Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Perinatal outcomes in multiparous women. The impact of urban and rural residence – a retrospective analysis from Poland
1
Department of Human Anatomy, Medical University of Warsaw, Poland
2
Department of Obstetrics and Gynaecology Didactics, Medical University of Warsaw, Poland
3
Department of Emergency Medical Services, Medical University of Warsaw, Poland
Corresponding author
Patryk Rzońca
Department of Emergency Medicine, Medical University of Lublin, Staszica 4-6, 20-081, Lublin, Poland
Department of Emergency Medicine, Medical University of Lublin, Staszica 4-6, 20-081, Lublin, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
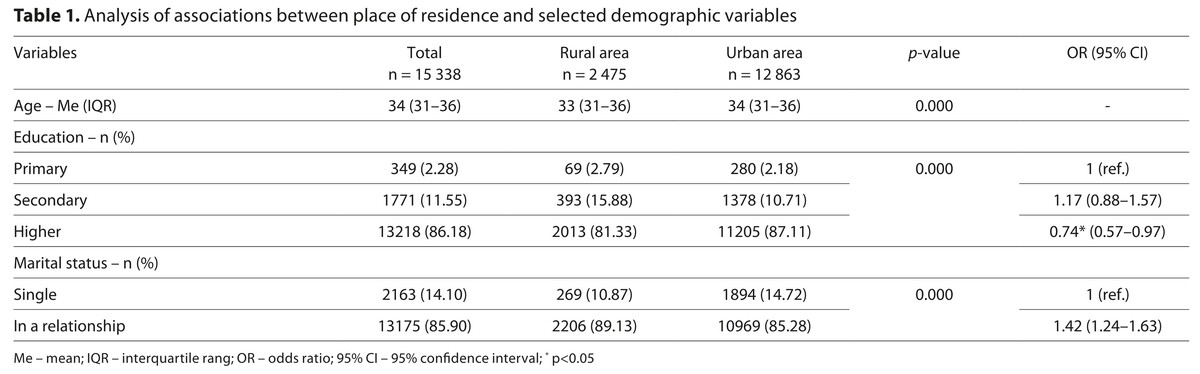
Multiparous women may experience additional health problems due to their past pregnancies. Place of residence has a significant impact on the health of the mother and her newborn baby, including on perinatal outcomes. Therefore, understanding the differences in perinatal outcomes between women living in rural and urban areas is crucial for shaping health promotion and public health measures. The aim of the study is to examine the association between place of residence and selected perinatal outcomes in multiparous women.
Material and methods:
This retrospective study was based on an analysis of the electronic medical records of women who gave birth at St. Sophia’s Hospital in Warsaw, Poland, between January 2017 – December 2021. The study included only multiparous women. The data analysed included place of residence, medical procedures performed and perinatal outcomes.
Results:
Multiparous women living in rural areas were more likely to give birth prematurely (OR=1.73) and have caesarean delivery (OR=1.21). They were also more likely to have spinal anaesthesia (OR=1.22) and amniotomy (OR=1.23). Babies born to mothers living in rural areas tended to be of lower birth weight (3,480 vs 3,500 grams) than babies born to women living in urban areas.
Conclusions:
The study showed that multiparous women living in rural areas are more likely to experience perinatal complications and undergo different medical procedures during labour than women living in urban areas. The findings demonstrate the need for differentiated perinatal care interventions for women living in rural and urban areas.
Multiparous women may experience additional health problems due to their past pregnancies. Place of residence has a significant impact on the health of the mother and her newborn baby, including on perinatal outcomes. Therefore, understanding the differences in perinatal outcomes between women living in rural and urban areas is crucial for shaping health promotion and public health measures. The aim of the study is to examine the association between place of residence and selected perinatal outcomes in multiparous women.
Material and methods:
This retrospective study was based on an analysis of the electronic medical records of women who gave birth at St. Sophia’s Hospital in Warsaw, Poland, between January 2017 – December 2021. The study included only multiparous women. The data analysed included place of residence, medical procedures performed and perinatal outcomes.
Results:
Multiparous women living in rural areas were more likely to give birth prematurely (OR=1.73) and have caesarean delivery (OR=1.21). They were also more likely to have spinal anaesthesia (OR=1.22) and amniotomy (OR=1.23). Babies born to mothers living in rural areas tended to be of lower birth weight (3,480 vs 3,500 grams) than babies born to women living in urban areas.
Conclusions:
The study showed that multiparous women living in rural areas are more likely to experience perinatal complications and undergo different medical procedures during labour than women living in urban areas. The findings demonstrate the need for differentiated perinatal care interventions for women living in rural and urban areas.
REFERENCES (22)
1.
Laksono AD, Rohmah N, Megatsari H. Barriers for multiparous women to using long-term contraceptive methods in Southeast Asia: case study in Philippines and Indonesia. BMC Public Health. 2022;22(1):1425. https://doi.org/10.1186/s12889....
2.
Central Statistical Office. Demographic Yearbook of Poland 2024. CSO, Warsaw 2024. https://stat.gov.pl/download/g...]. (access: 2025.07.29).
3.
Central Statistical Office. Population. Size and structure and vital statistics in Poland by territorial division in 2024. As of 31 December. CSO, Warsaw 2025. https://stat.gov.pl/obszary-te.... (access: 2025.07.29).
4.
Margerison CE, Wang X, Gemmill A, Goldman-Mellor S. Pregnancy-Associated Mortality During the Pandemic: Disparities by Rurality.Am J Prev Med. 2024 Sep 12:S0749–3797(24)00306–4. https://doi.org/10.1016/j.amep....
5.
Holcomb DS, Pengetnze Y, Steele A, et al. Geographic barriers to prenatal care access and their consequences. Am J Obstet Gynecol MFM. 2021;3(5):100442. https://doi.org/10.1016/j.ajog....
6.
Ospina M, Osornio-Vargas ÁR, Nielsen CC, et al. Socioeconomic gradients of adverse birth outcomes and related maternal factors in rural and urban Alberta, Canada: a concentration index approach. BMJ Open. 2020;10(1):e033296. https://doi.org/10.1136/bmjope....
7.
Bizuayehu HM, Harris ML, Chojenta C, et al. Maternal residential area effects on preterm birth, low birth weight and caesarean section in Australia: A systematic review. Midwifery. 2023;123:103704. https://doi.org/10.1016/j.midw....
8.
Szubert M, Ilowiecka M, Wilczynski J, et al. Health-Related Behaviors of Pregnant Women Residing in Urban and Rural Areas in Poland. Intern J Environ ResPublic Health. 2020;17(12):4395. https://doi.org/10.3390/ijerph....
9.
Genowska A, Fryc J, Szpak A, et al. Is socio-economic status associated with adverse birth outcomes in Poland? Ann Agric Environ Med. 2019;26(2):369–374. https://doi.org/10.26444/aaem/....
10.
Putri AS, Wurisastuti T, Suryaputri IY, Mubasyiroh R. Postpartum Depression in Young Mothers in Urban and Rural Indonesia. J Prev Med Public Health. 2023;56(3):272–281.
11.
Wallenborn JT, Valera CB, Kounnavong S, et al. Urban-Rural Gaps in Breastfeeding Practices: Evidence From Lao People’s Democratic Republic. Int J Public Health. 2021 Sep 9;66:1604062.
12.
Kitengie BL, Ngiele CM, Salamayi YS, et al. Assessment of the risk factors for low birth weight at Kitenge Hospital, Mbujimayi City, Democratic Republic of the Congo: 2018–2022. Orapuh J. 2024;5(3):e1125.
13.
Mehrnoush V, Ranjbarc A, Banihashemia F, et al. Urban-rural differences in the pregnancy-related adverse outcome. Gynecol Obstetrics Clin Med. 2023;3:51–55. https://doi.org/10.1016/j.gocm....
14.
Rodrigo-Gallardo PK, Caira-Chuquineyra B, Fernandez-Guzman D, et al. Determinants of non-institutional childbirth: Evidence from the Peruvian demographic and health survey. Eur J Obstet Gynecol Reprod Biol X. 2023;20:100250. https://doi.org/10.1016/j.euro....
15.
Giang, Hoang Thi Nam, et al. Factors associated with the very high caesarean section rate in urban areas of Vietnam. Plos One. 2022:e0273847.
16.
Tadese M, Desta Tessema S, Tsegaw Taye B. Adverse Perinatal Outcomes Among Grand Multiparous and Low Multiparous Women and Its Associated Factors in North Shewa Zone Public Hospitals: The Role of Parity. Int J Gen Med. 2021;14:6539–6548. https://doi.org/10.2147/IJGM.S....
17.
Li, Long, et al. Urban–rural disparity in the relationship between ambient air pollution and preterm birth. Intern J Health Geographics 2020;19:1–15.
18.
Mekie M, Taklual W. Magnitude of low birth weight and maternal risk factors among women who delivered in Debre Tabor Hospital, Amhara Region, Ethiopia: a facility based cross-sectional study. Ital J Pediatr. 2019;45(1):86. https://doi.org/10.1186/s13052....
19.
Mgaya AH, Massawe SN, Kidanto HL, Mgaya HN. Grand multiparity: is it still a risk in pregnancy? BMC Pregnancy Childbirth. 2013 Dec 23;13:241. https://doi.org/10.1186/1471-2....
20.
Gebremedhin M, Ambaw F, Admassu E, Berhane H. Maternal associated factors of low birth weight: a hospital based cross-sectional mixed study in Tigray, Northern Ethiopia. BMC Pregnancy Childbirth. 2015;15:222. https://doi.org/10.1186/s12884....
21.
Zhang R, Li C, Mi B. The different effects of prenatal nutrient supplementation on neonatal birth weights between urban and rural areas of northwest China: a cross sectional study. Asia Pac J Clin Nutr. 2018;27(4):875–885. https://doi.org/10.6133/apjcn.....
22.
Bączek G, Szyszka M, Rzońca P, et al. Place of residence and time of day as factors affecting the course of vaginal delivery. Ann Agric Environ Med. 2022;29(4):554–559. https://doi.org/10.26444/aaem/....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.