Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Evaluation of the quality of life of older people with diabetes
1
ORPEA Polska Sp. z o.o.; Wrocław, Poland
2
Institute of Environmental Protection – National Research Institute, Warsaw, Poland
3
Faculty of Pedagogy and Psychology, Jan Kochanowski University, Kielce, Poland
4
Institute of Rural Health, Lublin, Poland
5
Collegium Medicum, Jan Kochanowski University, Kielce, Poland
6
Faculty of Public Health, Catholic University, Ružomberok, Slovakia
7
Department of Internal Nursing, Faculty of Health Sciences, Medical University, Wrocław, Poland
8
Faculty of Health and Physical Culture Sciences, Witelon Collegium State University, Legnica, Poland
Corresponding author
Ann Agric Environ Med. 2023;30(3):505-512
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Diabetes is commonly classified as a chronic disease of affluence due to the frequency of its incidence and the rate of its spreading. The aim of the study was to evaluate the quality of life of geriatric patients with type 2 diabetes.
Material and methods:
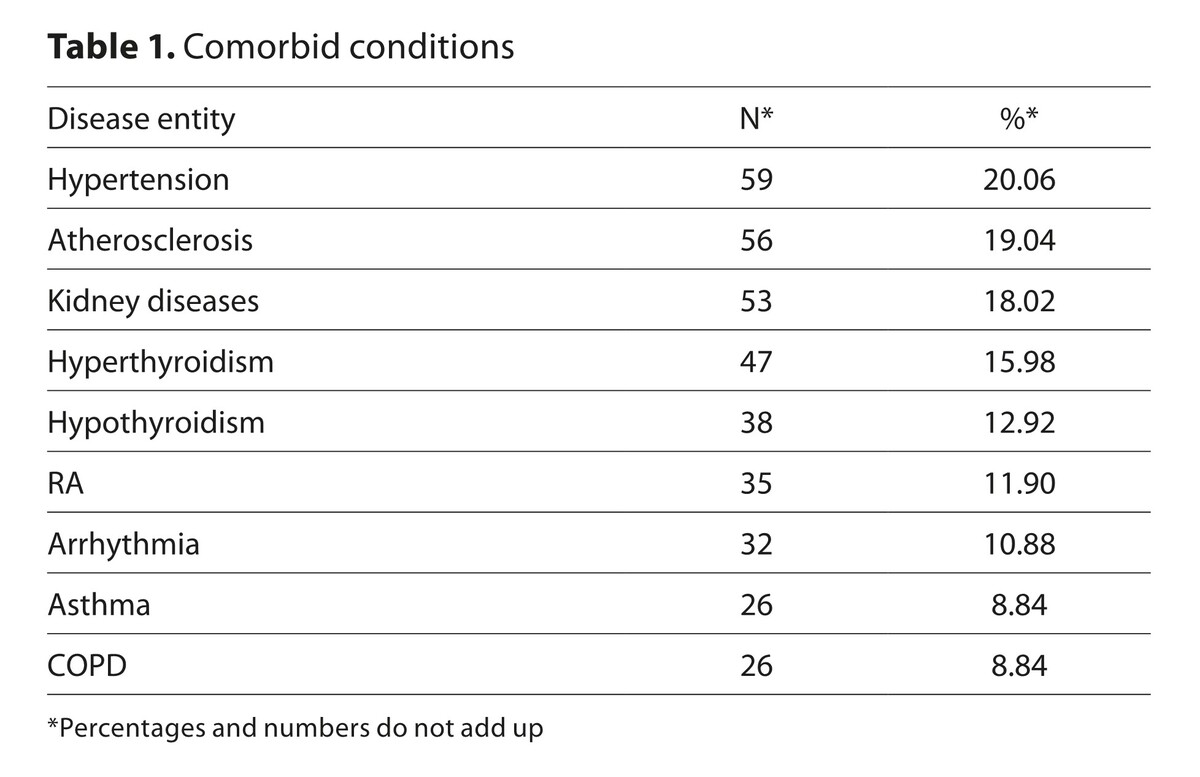
294 seniors diagnosed with type 2 diabetes living in the Lower Silesian Province in south-western Poland took part in the study. The study used a self-developed questionnaire collecting clinical and socio-demographic data, the WHOQOL-Bref questionnaire, Acceptance of Illness Scale (AIS), Self-Care of Diabetes Inventory (SCODI) and the Geriatric Depression Scale (GDS).
Results:
Significant relationships of QoL with BMI, level of education and place of residence, were observed. BMI was significantly negatively correlated with the psychological domain of functioning and the environmental functioning, the level of education was correlated with physical health, psychological and environmental functioning, while the place of residence was correlated with the perception of the QoL and environmental functioning. Acceptance of illness was positively correlated with the perception of QoL and one’s physical health. The results of regression analyses in predicting QoL in all domains showed that all models were a good fit for the data (p < 0.001), and the single predictor was maintenance of self-care. The level of depression was negatively correlated to a statistically significant degree with the perception of QoL and one’s health condition.
Conclusions:
BMI, level of education and place of residence had the highest impact on the quality of life of the participants. The quality of life of the participants improved with the increase in the acceptance of their illness. The higher the level of depression exhibited by the participants, the poorer they evaluated their quality of life.
Diabetes is commonly classified as a chronic disease of affluence due to the frequency of its incidence and the rate of its spreading. The aim of the study was to evaluate the quality of life of geriatric patients with type 2 diabetes.
Material and methods:
294 seniors diagnosed with type 2 diabetes living in the Lower Silesian Province in south-western Poland took part in the study. The study used a self-developed questionnaire collecting clinical and socio-demographic data, the WHOQOL-Bref questionnaire, Acceptance of Illness Scale (AIS), Self-Care of Diabetes Inventory (SCODI) and the Geriatric Depression Scale (GDS).
Results:
Significant relationships of QoL with BMI, level of education and place of residence, were observed. BMI was significantly negatively correlated with the psychological domain of functioning and the environmental functioning, the level of education was correlated with physical health, psychological and environmental functioning, while the place of residence was correlated with the perception of the QoL and environmental functioning. Acceptance of illness was positively correlated with the perception of QoL and one’s physical health. The results of regression analyses in predicting QoL in all domains showed that all models were a good fit for the data (p < 0.001), and the single predictor was maintenance of self-care. The level of depression was negatively correlated to a statistically significant degree with the perception of QoL and one’s health condition.
Conclusions:
BMI, level of education and place of residence had the highest impact on the quality of life of the participants. The quality of life of the participants improved with the increase in the acceptance of their illness. The higher the level of depression exhibited by the participants, the poorer they evaluated their quality of life.
REFERENCES (46)
1.
Lutomski P, Kaczoruk M, Florek-Łuszczki M. Ageing policy in Poland during the COVID-19 pandemic. Ann Agric Environ Med. 2021;28(4):551–557. doi:10.26444/aaem/143559.
3.
Maresova P, Javanmardi E, Barakovic S, et al. Consequences of chronic diseases and other limitations associated with old age – a scoping review. BMC Public Health 2019;19:1431. doi:10.1186/s12889-019-7762-5.
4.
Beard JR, Officer A, de Carvalho AI, et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–2154. doi:10.1016/S0140-6736(15)00516-4.
5.
Reynolds R, Dennis S, Hasan I, et al. A systematic review of chronic disease management interventions in primary care. BMC Fam Pract. 2018;19(1):11. doi:10.1186/s12875-017-0692-3.
6.
Krzemińska S, Bąk E, Polanská A, et al. Does gender affect health-related quality of life in patients with type 2 diabetes (ADDQoL) in Central European countries? Ann Agric Environ Med. 2023. doi:10.26444/aaem/161584.
7.
Stanowisko Polskiego Stowarzyszenia Diabetologicznego: „Current Topics In Diabetes – Zalecenia kliniczne dotyczące postępowania u chorych na cukrzycę 2022”. Polskie Towarzystwo Diabetologiczne, Official Journal of the Diabetes Poland, Termedia Publishing House; 2022. p. 9–11, 56–59.
8.
Petersmann A, Nauck M, Müller-Wieland D. Definition, Classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes. 2018;126(7):406–410. doi:10.1055/a-0584-6223.
9.
Cole JB, Florez JC. Genetics of diabetes mellitus and diabetes complications. Nat Rev Nephrol. 2020;16(7):377–390. doi:10.1038/s41581-020-0278-5.
10.
Speight J, Holmes-Truscott E, Hendrieckx C, et al. Assessing the impact of diabetes on quality of life: what have the past 25 years taught us? Diabet Med. 2020;37:483–492. doi:10.1111/dme.14196.
11.
Palamenghi L, Carlucci MM, Graffigna G. Measuring the Quality of Life in Diabetic Patients: A Scoping Review. J Diabetes Res. 2020;20:5419298. doi:10.1155/2020/5419298.
12.
Kaptacz I. Assessment of quality of life, acceptance of illness, needs and expectations of patients under palliative home care – preliminary pilot study. Palliative Med. 2018;10(3):137–144. doi:10.5114/pm.2018.79836.
13.
Haraldstad K, Wahl A, Andenaes R, et al. A systematic review of quality of life research in medicine and health sciences. Qual Life Res. 2019;28(10):2641–2650. doi:10.1007/s11136-019-02214-9.
14.
World Medical Association Declaration of Helsinki. 2013. JAMA, 310(20):2191. https://doi.org/10.1001/jama.2....
15.
Gnacińska-Szymańska M, Dardzińska J, Majkowicz M, et al. The assessment of quality of life in patients with excessive body mass using WHOQOL-BREF form. Endokrynol Otył Zab Przem Mat. 2012;8(4):136–142.
16.
Jankowska-Polańska B, Ilko A, Wleklik M. Influence the acceptance of the disease on quality of life of patients with hypertension. Arterial Hypertension. 2014;18(3):143–150.
17.
Kowalewska B, Cybulski M, Jankowiak B. et al. Acceptance of Illness, Satisfaction with Life, Sense of Stigmatization, and Quality of Life among People with Psoriasis: A Cross-Sectional Study. Dermatol Ther. 2020;10(3):413–430. doi:10.1007/s13555-020-00368-w.
18.
Krzemińska S, Czapor E. The level of self-care in patients with T2 diabetes using the Self-Care of Diabetes Inventory (SCODI) questionnaire. Współczesne Pielęgniarstwo i Ochrona Zdrowia. 2019;8(4):109–114.
19.
Hussenoeder FS, Jentzsch D, Matschinger H, et al. Depression and quality of life in old age: a closer look. Eur J. 2021;18:75–83. doi:10.1007/s10433-020-00573-8.
20.
Krawczyk-Wasilewska A, Gajewska E, Samborski W. Gender as one of the factors that may determine the quality of life in rheumatoid arthritis. Nowiny Lek. 2012;81(4):347–353.
21.
Olek D, Uchmanowicz I, Chudiak A, et al. Effect of acceptance of disease on quality of life in patients with chronić obstructive pulmonary disease. Nursing Topics. 2014;22(4):471–476.
22.
Bonora BM, Boscari F, Avogaro A, et al. Glycaemic Control Among People with Type 1 Diabetes During Lockdown for the SARS-CoV-2 Outbreak in Italy. Diabetes Ther. 2020;11:1369–1379. doi:10.1007/s13300-020-00829-7.
23.
Pazderska M. The quality of life and dietetic conditioning of diabetes patients receiving outpatient treatment. Pielęgniarstwo w Opiece Długoterminowej 2017;3:35–48. doi:10.19251/pwod/2017.3(4).
24.
Finbråten HS, Guttersrud Ø, Nordström G, et al. Explaining variance in health literacy among people with type 2 diabetes: the association between health literacy and health behaviour and empowerment. BMC Public Health. 2020;20:161. doi:10.1186/s12889-020-8274-z.
25.
Bottcher LB, Bandeira PFR, Vieira NB, et al. Quality of Life, BMI, and Physical Activity in Bariatric Surgery Patients: a Structural Equation Model. Obesity Surgery. 2020;30:2927–2934. doi:10.1007/s11695-020-04615-z.
26.
Chen HT, Chung Y., Chen YJ, et al. Effects of different types of exercise on body composition, muscle strength, and IGF-1 in the elderly with sarcopenic obesity. J Am Geriatrics Soc. 2017;65:827–832. doi:10.1111/jgs.14722.
27.
Hiol AN, von Hurst PR, Conlon CA, et al. Body composition associations with muscle strength in older adults living in Auckland, New Zealand. PLoS ONE. 2021;16(5):e0250439. doi:10.1371/journal.pone.0250439.
28.
Nemcova J, Hlinkova E, Farsky I, Ziakova K, Jarosova D, Zelenikova R, et al. Quality of life in patients with diabetic foot ulcer in Visegrad countries. J Clin Nursing. 2017;26(9–10):1245–1256. doi:10.1111/jocn.13508.
29.
León-Salas B, Ayala A, Blaya-Nováková V, et al. Quality of life across three groups of older adults differing in cognitive status and place of residence. Ger Gerontol Intern. 2015;15(5):627–635. /doi:10.1111/ggi.12325.
30.
Kirsten J, Ridley C, Turner S. Effective communication with older people. Nurs Older People. 2019;29:e1126. doi:10.7748/nop.2019.e1126.
31.
Kurpas D. Zachowania zdrowotne u pacjentów z somatycznymi chorobami przewlekłymi. In: Cybulski M, Krajewska-Kułak E, editors. Edukacja prozdrowotna seniorów jako szansa na pomyślne starzenie się na przykładzie miasta Białegostoku. Białystok: Uniwersytet Medyczny w Białymstoku; 2016. p. 45–60.
32.
Sienkiewicz-Wilowska JA. Społeczne aspekty bycia seniorem a rozwój osób w okresie późnej dorosłości. In: Edukacja osób starszych. Uwarunkowania. Trendy. Metody. Warszawa: Stowarzyszenie Trenerów Organizacji Pozarządowych; 2013. p. 27–40.
33.
van Leeuwen KM, van Loon MS, van Nes FA, et al. What does quality of life mean to older adults? A thematic synthesis. PLoS One. 2019;14(3):e0213263. doi:10.1371/journal.pone.0213263.
34.
Corrêa K, Gouvêa GR, Silva MAVD, et al. Quality of life and characteristics of diabetic patients. Ciencia Saude Coletiva. 2017; 22: 921–930. doi:10.1590/1413-81232017223.24452015.
35.
Freedland KE, Rich MW, Carney RM. Improving Quality of Life in Heart Failure. Curr Cardiol Rep. 2021;23:159. doi:10.1007/s11886-021-01588-y.
36.
Krzemińska S, Kostka A. Acceptance of illness and quality of life in patients with type 2 diabetes. J Educ Health Sport. 2021;11(5):86–100. doi:10.12775/JEHS.2021.11.05.009.
37.
Szpilewska K, Juzwiszyn J, Bolanowska Z, et al. Acceptance of disease and the quality of life in patients with enteric stoma. Pol J Surgery. 2018;90(1):13–17. doi:10.5604/01.3001.0011.5954.
38.
Kołtuniuk A, Pytel A, Kulik A, et al. The Role of Disease Acceptance, Life Satisfaction, and Stress Perception on the Quality of Life Among Patients With Multiple Sclerosis: A Descriptive and Correlational Study. Rehabil Nurs. 2021;46(4):205–213. doi:10.1097/RNJ.0000000000000288.
39.
Marthoenis M, Syukri M, Abdullah A, et al. Quality of life, depression, and anxiety of patients undergoing hemodialysis: Significant role of acceptance of the illness. Inter J Psychiatry Med. 2020;56(1):40–50. doi:10.1177/0091217420913382.
40.
Kwiendacz H, Nabrdalik K, Brzoza, Stokłosa I, et al. Knowledge about type 2 diabetes among visitors of two shopping centers in Upper Silesia, Poland: a survey research performed as a part of social action “Health under Control”. Clin Diabetol. 2018;7(4):182–188. doi: 10.5603/DK.2018.0017.
41.
Xu X, Han J, Li Y, et al. Effects of Orem’s Self-Care Model on the Life Quality of Elderly Patients with Hip Fractures. Pain Res Manag. 2020;20:5602683. doi:10.1155/2020/5602683.
42.
Tok Yildiz F, Kasikci M. Impact of Training Based on Orem’s Theory on Self-Care Agency and Quality of Life in Patients With Coronary Artery Disease. J Nurs Res. 2020;28(6):e125. doi:10.1097/JNR.0000000000000406.
43.
Zis P, Daskalaki A, Bountouni I, et al. Depression and chronic pain in the elderly: links and management challenges. Clinical Interventions in Aging. 2017;12:709–720.
44.
Kozieł P, Lomper K, Uchmanowicz B, et al. Association between acceptance of illness, anxiety and depression with assessment quality of life of breast cancer patients. Med Paliatywna Praktyce. 2016;10(1):28–36.
45.
Zhang Y, Chen Y, Ma L. Depression and cardiovascular disease in elderly: Current understanding. J Clin Neurosci. 2018;47:1–5. doi:10.1016/j.jocn.2017.09.022.
46.
Kodłubowska M, Zawada A. Determinant factors of quality of life in patients after amputation of a lower extremity in the course of atherosclerosis and type 2 diabetes. Piel Chirurgiczne Angiol. 2020;2(14):75–83.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.