 2024;17(5):571. Published 2024 Apr 29. https://doi.org/10.3390/ph1705....
32.
Najafi-Taher R, Jafarzadeh Kohneloo A, Eslami Farsani V, et al. A topical gel of tea tree oil nanoemulsion containing adapalene versus adapalene marketed gel in patients with acne vulgaris: a randomized clinical trial. Arch Dermatol Res. 2022;314(7):673–679. https://doi.org/10.1007/s00403....
33.
Matias M, Pinteus S, Martins A, et al. Gelidiales Are Not Just Agar-Revealing the Antimicrobial Potential of Gelidium corneum for Skin Disorders. Antibiotics (Basel). 2022;11(4):481. Published 2022 Apr 5. https://doi.org/10.3390/antibi....
34.
Tollenaere M, Boira C, Chapuis E, et al. Action of Mangifera indica Leaf Extract on Acne-Prone Skin through Sebum Harmonization and Targeting C. acnes. Molecules. 2022;27(15):4769. Published 2022 Jul 26. https://doi.org/10.3390/molecu....
35.
Kurek-Górecka A, Górecki M, Rzepecka-Stojko A, et al. Bee Products in Dermatology and Skin Care. Molecules. 2020; 25(3):556. https://doi.org/10.3390/molecu....
36.
Batra R, Sadhasivam S, Saini S, et al. Efficacy and Safety of VB-1953 Topical Gel in Non-Responder Acne Patients with Clindamycin-Resistant Cutibacterium acnes. Drugs R D. 2020;20(2):95–104. https://doi.org/10.1007/s40268....
37.
Han HS, Shin SH, Choi BY, et al. A split face study on the effect of an anti-acne product containing fermentation products of Enterococcus faecalis CBT SL-5 on skin microbiome modification and acne improvement [published correction appears in J Microbiol. 2022 Jul;60(7):766.]. J Microbiol. 2022;60(5):488–495. https://doi.org/10.1007/s12275....
38.
Sánchez-Pellicer P, Navarro-Moratalla L, Núñez-Delegido E, et al. Acne, Microbiome, and Probiotics: The Gut-Skin Axis. Microorganisms. 2022;10(7):1303. https://doi.org/10.3390/microo....
39.
Chae M, Kim BJ, Na J, et al. Antimicrobial activity of Lactiplantibacillus plantarum APsulloc 331261 and APsulloc 331266 against pathogenicskin microbiota. Front Biosci (Elite Ed). 2021;13(2):237–248. https://doi.org/10.52586/e881.
40.
Espinoza-Monje M, Campos J, Alvarez Villamil E, et al. Characterization of Weissella viridescens UCO-SMC3 as a Potential Probiotic for the Skin: Its Beneficial Role in the Pathogenesis of Acne Vulgaris. Microorganisms. 2021;9(7):1486. https://doi.org/10.3390/microo....
41.
Rahmayani T, Putra IB, Jusuf NK. The Effect of Oral Probiotic on the Interleukin-10 Serum Levels of Acne Vulgaris. Open Access Maced J Med Sci. 2019;7(19):3249–3252. https://doi.org/10.3889/oamjms....
42.
Rinaldi F, Marotta L, Mascolo A, et al. Facial Acne: A Randomized, Double-Blind, Placebo-Controlled Study on the Clinical Efficacy of a Symbiotic Dietary Supplement. Dermatol Ther (Heidelb). 2022;12(2):577–589. https://doi.org/10.1007/s13555....
43.
Kim J, Kim H, Jeon S, et al. Synergistic Antibacterial Effects of Probiotic Lactic Acid Bacteria with Curcuma longa Rhizome Extract as Synbiotic against Cutibacterium acnes. Appl. Sci. 2020;10:8955. https://doi.org/10.3390/app102....
44.
Marito S, Keshari S, Huang CM. PEG-8 Laurate Fermentation of Staphylococcus epidermidis Reduces the Required Dose of Clindamycin Against Cutibacterium acnes. Int J Mol Sci. 2020;21(14):5103. https://doi.org/10.3390/ijms21....
45.
Podrini C, Schramm L, Marianantoni G, et al. Topical Administration of Lactiplantibacillus plantarum (SkinDuoTM) Serum Improves Anti-Acne Properties. Microorganisms. 2023;11(2):417. https://doi.org/10.3390/microo....
46.
Sathikulpakdee S, Kanokrungsee S, Vitheejongjaroen P, et al. Efficacy of probiotic-derived lotion from Lactobacillus paracasei MSMC 39-1 in mild to moderate acne vulgaris, randomized controlled trial. J Cosmet Dermatol. 2022;21(10):5092–5097. https://doi.org/10.1111/jocd.1....
47.
AOBiome therapeutics reports positive efficacy results from phase 2b clinical trial of ammonia oxidizing bacteria (AOB) for the treatment of acne vulgaris. AOBiome Therapeutics https://www.aobiome.com/pressr... (access: 2024.10.15).
48.
Tsai WH, Chou CH, Chiang YJ, et al. Regulatory effects of Lactobacillus plantarum-GMNL6 on human skin health by improving skin microbiome. Int J Med Sci. 2021;18(5):1114–1120. https://doi.org/10.7150/ijms.5....
49.
Liang L, Qi X, Jiang X, et al. Lactobacillus plantarum MH-301 as an effective adjuvant to isotretinoin in the treatment of acne vulgaris: a randomized and open-label trail. Front Med (Lausanne). 2024;10:1340068. https://doi.org/10.3389/fmed.2....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.