Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Non-pharmacological interventions for gait rehabilitation in children with neurodisability – A bibliometric and visualization analysis
1
Department of Physical Culture, Gdansk University of Physical Education and Sport, Poland
Corresponding author
hongli yu
Department of Physical Culture, University of Physical Education and Sport, Gdańsk, Poland
Department of Physical Culture, University of Physical Education and Sport, Gdańsk, Poland
KEYWORDS
gaitphysical therapyDown syndromecerebral palsybibliometric analysisnon-pharmacological interventionsneurodisability
TOPICS
ABSTRACT
Introduction and objective:
Gait impairments significantly impact the daily active participation and quality of life in children with neurodisabilities. Non-pharmacological interventions (NPIs) have demonstrated positive outcomes in gait rehabilitation, although comprehensive analyses that map the global research landscape in this domain are limited. The aim of the bibliometric review is to systematically explore and visualize global research trends, identify hotspots, and highlight emerging themes related to NPIs for gait rehabilitation in children with neurodisability. The literature coverage spans 1993–2024.
Review methods:
Literature was collected from the Web of Science Core Collection using the keywords “cerebral palsy,” “rehabilitation,” and “gait,” and was systematically analyzed.
Brief description of the state of knowledge:
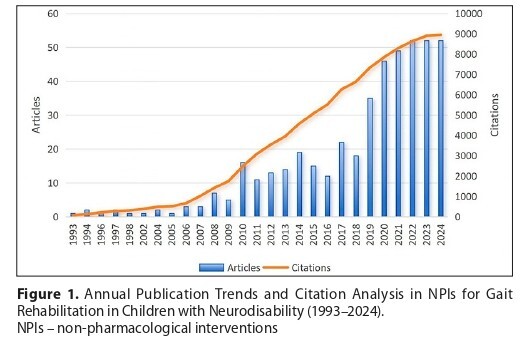
A total of 455 relevant documents were included. The number of studies has steadily increased from 1993 to 2024 in this field. The United States leads in terms of publication volume and cumulative citations, with Developmental Medicine & Child Neurology published the highest number of papers in this area. Emerging technologies such as exoskeletons, virtual reality and robot-assisted gait training have become research hotspots.
Results:
The findings of the study provide researchers and clinicians with a clear, objective understanding of the current state and future directions in this important area of research.
Summary:
The study visually represented research trends on the NPIs in gait rehabilitation for children with neurodisability, revealed emerging patterns of research and areas of focus.
Gait impairments significantly impact the daily active participation and quality of life in children with neurodisabilities. Non-pharmacological interventions (NPIs) have demonstrated positive outcomes in gait rehabilitation, although comprehensive analyses that map the global research landscape in this domain are limited. The aim of the bibliometric review is to systematically explore and visualize global research trends, identify hotspots, and highlight emerging themes related to NPIs for gait rehabilitation in children with neurodisability. The literature coverage spans 1993–2024.
Review methods:
Literature was collected from the Web of Science Core Collection using the keywords “cerebral palsy,” “rehabilitation,” and “gait,” and was systematically analyzed.
Brief description of the state of knowledge:
A total of 455 relevant documents were included. The number of studies has steadily increased from 1993 to 2024 in this field. The United States leads in terms of publication volume and cumulative citations, with Developmental Medicine & Child Neurology published the highest number of papers in this area. Emerging technologies such as exoskeletons, virtual reality and robot-assisted gait training have become research hotspots.
Results:
The findings of the study provide researchers and clinicians with a clear, objective understanding of the current state and future directions in this important area of research.
Summary:
The study visually represented research trends on the NPIs in gait rehabilitation for children with neurodisability, revealed emerging patterns of research and areas of focus.
REFERENCES (50)
1.
Gardiner E, Wong V, Lin G, Miller AR. Terminology and descriptions of navigation and related practices for children with neurodisability and their families: a scoping review. BMC Health Serv Res. 2022;22(1):214. Published 2022 Feb 17. doi:10.1186/s12913-022-07617-y.
2.
Morris C, Janssens A, Tomlinson R, et al. Towards a definition of neurodisability: a Delphi survey. Dev Med Child Neurol. 2013;55(12):1103–1108. doi:10.1111/dmcn.12218.
3.
World Health Organization. Package of Interventions for Rehabilitation: Module 5: Neurodevelopmental Disorders. Geneva, Switzerland: World Health Organization; 2023. Accessed December 11, 2024. https://www.who.int/publicatio....
4.
World Health Organization. Package of interventions for rehabilitation: module 5: neurodevelopmental disorders: web annex: literature reviews and evidence tables. Geneva, Switzerland: World Health Organization; 2023. ISBN 9789240071216.
5.
Oxelgren UW, Myrelid Å, Annerén G, et al. Prevalence of autism and attention-deficit-hyperactivity disorder in Down syndrome: a population-based study. Dev Med Child Neurol. 2017;59(3):276–283. doi:10.1111/dmcn.13217.
6.
Craig F, Savino R, Trabacca A. A systematic review of comorbidity between cerebral palsy, autism spectrum disorders and Attention Deficit Hyperactivity Disorder. Eur J Paediatr Neurol. 2019;23(1):31–42. doi:10.1016/j.ejpn.2018.10.005.
7.
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2133–2161. doi:10.1016/S0140-6736(24)00757-8.
8.
Global Research on Developmental Disabilities Collaborators. Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Glob Health. 2018;6(10):e1100-e1121. doi:10.1016/S2214-109X(18)30309-7. Published correction in: Lancet Glob Health. 2018;6(12):e1287. doi:10.1016/S2214-109X(18)30443-1.
9.
Stallings EB, Isenburg JL, Rutkowski RE, et al. National population-based estimates for major birth defects, 2016–2020. Birth Defects Res. 2024;116(1):e2301. doi:10.1002/bdr2.2301.
10.
McIntyre S, Goldsmith S, Webb A, et al. Global prevalence of cerebral palsy: A systematic analysis. Dev Med Child Neurol. 2022;64(12):1494–1506. doi:10.1111/dmcn.15346.
11.
Petrou S, Johnson S, Wolke D, Marlow N. The association between neurodevelopmental disability and economic outcomes during mid-childhood. Child Care Health Dev. 2013;39(3):345–357. doi:10.1111/j.1365-2214.2012.01368.x.
12.
Schlaggar BL, Mink JW. Movement disorders in children. Pediatr Rev. 2003;24(2):39–51. doi:10.1542/pir.24-2-39.
13.
Colizzi M, Ciceri ML, Di Gennaro G, et al. Investigating Gait, Movement, and Coordination in Children with Neurodevelopmental Disorders: Is There a Role for Motor Abnormalities in Atypical Neurodevelopment?. Brain Sci. 2020;10(9):601. Published 2020 Sep 2. doi:10.3390/brainsci10090601.
14.
Hallemans A, Verbeque E, Van de Walle P. Motor functions. Handb Clin Neurol. 2020;173:157–170. doi:10.1016/B978-0-444-64150-2.00015-0.
15.
Teka WW, Hamade KC, Barnett WH, et al. From the motor cortex to the movement and back again. PLoS One. 2017;12(6):e0179288. Published 2017 Jun 20. doi:10.1371/journal.pone.0179288.
16.
Verschuren O, Peterson MD, Balemans AC, Hurvitz EA. Exercise and physical activity recommendations for people with cerebral palsy. Dev Med Child Neurol. 2016;58(8):798–808. doi:10.1111/dmcn.13053.
17.
Rosenberg L, Moran A, Bart O. The associations among motor ability, social-communication skills, and participation in daily life activities in children with low-functioning autism spectrum disorder. J Occup Ther Sch Early Interv. 2017;10(2):137–146. doi:10.1080/19411243.2017.1304842.
18.
Farran EK, Bowler A, Karmiloff-Smith A, et al. Cross-Domain Associations Between Motor Ability, Independent Exploration, and Large-Scale Spatial Navigation; Attention Deficit Hyperactivity Disorder, Williams Syndrome, and Typical Development. Front Hum Neurosci. 2019;13:225. Published 2019 Jul 3. doi:10.3389/fnhum.2019.00225.
19.
WHO Multicentre Growth Reference Study Group. WHO Motor Development Study: windows of achievement for six gross motor development milestones. Acta Paediatr Suppl. 2006;450:86–95. doi:10.1111/j.1651-2227.2006.tb02379.x.
20.
Shamel S, Zarkesh MR. Recent challenges in children’s developmental milestones. Pediatr Res. Published online December 16, 2024. doi:10.1038/s41390-024-03781-5.
21.
Kwan C, Gitimoghaddam M, Collet JP. Effects of Social Isolation and Loneliness in Children with Neurodevelopmental Disabilities: A Scoping Review. Brain Sci. 2020;10(11):786. Published 2020 Oct 28. doi:10.3390/brainsci10110786.
22.
Candiri BA, Arıkan AN, Çolak SC. Balance and physical activity in children with neurodevelopmental disorders. In: Bilgili A, editor. Current Researches in Health Sciences-III. Ankara, Turkey: Özgür Yayınları; 2023:117. doi:10.58830/ozgur.pub305.c1255.
23.
Chouksey A, Pandey S. Functional Movement Disorders in Children. Front Neurol. 2020;11:570151. Published 2020 Nov 12. doi:10.3389/fneur.2020.570151.
24.
Hilfiker R, Meichtry A, Eicher M, et al. Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: a systematic review incorporating an indirect-comparisons meta-analysis. Br J Sports Med. 2018;52(10):651–658. doi:10.1136/bjsports-2016-096422.
25.
Catalá-López F, Hutton B, Núñez-Beltrán A, et al. The pharmacological and non-pharmacological treatment of attention deficit hyperactivity disorder in children and adolescents: A systematic review with network meta-analyses of randomised trials. PLoS One. 2017;12(7):e0180355. Published 2017 Jul 12. doi:10.1371/journal.pone.0180355.
26.
Tao R, Yang Y, Wilson M, et al. Comparative effectiveness of physical activity interventions on cognitive functions in children and adolescents with Neurodevelopmental Disorders: a systematic review and network meta-analysis of randomized controlled trials. Int J Behav Nutr Phys Act. 2025;22(1):6. Published 2025 Jan 13. doi:10.1186/s12966-024-01702-7.
27.
Meza N, Rojas V, Escobar Liquitay CME, et al. Non-pharmacological interventions for autism spectrum disorder in children: an overview of systematic reviews. BMJ Evid Based Med. 2023;28(4):273–282. doi:10.1136/bmjebm-2021-111811.
28.
Hocking DR, Farhat H, Gavrila R, et al. Do Active Video Games Improve Motor Function in People With Developmental Disabilities? A Meta-analysis of Randomized Controlled Trials. Arch Phys Med Rehabil. 2019;100(4):769–781. doi:10.1016/j.apmr.2018.10.021.
29.
Méndez-Martínez M, Rodríguez-Grande EI. Effects of therapeutic exercise on the motor function of adults with Down syndrome: a systematic review and meta-analysis. Sci Rep. 2023;13(1):21962. Published 2023 Dec 11. doi:10.1038/s41598-023-48179-1.
30.
Short AD, Chen H, Hulks V, Scerif G. Non‑pharmacological interventions targeting motor difficulties in neurodivergent children: a systematic review. Neurodiversity. 2025;3:1–25. doi:10.1177/27546330241310175.
31.
Phadke V, Sharma R, Sharma N, Mitra S. Global Research Trends on Gait Rehabilitation in Individuals With Spinal Cord Injury- A Bibliometric Analysis. Global Spine J. 2024;14(8):2408–2419. doi:10.1177/21925682241243074.
32.
Mikolajczyk T, Ciobanu I, Badea DI, et al. Advanced technology for gait rehabilitation: an overview. Adv Mech Eng. 2018;10(7):1–19. doi:10.1177/1687814018783627.
33.
Montazeri A, Mohammadi S, Hesari PM, Ghaemi M, Riazi H, Sheikhi-Mobarakeh Z. Preliminary guideline for reporting bibliometric reviews of the biomedical literature (BIBLIO): a minimum requirements. Syst Rev. 2023;12(1):239. doi:10.1186/s13643-023-02410-2.
34.
Donthu N, Kumar S, Mukherjee D, Pandey N, Lim WM. How to conduct a bibliometric analysis: an overview and guidelines. J Bus Res. 2021;133:285–296. doi:10.1016/j.jbusres.2021.04.070.
35.
Mongeon P, Paul-Hus A. The journal coverage of Web of Science and Scopus: a comparative analysis. Scientometrics. 2016;106(1):213–228. doi:10.1007/s11192-015-1765-5.
36.
Aslam A, editor. The State of the World’s Children 2013: Children with Disabilities. New York, NY: United Nations Children’s Fund (UNICEF); 2013.
37.
World Health Organization. Developmental Difficulties in Early Childhood: Prevention, Early Identification, Assessment and Intervention in Low- and Middle-Income Countries. Geneva, Switzerland: World Health Organization; 2012.
38.
Boyd RN, Jordan R, Pareezer L, et al. Australian Cerebral Palsy Child Study: protocol of a prospective population based study of motor and brain development of preschool aged children with cerebral palsy. BMC Neurol. 2013;13:57. Published 2013 Jun 11. doi:10.1186/1471-2377-13-57.
39.
Sakzewski L, Pool D, Armstrong E, et al. ACTIVE STRIDES-CP: protocol for a randomised trial of intensive rehabilitation (combined intensive gait and cycling training) for children with moderate-to-severe bilateral cerebral palsy. BMJ Open. 2023;13(3):e068774. Published 2023 Mar 29. doi:10.1136/bmjopen-2022-068774.
40.
Booth ATC, Buizer AI, Meyns P, et al. The efficacy of functional gait training in children and young adults with cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2018;60(9):866–883. doi:10.1111/dmcn.13708.
41.
Moreau NG, Bodkin AW, Bjornson K, et al. Effectiveness of Rehabilitation Interventions to Improve Gait Speed in Children With Cerebral Palsy: Systematic Review and Meta-analysis. Phys Ther. 2016;96(12):1938–1954. doi:10.2522/ptj.20150401.
42.
Chen Y, Fanchiang HD, Howard A. Effectiveness of Virtual Reality in Children With Cerebral Palsy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phys Ther. 2018;98(1):63–77. doi:10.1093/ptj/pzx107.
43.
Zago M, Duarte NAC, Grecco LAC, et al. Gait and postural control patterns and rehabilitation in Down syndrome: a systematic review. J Phys Ther Sci. 2020;32(4):303–314. doi:10.1589/jpts.32.303.
44.
Cai X, Qian G, Cai S, et al. The effect of whole-body vibration on lower extremity function in children with cerebral palsy: A meta-analysis. PLoS One. 2023;18(3):e0282604. Published 2023 Mar 10. doi:10.1371/journal.pone.0282604.
45.
Qian G, Cai X, Xu K, et al. Which gait training intervention can most effectively improve gait ability in patients with cerebral palsy? A systematic review and network meta-analysis. Front Neurol. 2023;13:1005485. Published 2023 Jan 10. doi:10.3389/fneur.2022.1005485.
46.
Qian G, Perzanowska E, Kozakiewicz M, et al. Immediate effects of Vojta Therapy on gait ability in down syndrome patients: a pilot study [published correction appears in Front Neurol. 2025 Apr 02;16:1591573. doi:10.3389/fneur.2025.1591573.]. Front Neurol. 2025;15:1511849. Published 2025 Jan 6. doi:10.3389/fneur.2024.1511849.
47.
Qian G, Perzanowska E, Wilczyńska D, et al. Exploring the impact of home-based Vojta therapy on gait performance in individuals with Down syndrome: a preliminary feasibility study. Front Neurol. 2025;16:1537635. Published 2025 Mar 11. doi:10.3389/fneur.2025.1537635.
48.
Llamas-Ramos R, Sánchez-González JL, Llamas-Ramos I. Robotic Systems for the Physiotherapy Treatment of Children with Cerebral Palsy: A Systematic Review. Int J Environ Res Public Health. 2022;19(9):5116. Published 2022 Apr 22. doi:10.3390/ijerph19095116.
49.
Diot CM, Youngblood JL, Friesen AH, et al. Robot-Assisted Gait Training with Trexo Home: Users, Usage and Initial Impacts. Children (Basel). 2023;10(3):437. Published 2023 Feb 24. doi:10.3390/children10030437.
50.
Mohd Iqbal HA, Zanudin A, Mohd Nordin NA. Motivational influence of virtual reality in physical therapy for children with cerebral palsy: a systematic review protocol. BMJ Open. 2025;15(1):e075912. Published 2025 Jan 7. doi:10.1136/bmjopen-2023-075912.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.