Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
CASE REPORT
Demographic factors, cancer history, and stress coping strategies among colorectal cancer patients during the end of the COVID-19 pandemic – a cross-sectional association study
1
Students’ Scientific Association, Department of Psychology, Chair of Psychosocial Aspects of Medicine, Faculty of Medicine, Medical University, Lublin, Poland
2
Students’ Scientific Association, Chair of Nursing Development, Faculty of Health Sciences, Medical University, Lublin, Poland
3
Department of Psychology, Chair of Psychosocial Aspects of Medicine, Faculty of Medical Sciences, Medical University, Lublin, Poland
4
Chair of Nursing Development, Faculty of Health Sciences, Medical University, Lublin, Poland
Corresponding author
Joanna Milanowska
Department of Psychology, Chair of Psychosocial Aspects of Medicine, Faculty of Medical Sciences, Medical University of Lublin, Poland
Department of Psychology, Chair of Psychosocial Aspects of Medicine, Faculty of Medical Sciences, Medical University of Lublin, Poland
KEYWORDS
TOPICS
ABSTRACT
Objective:
The aim of the is to determine the occurrence, severity, and correlates of distress in patients undergoing oncological treatment during the SARS-CoV-2 pandemic, focusing on the relationships with demographic factors, such as gender, age, residence, and treatment types. The relationships between distress and strategies for coping with cancer are also examined.
Material and methods:
A diagnostic survey method was utilised which incorporated such tools as the Distress Thermometer and the Mini-MAC Scale. The survey assessed stress severity and coping strategies among 104 oncological patients treated for colorectal cancer at the Oncology Centre of the Lublin Region, eastern Poland, during the last year of the pandemic.
Results:
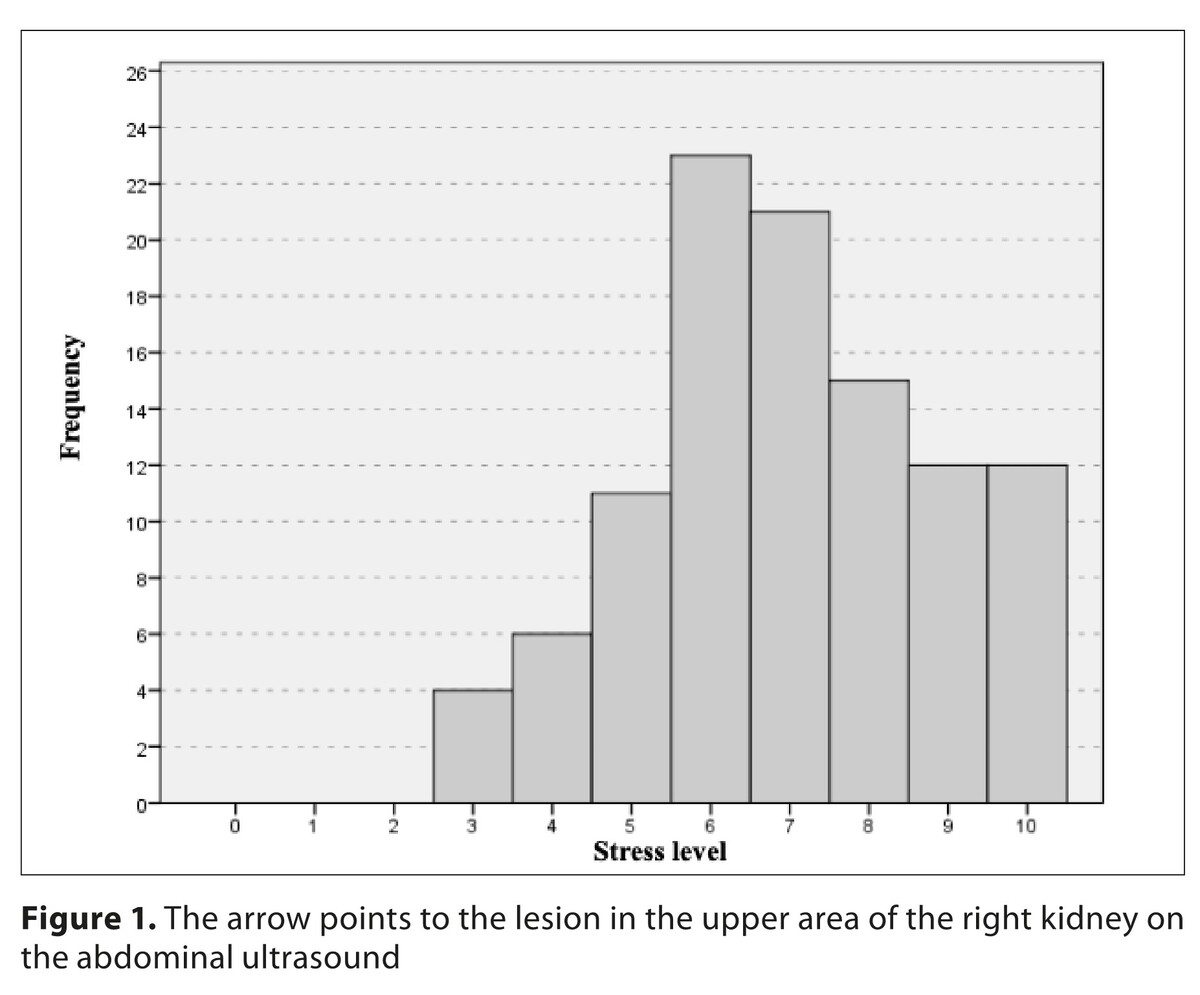
The average stress score was 6.96 [95% Confidence interval (CI) (6.60, 7.32)] with a standard deviation of 1,86. Women and younger patients exhibited higher anxiety and destructive coping styles. Analysis also revealed that cancer patients residing in rural areas reported higher levels of distress and more frequent use of destructive coping mechanisms, compared to their urban counterparts. Positive re-evaluation as a coping strategy increased with age. The study found that a history of cancer was associated with higher levels of distress and a greater use of destructive coping styles, regardless of the cancer stage or type of treatment.
Conclusions:
Coping strategies in cancer patients are significantly associated with demographic factors, including gender, age, and place of residence. Distress levels in cancer patients are positively correlated with non-constructive coping strategies, such as anxious preoccupation and helplessness-hopelessness. High levels of distress underscore the need for routine distress screening and comprehensive psychosocial support.
The aim of the is to determine the occurrence, severity, and correlates of distress in patients undergoing oncological treatment during the SARS-CoV-2 pandemic, focusing on the relationships with demographic factors, such as gender, age, residence, and treatment types. The relationships between distress and strategies for coping with cancer are also examined.
Material and methods:
A diagnostic survey method was utilised which incorporated such tools as the Distress Thermometer and the Mini-MAC Scale. The survey assessed stress severity and coping strategies among 104 oncological patients treated for colorectal cancer at the Oncology Centre of the Lublin Region, eastern Poland, during the last year of the pandemic.
Results:
The average stress score was 6.96 [95% Confidence interval (CI) (6.60, 7.32)] with a standard deviation of 1,86. Women and younger patients exhibited higher anxiety and destructive coping styles. Analysis also revealed that cancer patients residing in rural areas reported higher levels of distress and more frequent use of destructive coping mechanisms, compared to their urban counterparts. Positive re-evaluation as a coping strategy increased with age. The study found that a history of cancer was associated with higher levels of distress and a greater use of destructive coping styles, regardless of the cancer stage or type of treatment.
Conclusions:
Coping strategies in cancer patients are significantly associated with demographic factors, including gender, age, and place of residence. Distress levels in cancer patients are positively correlated with non-constructive coping strategies, such as anxious preoccupation and helplessness-hopelessness. High levels of distress underscore the need for routine distress screening and comprehensive psychosocial support.
ABBREVIATIONS
SPSS – Statistical Package for Social Sciences
CI – Confidence interval
MBSR – Like Mindfulness-Based Stress Reduction
CBT – Cognitive-Behavioural Therapy
DT – Distress Thermometer
NCCN – National Comprehensive Cancer Network
MAC – Mental Adjustment to Cancer Scale
KS – Kołmogorow-Smirnow Test
SKEW – Skewness Coefficient
KURT – Kurtosis
n – number of observations
% – percentage*
LL – Lower Limit of the 95% confidence interval for the proportion
UL – Upper Limit of the 95% confidence interval for the proportion
M – mean
SD – standard deviation
Mr – mean rank
H – Kruskal-Wallis Test result
p – test probability
df – degrees of freedom
ε2 – epsilon square
M – Mean
Min – minimum value*
Max – maximum value*
SD – standard deviation
p – test probability
R – linear regression
R2 – determination coefficient
b – standardized regression coefficient
F – global statistics
REFERENCES (31)
1.
Roth AJ, Kornblith AB, Batel-Copel L, et al. Rapid screening for psychologic distress in men with prostate carcinoma: A pilot study. Cancer. 1998;82(10):1904–1908. https://doi.org/10.1002/(SICI)...<1904:AID-CNCR14>3.0.CO;2-X.
2.
Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company; 1984.
3.
Marziliano A, Tuman M, Moyer A. The relationship between post-traumatic stress and post-traumatic growth in cancer patients and survivors: A systematic review and meta-analysis. Psychooncology. 2020;29(4):604–16. https://doi.org/10.1002/pon.53....
4.
Deshields TL, Gregorio SW-D, Flowers SR, et al. Addressing distress management challenges: Recommendations from the consensus panel of the American Psychosocial Oncology Society and the Association of Oncology Social Work. CA Cancer J Clin. 2021;71(5):407–36. https://doi.org/10.3322/caac.2....
5.
Veeraiah S, Kayser K, Sudhakar R. Psychosocial factors influencing distress among cancer patients in South India. J Psychosoc Oncol Res Pract. 2022;4(1). https://doi.org/10.1097/or9.00....
6.
Zhang MF, Wen YS, Liu WY, et al. Effectiveness of mindfulness-based therapy for reducing anxiety and depression in patients with cancer: A meta-analysis. Medicine (Baltimore). 2019;98(45). https://doi.org/10.1097/md.000....
7.
Leung J, Pachana NA, McLaughlin D. Social support and health-related quality of life in women with breast cancer: a longitudinal study. Psychooncology. 2020;29(4):836–43. https://doi.org/10.1002/pon.53....
9.
Polish Psycho-Oncological Society. Guidelines for the Psychological Care of Cancer Patients. 2020.
10.
Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients: A multicenter evaluation of the distress thermometer. Cancer. 2005;103(7):1494–1502. https://doi.org/10.1002/cncr.2....
11.
Watson M, Law MG, Santos MD, et al. The Mini-MAC. J Psychosocial Oncol. 1994;12(3):33–46. https://doi.org/10.1300/j077v1....
12.
Juczyński Z. Narzedzia pomiaru w promocji i psychologii zdrowia. Warszawa: Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego; 2001.
13.
Carlson LE, Zelinski EL, Toivonen KI, et al. Prevalence of psychosocial distress in cancer patients across 55 North American cancer centers. J Psychosoc Oncol. 2019;37(1):5–21. https://doi.org/10.1080/073473....
14.
Zhou J, Wang Z, Chen X, Li Q. Gender Differences in Psychosocial Outcomes and Coping Strategies of Patients with Colorectal Cancer: A Systematic Review. Healthcare (Basel). 2023;11(18):2591. https://doi.org/10.3390/health....
15.
Johns SA, Brown LF, Beck-Coon K, et al. Randomized controlled pilot study of mindfulness-based stress reduction for persistently fatigued cancer survivors. Psychooncol. 2015;24(8):885–93. https://doi.org/10.1002/pon.36....
16.
Secinti E, Tometich DB, Johns SA, Mosher CE. Meta-analysis of the effects of psychosocial interventions on survival time in cancer patients. Psychooncol. 2019;28(12):2381–93. https://doi.org/10.1002/pon.52....
17.
Bottaro R, Faraci P. The influence of socio-demographics and clinical characteristics on coping strategies in cancer patients: a systematic review. Support Care Cancer. 2022;30(11):8785–8803. https://doi.org/10.1007/s00520....
18.
Tsamakis K, Tsiptsios D, Ouranidis A, et al. Oncology during the COVID-19 pandemic: challenges, dilemmas, and the psychosocial impact on cancer patients. Oncology Letters. 2020;20(1):441–47. https://doi.org/10.3892/ol.202....
19.
Chen N, McGrath CB, Stopsack KH, et al. Social Integration and Long-Term Physical and Psychosocial Quality of Life Among Prostate Cancer Survivors in the Health Professionals Follow-up Study. J Cancer Surviv. Published online July 1, 2024. https://doi.org/10.1007/s11764....
20.
Romito F, Dellino M, Loseto G, et al. Psychological Distress in Outpatients With Lymphoma During the COVID-19 Pandemic. Front Oncol. 2020;10:1270. https://doi.org/10.3389/fonc.2....
21.
Rodriguez-Gonzalez A, Velasco-Durantez V, Martin-Abreu C, et al. Fatigue, Emotional Distress, and Illness Uncertainty in Patients with Metastatic Cancer: Results from the Prospective NEOETIC_SEOM Study. Curr Oncol. 2022;29(12):9722–33. https://doi.org/10.3390/curron....
22.
Kim Y, Baker F, Spillers RL. Cancer caregivers’ quality of life: effects of gender, relationship, and appraisal. Psychooncol. 2010;19(10):1047–1054. https://doi.org/10.1002/pon.16....
23.
Kvillemo P, Bränström R. Coping with breast cancer: a meta-analysis. PLoS One. 2014;9(11). https://doi.org/10.1371/journa....
24.
Obispo B, Cruz-Castellanos P, Fernández-Montes A, et al. Coping strategies as mediators of uncertainty and psychological distress in patients with advanced cancer. Psycho-Oncol. 2023;32(11):1694–1701. https://doi.org/10.1002/pon.62....
25.
Ng DWL, Chan FHF, Barry TJ, et al. Psychological distress during the 2021 COVID-19 pandemic: A comparison of cancer patients and the general population. Supportive Care in Cancer. 2021;29(10):6085–6095. https://doi.org/10.1007/s00520....
26.
Zhou Y, Li W, Hong Y, et al. Longitudinal study of psychological distress among breast cancer patients during COVID-19 pandemic. Breast Cancer Research and Treatment. 2022;191(1):53–61. https://doi.org/10.1007/s10549....
27.
Riera R, Bagattini ÂM, Pacheco RL, et al. Delays and Disruptions in Cancer Health Care Due to COVID-19 Pandemic: Systematic Review. JCO Glob Oncol. 2021;7:311–323. https://doi.org/10.1200/GO.20.....
28.
Teglia F, Angelini M, Astolfi L, et al. Global Association of COVID-19 Pandemic Measures With Cancer Screening: A Systematic Review and Meta-analysis. JAMA Oncol. 2022;8(9):1287–1293. https://doi.org/10.1001/jamaon....
29.
Shah R, Hanna NM, Loo CE, et al. The global impact of the COVID-19 pandemic on delays and disruptions in cancer care services: a systematic review and meta-analysis. Nat Cancer. 2025;6(1):194–204. https://doi.org/10.1038/s43018....
30.
Sigorski D, Sobczuk P, Osmola M, et al. Impact of COVID-19 on anxiety levels among patients with cancer actively treated with systemic therapy. ESMO Open. 2020;5(5):e000970. https://doi.org/10.1136/esmoop....
31.
Doege D, Frick J, Eckford RD, et al. Anxiety and depression in cancer patients and survivors in the context of restrictions in contact and oncological care during the COVID-19 pandemic. Int J Cancer. 2025;156(4):711–722. https://doi.org/10.1002/ijc.35....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.