Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Risk factors affecting the clinical course of COVID-19 in patients with lymphoid malignancies in the Omicron subvariants era – a real-world analysis by the Polish Adult Lukemia Study Group
1
Department of Haematology, National Medical Institute of the Ministry of Interior and Administration, Warsaw, Poland
2
Department of Haematology and Bone Marrow Transplantation, University of Medical Sciences, Poznań, Poland
3
University of Zielona Gora, Department of Haematology, Poland
4
Department of Haematology, Oncology and Radiotherapy, Multi-Specialist Hospital, Gorzów Wielkopolski, Poland
5
Department of Haematooncology and Bone Marrow Transplantation, Medical University, Lublin, Poland
6
Clinical Department of Haematology, Cell Therapies and Internal Diseases Medical University, Wrocław, Poland
7
Department of Haematology, Institute of Haematology and Transfusion Medicine, Warsaw, Poland
8
Department of Haematology and Bone Marrow Transplantation, Medical University of Silesia, Katowice, Poland
9
Department of Haematology, Oncology and Internal Medicine, Medical University, Warsaw, Poland
Corresponding author
Agnieszka Szymczyk
Department of Hematology, National Medical Institute of the Ministry of Interior and Administration, Wołoska 137 Str., 02-507, Warsaw, Poland
Department of Hematology, National Medical Institute of the Ministry of Interior and Administration, Wołoska 137 Str., 02-507, Warsaw, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Patients with lymphoid malignancies, were found to have a higher risk of SARS-CoV-2 infection and a severe course of COVID-19. Real-world data (RWD) is presented on the clinical course of COVID-19 in patients with lymphoid malignancies from the centres of the Polish Adult Leukemia Group (PALG).
Material and methods:
A retrospective analysis was carried between October 2023 – February 2024 of patients diagnosed with COVID-19.
Results:
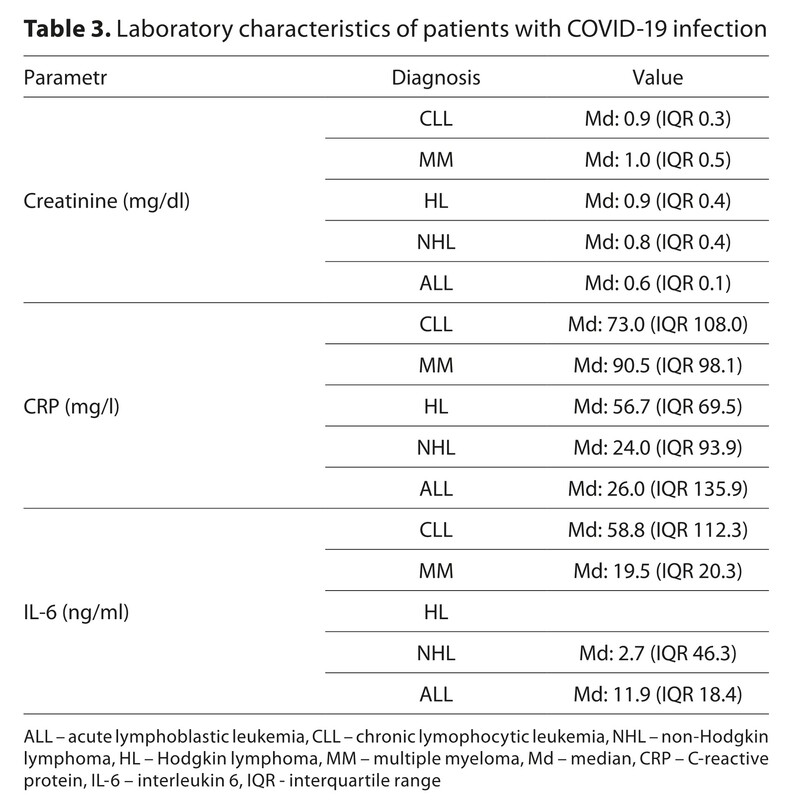
Antiviral treatment of COVID-19 was used in 72.9% of patients (51.8% nirmatrelvir+ritonavir, 9.4% remdesivir, 11.8% molnupiravir; the remaining patients were treated symptomatically. The hospitalization rate was 72.9%, but most patients presented with mild symptoms or asymptomatic COVID-19. Only 7.1% of patients required hospitalization in the Intensive Care Unit (ICU) and mechanical ventilation. The median hospitalization time was 10.0 days (IQR 15.0). A significant correlation was found between the length of hospitalization and the severity of COVID-19 course, assessed according to the AOTMiT scale, performance status according to the ECOG scale, number of previous COVID-19 episodes, use of antibiotic therapy, highest detected CRP and HCT (p < 0.05). On median, positive COVID-19 test result lasted 8.0 days (IQR 11.0), and the only risk factor for longer duration of COVID-19 test positivity was the absolute number and percentage of monocytes (p<0.05).
Conclusions:
Analysis showed that the clinical course of COVID-19 was mild in the majority of patients. Regarding the changes in the clinical course of COVID-19 over time, further studies are necessary to isolate the risk factors risk of severe infection.
Patients with lymphoid malignancies, were found to have a higher risk of SARS-CoV-2 infection and a severe course of COVID-19. Real-world data (RWD) is presented on the clinical course of COVID-19 in patients with lymphoid malignancies from the centres of the Polish Adult Leukemia Group (PALG).
Material and methods:
A retrospective analysis was carried between October 2023 – February 2024 of patients diagnosed with COVID-19.
Results:
Antiviral treatment of COVID-19 was used in 72.9% of patients (51.8% nirmatrelvir+ritonavir, 9.4% remdesivir, 11.8% molnupiravir; the remaining patients were treated symptomatically. The hospitalization rate was 72.9%, but most patients presented with mild symptoms or asymptomatic COVID-19. Only 7.1% of patients required hospitalization in the Intensive Care Unit (ICU) and mechanical ventilation. The median hospitalization time was 10.0 days (IQR 15.0). A significant correlation was found between the length of hospitalization and the severity of COVID-19 course, assessed according to the AOTMiT scale, performance status according to the ECOG scale, number of previous COVID-19 episodes, use of antibiotic therapy, highest detected CRP and HCT (p < 0.05). On median, positive COVID-19 test result lasted 8.0 days (IQR 11.0), and the only risk factor for longer duration of COVID-19 test positivity was the absolute number and percentage of monocytes (p<0.05).
Conclusions:
Analysis showed that the clinical course of COVID-19 was mild in the majority of patients. Regarding the changes in the clinical course of COVID-19 over time, further studies are necessary to isolate the risk factors risk of severe infection.
REFERENCES (34)
1.
Guo W, Zheng Y, Feng S. Omicron related COVID-19 prevention and treatment measures for patients with hematological malignancy and strategies for modifying hematologic treatment regimes. Front Cell Infect Microbiol. 2023 Oct 19;13:1207225.
2.
Ng HJ, Alata MK, Nguyen QT, et al. Managing and treating COVID-19 in patients with hematological malignancies: a narrative review and expert insights. Clin Exp Med. 2024;24(1):119.
3.
Warda H, Skórka K, Giannopoulos K. Covid-19 in patients with haematological malignancies. Acta Haematol Pol. 2024;55(2):73–89.
4.
Liu Y, Gu X, Li H, Zhang H, Xu J. Mechanisms of long COVID: An updated review. Chin Med J Pulm Crit Care Med. 2023 Dec 6;1(4):231–40.
5.
Wang L, Wang W, Xu R, Berger NA. SARS-CoV-2 primary and breakthrough infections in patients with cancer: Implications for patient care. Best Pract Res Clin Haematol. 2022 Sep;35(3):101384.
6.
Puła B, Pruszczyk K, Pietrusza E, et al. Outcome of SARS-CoV-2-Infected Polish Patients with Chronic Lymphocytic Leukemia. Cancers. 2022 Jan;14(3):558.
7.
Crassini K, Gibson J. Pathogenesis and management of immune dysfunction secondary to B cell haematological malignancies. Intern Med J. 2024 Jan;54(1):16–25.
8.
Shah M, El Chaer F, Ho DY, El Boghdadly Z. Managing infectious challenges in the age of molecular-targeted therapies for adult hematological malignancies. Transpl Infect Dis. 2024;26(3):e14283.
9.
Hallek M, Cheson BD, Catovsky D, et al. iwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood. 2018 Jun 21;131(25):2745–60.
10.
Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014 Nov;15(12):e538–548.
11.
Alaggio R, Amador C, Anagnostopoulos I, et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia. 2022 Jul;36(7):1720–48.
12.
Chatzikonstantinou T, Kapetanakis A, Scarfò L, et al. COVID-19 severity and mortality in patients with CLL: an update of the international ERIC and Campus CLL study. Leukemia. 2021 Dec;35(12):3444–54.
13.
Scarfò L, Chatzikonstantinou T, Rigolin GM, et al. COVID-19 severity and mortality in patients with chronic lymphocytic leukemia: a joint study by ERIC, the European Research Initiative on CLL, and CLL Campus. Leukemia. 2020 Sep;34(9):2354–63.
14.
Ehmsen S, Asmussen A, Jeppesen SS, et al. Antibody and T cell immune responses following mRNA COVID-19 vaccination in patients with cancer. Cancer Cell. 2021 Aug 9;39(8):1034–6.
15.
Niemann CU, da Cunha-Bang C, Helleberg M, Ostrowski SR, Brieghel C. Patients with CLL have a lower risk of death from COVID-19 in the Omicron era. Blood. 2022 Aug 4;140(5):445–50.
16.
Martínez-López J, de la Cruz J, Gil-Manso R, et al. COVID-19 Outcomes in Patients with Hematologic Malignancies in the Era of COVID-19 Vaccination and the Omicron Variant. Cancers. 2024 Jan;16(2):379.
17.
Wysocki J, Siewert B, Mastalerz-Migas A, et al. Vaccinations against COVID-19 in adults in the 2023/2024 season. Recommendations of the Polish Society of Vaccinology, the Polish Society of Family Medicine, the Polish Society of Epidemiology and Physicians of Infectious Diseases and the Polish Society of Gynecologists and Obstetricians. Lek POZ. 2024;10(1):23–34.
18.
Quinot C, Kirsebom F, Andrews N, et al. Severity of COVID-19 sublineages XBB/XBB 1.5/XBB1.16, EG.5.1. and JN.1. in England. Lancet Reg Health Eur. 2024 Aug;43:100975.
19.
Passamonti F, Cattaneo C, Arcaini L, et al. Clinical characteristics and risk factors associated with COVID-19 severity in patients with haematological malignancies in Italy: a retrospective, multicentre, cohort study. Lancet Haematol. 2020 Oct;7(10):e737–45.
20.
Cai J, Li C, CCCG ALL Study Group. COVID-19 infection in children with acute lymphoblastic leukemia in China: Mild clinical course after Omicron infection. Chin Med J (Engl). 2024 Aug 20;137(16):2008–10.
21.
Mitra AK, Mukherjee UK, Mazumder S, et al. Sample average treatment effect on the treated (SATT) analysis using counterfactual explanation identifies BMT and SARS-CoV-2 vaccination as protective risk factors associated with COVID-19 severity and survival in patients with multiple myeloma. Blood Cancer J. 2023 Dec 7;13(1):180.
22.
Ayako RM, Patel K, Ndede I, et al. Inflammatory, Hematological and Biochemical Biomarkers in COVID-19 Patients. Immun Inflamm Dis . 2024; 12: e70078. doi:10.1002/iid3.70078.
23.
Peng J, Yuan G, Deng X, et al. Diagnostic Value of Peripheral Hematologic Markers for Coronavirus Disease 2019 (COVID-19): A Multicenter. Cross-sectional Study. J Clin Lab Anal. 2020; 34: e23475. doi:10.1002/jcla.23475.
24.
Tiwari A, Lipponen A, Hokajärvi AM, et al. Detection and Quantification of SARS-CoV-2 RNA in Wastewater Influent in Relation to Reported COVID-19 Incidence in Finland. Water Res. 2022; 215: 118220. doi:10.1016/j.watres.2022.118220.
25.
Cook MR, Dykes K, White K, et al. Thrombotic and Clinical Outcomes in Patients with Hematologic Malignancy and COVID-19. Clin Lymphoma Myeloma Leuk. 2022 Jul;22(7):e452–8.
26.
Levi M, van Es N. COVID-19 associated coagulopathy and thrombosis in cancer. Thromb Res. 2022 May;213:S72–6.
27.
Kole C, Stefanou Ε, Karvelas N, Schizas D, Toutouzas KP. Acute and Post-Acute COVID-19 Cardiovascular Complications: A Comprehensive Review. Cardiovasc Drugs Ther. 2024 Oct 1;38(5):1017–32.
28.
Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022 Mar;28(3):583–90.
29.
Laracy JC, Kamboj M, Vardhana SA. Long and persistent COVID-19 in patients with hematologic malignancies: from bench to bedside. Curr Opin Infect Dis. 2022 Aug 1;35(4):271–9.
30.
Hueso T, Pouderoux C, Péré H, et al. Convalescent plasma therapy for B-cell–depleted patients with protracted COVID-19. Blood. 2020 Nov 12;136(20):2290–5.
31.
Yasuda H, Mori Y, Chiba A, et al. Resolution of One-Year Persisting COVID-19 Pneumonia and Development of Immune Thrombocytopenia in a Follicular Lymphoma Patient With Preceding Rituximab Maintenance Therapy: A follow-up Report and Literature Review of Cases With Prolonged Infections. Clin Lymphoma Myeloma Leuk. 2021 Oct;21(10):e810–6.
32.
Duléry R, Lamure S, Delord M, et al. Prolonged in-hospital stay and higher mortality after Covid-19 among patients with non-Hodgkin lymphoma treated with B-cell depleting immunotherapy. Am J Hematol. 2021 Aug;96(8):934–44.
33.
Lee CY, Shah MK, Hoyos D, et al. Prolonged SARS-CoV-2 infection in patients with lymphoid malignancies. Cancer Discov. 2022 Jan;12(1):62–73.
34.
Ravkov EV, Williams ESCP, Elgort M, et al. Reduced monocyte proportions and responsiveness in convalescent COVID-19 patients. Front Immunol. 2024 Jan 4;14:1329026.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.