Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Sleep problems and related factors in rural and urban populations in Western Pomerania, Poland
1
Department of Humanities in Medicine, Pomeranian Medical University, Szczecin, Poland
Corresponding author
Weronika Wolińska
Department of Humanities in Medicine, Pomeranian Medical University, Szczecin, Chłapowskiego 11, 70-103, Szczecin, Poland
Department of Humanities in Medicine, Pomeranian Medical University, Szczecin, Chłapowskiego 11, 70-103, Szczecin, Poland
Ann Agric Environ Med. 2022;29(3):443-452
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Insomnia is considered the most common sleep disorder. Sleep deprivation, regardless of its causes, leads to deterioration in the quality of life (QoL), poorer daytime functioning, and reduced professional productivity. It also contributes to an increase in the number of occupational and road accidents. Most research on sleep problems has been conducted on samples of urban residents, with few studies among people living in rural areas, where high rates of sleep problems have also been recorded.
Objective:
The aim of the study was to determine sleep problems and their impact on the QoL of rural and urban residents of the West Pomeranian Province of Poland.
Material and methods:
The study involved 597 people: 187 (31.32%) rural and 410 (68.68%) urban residents. The research instruments used in the study were standardized questionnaires, namely the Athens Insomnia Scale (AIS), Insomnia Severity Index (ISI), Epworth Sleepiness Scale (ESS), and the Short Form 36 Health Survey (SF-36), and the author’s questionnaire concerning socio-demographic data.
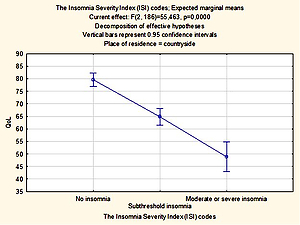
Results:
There was a statistically significant relationship between insomnia and gender, both among rural (p < 0.050) and urban (p < 0.005) residents. Diseases that turned out to be significantly related to insomnia in rural residents were diabetes (p < 0.045) and depression (p < 0.015). Women living in the city assessed their QoL worse than men (p < 0.0005). The lowest QoL was demonstrated in people with insomnia.
Conclusions:
The results suggest that insomnia is often a permanent condition in the Polish population. Bearing in mind the prevalence of insomnia among Poles, especially in the 60–79 age group, it is necessary to introduce obligatory tests of sleep disorders and QoL into the practice of a family doctor, due to the long-term adverse effects of persistent insomnia.
Insomnia is considered the most common sleep disorder. Sleep deprivation, regardless of its causes, leads to deterioration in the quality of life (QoL), poorer daytime functioning, and reduced professional productivity. It also contributes to an increase in the number of occupational and road accidents. Most research on sleep problems has been conducted on samples of urban residents, with few studies among people living in rural areas, where high rates of sleep problems have also been recorded.
Objective:
The aim of the study was to determine sleep problems and their impact on the QoL of rural and urban residents of the West Pomeranian Province of Poland.
Material and methods:
The study involved 597 people: 187 (31.32%) rural and 410 (68.68%) urban residents. The research instruments used in the study were standardized questionnaires, namely the Athens Insomnia Scale (AIS), Insomnia Severity Index (ISI), Epworth Sleepiness Scale (ESS), and the Short Form 36 Health Survey (SF-36), and the author’s questionnaire concerning socio-demographic data.
Results:
There was a statistically significant relationship between insomnia and gender, both among rural (p < 0.050) and urban (p < 0.005) residents. Diseases that turned out to be significantly related to insomnia in rural residents were diabetes (p < 0.045) and depression (p < 0.015). Women living in the city assessed their QoL worse than men (p < 0.0005). The lowest QoL was demonstrated in people with insomnia.
Conclusions:
The results suggest that insomnia is often a permanent condition in the Polish population. Bearing in mind the prevalence of insomnia among Poles, especially in the 60–79 age group, it is necessary to introduce obligatory tests of sleep disorders and QoL into the practice of a family doctor, due to the long-term adverse effects of persistent insomnia.
REFERENCES (56)
1.
Schlack R, Hapke U, Maske U, et al. Häufigkeit und Verteilung von Schlafproblemen und Insomnie in der deutschen Erwachsenenbevölkerung: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1) [Frequency and distribution of sleep problems and insomnia in the adult population in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS1)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56(5–6):740–748. doi:10.1007/s00103-013-1689-2.
2.
Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700. doi:10.1111/jsr.12594.
3.
Machado AKF, Wendt A, Wehrmeister FC. Sleep problems and associated factors in a rural population of a Southern Brazilian city. Rev Saude Publica. 2018 Sep 13;52(Suppl 1):5s. doi: 10.11606/S1518-8787.2018052000260.
4.
Morin CM, Jarrin DC, Ivers H, et al. Incidence, Persistence, and Remission Rates of Insomnia Over 5 Years. JAMA Netw Open. 2020;3(11):e2018782. doi:10.1001/jamanetworkopen.2020.18782.
5.
Nowicki Z, Grabowski K, Cubała WJ, et al. Rozpowszechnienie subiektywnej bezsenności w populacji polskiej. Psychiatr Pol. 2016; 50(1): 165–17. http://dx.doi.org/10.12740/PP/....
6.
Siemiński M, Skorupa Ł, Wiśniewska-Skorupa K. Diagnostics and therapy of insomnia in general practice Part I: Epidemiology, pathomechanism and diagostics of insomnia. Varia Medica. 2019;3(2); 109–115.
7.
Bjorvatn B, Jernelöv S, Pallesen S. Insomnia – A Heterogenic Disorder Often Comorbid With Psychological and Somatic Disorders and Diseases: A Narrative Review With Focus on Diagnostic and Treatment Challenges. Front Psychol. 2021;12:639198. doi:10.3389/fpsyg.2021.639198.
8.
Yamamoto K, Motokawa K, Yoshizaki T, et al. Association of Dietary Variety and Appetite with Sleep Quality in Urban-Dwelling Older Japanese Adults. J Nutr Health Aging. 2020;24(2):152–159. doi:10.1007/s12603-019-1297-4.
9.
Suh S, Cho N, Zhang J. Sex Differences in Insomnia: from Epidemiology and Etiology to Intervention. Curr Psychiatry Rep. 2018;20(9):69. doi:10.1007/s11920-018-0940-9.
10.
Paunio T, Korhonen T, Hublin C, et al. Poor sleep predicts symptoms of depression and disability retirement due to depression. J Affect Disord. 2015;172:381–389. doi:10.1016/j.jad.2014.10.002.
11.
National center on sleep disorders research, et al. National institutes of health sleep disorders research plan. Bethesda, MD: National Institutes of Health, 2011. https://www.nhlbi.nih.gov/file... (access: 2021.12.12).
12.
Leger D, Guilleminault C, Dreyfus JP, et al. Prevalence of insomnia in a survey of 12,778 adults in France. J Sleep Res. 2000;9(1):35–42. doi:10.1046/j.1365-2869.2000.00178.x.
13.
Léger D, Poursain B, Neubauer D, et al. An international survey of sleeping problems in the general population. Curr Med Res Opin. 2008;24(1):307–317. doi:10.1185/030079907x253771.
14.
Yang JJ, Cai H, Xia L, et al. The Prevalence of Depressive and Insomnia Symptoms, and Their Association With Quality of Life Among Older Adults in Rural Areas in China. Front Psychiatry. 2021;12:727939. doi:10.3389/fpsyt.2021.727939.
15.
Ju YJ, Lee JE, Choi DW, et al. Association between perceived environmental pollution and poor sleep quality: results from nationwide general population sample of 162,797 people. Sleep Med. 2021;80:236–243. doi:10.1016/j.sleep.2021.01.043.
16.
Li J, Yao YS, Dong Q, et al. Characterization and factors associated with sleep quality among rural elderly in China. Arch Gerontol Geriatr. 2013;56(1):237–243. doi:10.1016/j.archger.2012.08.002.
17.
Hoefelmann LP, Lopes Ada S, da Silva KS, et al. Sociodemographic factors associated with sleep quality and sleep duration in adolescents from Santa Catarina, Brazil: what changed between 2001 and 2011?. Sleep Med. 2013;14(10):1017–1023. doi:10.1016/j.sleep.2013.05.015.
18.
Hartz AJ, Daly JM, Kohatsu ND, et al. Risk factors for insomnia in a rural population. Ann Epidemiol. 2007;17(12):940–947. doi:10.1016/j.annepidem.2007.07.097.
19.
Baldwin CM, Griffith KA, Nieto FJ, et al. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep. 2001;24(1):96–105. doi:10.1093/sleep/24.1.96.
20.
Kaur H, Spurling BC, Bollu PC. Chronic Insomnia. In: StatPearls. Treasure Island (FL): StatPearls 2022.
21.
Léger D, Scheuermaier K, Philip P, et al. SF-36: evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosom Med. 2001;63(1):49–55. doi:10.1097/00006842-200101000-00006.
22.
Sirajudeen MS, Dilshad Manzar M, Alqahtani M, et al. Psychometric Properties of the Athens Insomnia Scale in Occupational Computer Users. Healthcare (Basel). 2020;8(2):89. doi:10.3390/healthcare8020089.
23.
Sattler S, Seddig D, Zerbini G. Assessing sleep problems and daytime functioning: a translation, adaption, and validation of the Athens Insomnia Scale for non-clinical application (AIS-NCA). Psychol Health. 2021;1–26. doi:10.1080/08870446.2021.1998498.
24.
Manzar MD, Albougami A, Hassen HY, et al. Psychometric Validation of the Athens Insomnia Scale Among Nurses: A Robust Approach Using Both Classical Theory and Rating Scale Model Parameters. Nat Sci Sleep. 2022;14:725–739. doi:10.2147/NSS.S325220.
25.
Enomoto K, Adachi T, Yamada K, et al. Reliability and validity of the Athens Insomnia Scale in chronic pain patients. J Pain Res. 2018;11:793–801. doi:10.2147/JPR.S154852.
26.
Manzar MD, Jahrami HA, Bahammam AS. Structural validity of the Insomnia Severity Index: A systematic review and meta-analysis. Sleep Med Rev. 2021;60:101531. doi:10.1016/j.smrv.2021.101531.
27.
Mamun MA, Alimoradi Z, Gozal D, et al. Validating Insomnia Severity Index (ISI) in a Bangladeshi Population: Using Classical Test Theory and Rasch Analysis. Int J Environ Res Public Health. 2021;19(1):225. doi:10.3390/ijerph19010225.
28.
Lapin BR, Bena JF, Walia HK, et al. The Epworth Sleepiness Scale: Validation of One-Dimensional Factor Structure in a Large Clinical Sample. J Clin Sleep Med. 2018;14(8):1293–1301. doi:10.5664/jcsm.7258.
29.
Walker NA, Sunderram J, Zhang P, et al. Clinical utility of the Epworth sleepiness scale. Sleep Breath. 2020;24(4):1759–1765. doi:10.1007/s11325-020-02015-2.
30.
Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016;4:2050312116671725. doi:10.1177/2050312116671725.
31.
Arovah NI, Heesch KC. Verification of the Reliability and Validity of the Short Form 36 Scale in Indonesian Middle-aged and Older Adults. J Prev Med Public Health. 2020;53(3):180–188. doi:10.3961/jpmph.19.324.
32.
Mong JA, Cusmano DM. Sex differences in sleep: impact of biological sex and sex steroids. Philos Trans R Soc Lond B Biol Sci. 2016;371(1688):20150110. doi:10.1098/rstb.2015.0110.
33.
Ulander M, Rangtell F, Theorell-Haglöw J. Sleep Measurements in Women. Sleep Med Clin. 2021;16(4):635–648. doi:10.1016/j.jsmc.2021.07.004.
34.
Pengo MF, Won CH, Bourjeily G. Sleep in Women Across the Life Span. Chest. 2018;154(1):196–206. doi:10.1016/j.chest.2018.04.005.
35.
Doi Y, Minowa M, Tango T. Impact and correlates of poor sleep quality in Japanese white-collar employees. Sleep. 2003;26(4):467–471. doi:10.1093/sleep/26.4.467.
36.
Benbir G, Demir AU, Aksu M, et al. Prevalence of insomnia and its clinical correlates in a general population in Turkey. Psychiatry Clin Neurosci. 2015;69(9):543–552. doi:10.1111/pcn.12252.
37.
Beihl DA, Liese AD, Haffner SM. Sleep duration as a risk factor for incident type 2 diabetes in a multiethnic cohort. Ann Epidemiol. 2009;19(5):351–357. doi:10.1016/j.annepidem.2008.12.001.
38.
Kasperczyk J, Jośko J. Ocena rozpowszechnienia i uwarunkowań zaburzeń snu u pracowników zmianowych. Med Pr 2012; 63(5): 573–583.
39.
Lecca R, Puligheddu M, Acar GM, et al. Shift rotation scheme, sleepiness and sleep quality in night-shift workers. Occup Med (Lond). 2021;71(9):446–452. doi:10.1093/occmed/kqab139.
40.
Babiarczyk B, Bujok M. Występowanie zaburzeń snu wśród pielęgniarek pracujących w systemie zmianowym. Probl Hig Epidemiol. 2019;100(2): 89–94.
41.
Szymańska-Czechór M, Kędra E. Ocena wpływu pracy zmianowej na stan zdrowia personelu pielęgniarskiego wybranego podmiotu leczniczego – dane jakościowe (część II). Probl Pielęg 2017;25(3): 191–196.
42.
Kawalec A, Pawlas K. Czynniki środowiskowe wpływające na sen oraz zachowanie higieny snu. Probl Hig Epidemiol. 2013;94(1): 1–5.
43.
Żołnierczyk-Zreda D. Rodzaj umowy o pracę a zdrowie i funkcjonowanie zawodowe pracowników – przegląd badań. Med Pr. 2015; 66(4): 565–573.
44.
Liu RQ, Qian Z, Trevathan E, et al. Poor sleep quality associated with high risk of hypertension and elevated blood pressure in China: results from a large population-based study. Hypertens Res. 2016;39(1):54–59. doi:10.1038/hr.2015.98.
45.
Zhuang J, Zhan Y, Zhang F, et al. Self-reported insomnia and coronary heart disease in the elderly. Clin Exp Hypertens. 2016;38(1):51–55. doi:10.3109/10641963.2015.1060983.
46.
Ulmer CS, Bosworth HB, Germain A, et al. Associations between sleep difficulties and risk factors for cardiovascular disease in veterans and active duty military personnel of the Iraq and Afghanistan conflicts. J Behav Med. 2015;38(3):544–555. doi:10.1007/s10865-015-9627-4.
47.
Kołpa M, Grochowska A, Kubik B, et al. Lifestyle, metabolic compensation in patients with type 2 diabetes mellitus and the risk of chronic disease complications. Clin Diabetol. 2018; 7(3): 151–158. doi: 10.5603/DK.2018.0011.
48.
Lopes JM, Galvao FD, Oliveira AGRDC. Risk of Death in the Elderly with Excessive Daytime Sleepiness, Insomnia and Depression: Prospective Cohort Study in an Urban Population in Northeast Brazil. Risco de Morte em Idosos com Sonolencia Excessiva Diurna, Insônia e Depressao: Estudo de Coorte Prospectiva em Populaçao Urbana no Nordeste Brasileiro. Arq Bras Cardiol. 2021;117(3):446–454. doi:10.36660/abc.20200059.
49.
Krajewska O, Skrypnik K, Kręgielska-Narożna M, et al. Wpływ długości i jakości snu na parametry antropometryczne, metaboliczne i ogólny stan zdrowia fizycznego i psychicznego. Forum Zaburzeń Metabolicznych. 2017;8(2): 47–54.
50.
Sykut A, Ślusarska B, Jędrzejkiewicz B, et al. Zaburzenia snu jako powszechny problem społeczny wybrane uwarunkowania i konsekwencje zdowotne. Pielęgniarstwo XXI wieku. 2017;16(2): 53–57. doi: 10.1515/pielxxiw-2017-0019.
51.
Ishak WW, Bagot K, Thomas S, et al. Quality of life in patients suffering from insomnia. Innov Clin Neurosci. 2012;9(10):13–26.
52.
Liao W, Luo Z, Dong X, et al. Associations between depressive symptoms, anxiety symptoms, their comorbidity and health-related quality of life: a large-scale cross-sectional study. BMC Public Health. 2021;21(1):1911. doi:10.1186/s12889-021-11969-1.
53.
Scalo J, Desai P, Rascati K. Insomnia, hypnotic use, and health-related quality of life in a nationally representative sample. Qual Life Res. 2015;24(5):1223–1233. doi:10.1007/s11136-014-0842-1.
54.
Darchia N, Oniani N, Sakhelashvili I, et al. Relationship between Sleep Disorders and Health Related Quality of Life-Results from the Georgia SOMNUS Study. Int J Environ Res Public Health. 2018;15(8):1588. doi:10.3390/ijerph15081588.
55.
Kang N, Liu X, Liao W, et al. Health-related quality of life among rural adults with type 2 diabetes mellitus: a cross-sectional study. Eur J Public Health. 2021;31(3):547–553. doi:10.1093/eurpub/ckaa247.
56.
Kiejna A, Wojtyniak B, Rymaszewska J. Prevalence of insomnia in Poland results of National Health Interview Suvey. Acta Neuropsychiatrica. 2003; 15: 68–73.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.