Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Pediculosis capitis and scabies in nurses from Eastern Poland – occupational risk and environmental determinants
1
Department of Biology and Parasitology, Faculty of Health Sciences, Medical University of Lublin, Lublin, Poland
2
Department of Health Promotion and Treatment of Obesity, Chair of Pathophysiology, Medical University of Silesia,
Katowice, Poland
3
Faculty of Physical Education and Health, University of Physical Education, Biala Podlaska, Poland
4
Faculty of Human Sciences, Higher School of Economics and Innovation (WSEI) Lublin, Poland
Ann Agric Environ Med. 2023;30(2):244-251
KEYWORDS
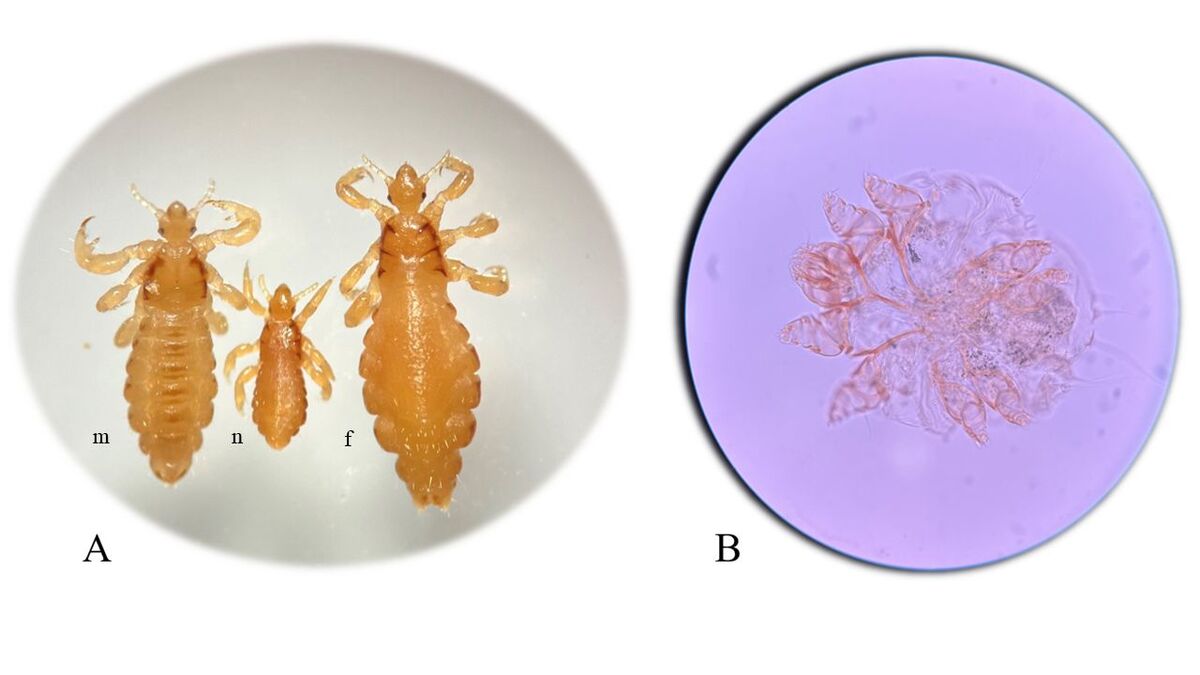
occupational hazardsscabiesPediculus humanus capitisSarcoptes scabiei var. hominispediculosis capitispediatric nursing
TOPICS
ABSTRACT
Introduction and objective:
Nurses are a group of healthcare professionals particularly vulnerable to infestations by Pediculus humanus capitis and Sarcoptes scabiei var. hominis contracted from patients under their medical care.
Material and methods:
The cross-sectional study included 322 professionally active nurses within public healthcare units in eastern Poland. The research tool was a questionnaire collecting anonymized data on the occurrence of pediculosis capitis and scabies in nurses, and their patients, concerning the environmental determinants in the period 2001–2013. The study was retrospective and participation of nurses was voluntary.
Results:
The obtained results indicated that 24.8% and 9.9% of the 322 respondents were infested by head lice and scabies mites, respectively. During their professional work, most nurses contracted head lice once (76.2%) while others (23.8%) were infested twice or more. The respondents did not declare repeated occupational scabies. The risk of contracting pediculosis capitis and scabies was not related to the length of service, but increased with the rise in the number of patients provided with nursing care. In the head lice-infested patients, the majority were aged 6–10 years (31.3%), while in the case of scabietic patients, children aged 0–5 years prevailed (26.4%).
Conclusions:
In medical care facilities, regular hygienic checks of both patients and medical staff, covering the condition of the skin and scalp, should be mandatory. The spread of pediculosis capitis and scabies among nurses can be reduced by the implementation not only of protective procedures mitigating occupational risk, but also the improvement of working conditions in medical facilities.
Nurses are a group of healthcare professionals particularly vulnerable to infestations by Pediculus humanus capitis and Sarcoptes scabiei var. hominis contracted from patients under their medical care.
Material and methods:
The cross-sectional study included 322 professionally active nurses within public healthcare units in eastern Poland. The research tool was a questionnaire collecting anonymized data on the occurrence of pediculosis capitis and scabies in nurses, and their patients, concerning the environmental determinants in the period 2001–2013. The study was retrospective and participation of nurses was voluntary.
Results:
The obtained results indicated that 24.8% and 9.9% of the 322 respondents were infested by head lice and scabies mites, respectively. During their professional work, most nurses contracted head lice once (76.2%) while others (23.8%) were infested twice or more. The respondents did not declare repeated occupational scabies. The risk of contracting pediculosis capitis and scabies was not related to the length of service, but increased with the rise in the number of patients provided with nursing care. In the head lice-infested patients, the majority were aged 6–10 years (31.3%), while in the case of scabietic patients, children aged 0–5 years prevailed (26.4%).
Conclusions:
In medical care facilities, regular hygienic checks of both patients and medical staff, covering the condition of the skin and scalp, should be mandatory. The spread of pediculosis capitis and scabies among nurses can be reduced by the implementation not only of protective procedures mitigating occupational risk, but also the improvement of working conditions in medical facilities.
ACKNOWLEDGEMENTS
The authors would like to thank all the nurses who devoted
their time and attention to contributing to this study. Their
commitment and belief that this research is relevant from
their perspective motivated us to share the results with a
broader audience.
REFERENCES (64)
1.
Drali R, Mumcuoglu K, Raoult D. Human Lice in Paleoentomology and Paleomicrobiology. Microbiol Spectr. 2016;4(4):10.1128. https://doi.org/10.1128/microb....
2.
Thomas J, Christenson JK, Walker E, Baby KE, Peterson GM. Scabies-An ancient itch that is still rampant today. J Clin Pharm Ther. 2017;42(6):793–799.
3.
Sangaré AK, Doumbo OK, Raoult D. Management and Treatment of Human Lice. Biomed Res Int. 2016;2016:8962685. https://doi.org/10.1155/2016/8....
4.
Thomas C, Coates SJ, Engelman D, Chosidow O, Chang AY. Ectoparasites: Scabies. J Am Acad Dermatol. 2020;82(3):533–548. https://doi.org/10.1016/j.jaad....
5.
Gramp P, Gramp D. Scabies in remote Aboriginal and Torres Strait Islander populations in Australia: A narrative review. PLoS Negl Trop Dis. 2021;15(9):e0009751. https://doi.org/10.1371/journa....
6.
Fu YT, Yao C, Deng YP, et al. Human pediculosis, a global public health problem. Infect Dis Poverty. 2022;11(1):58. https://doi.org/10.1186/s40249....
7.
Widaty S, Miranda E, Cornain EF, Rizky LA. Scabies: update on treatment and efforts for prevention and control in highly endemic settings. J Infect Dev Ctries. 2022;16(2):244–251. https://doi.org/10.3855/jidc.1....
8.
Leung AKC, Lam JM, Leong KF. Scabies: A Neglected Global Disease. Curr Pediatr Rev. 2020;16(1):33–42. https://doi.org/10.2174/157339....
9.
Hatam-Nahavandi K, Ahmadpour E, Pashazadeh F, et al. Pediculosis capitis among school-age students worldwide as an emerging public health concern: a systematic review and meta-analysis of past five decades. Parasitol Res. 2020;119(10):3125–3143. https://doi.org/10.1007/s00436....
10.
Firoozfar F, Moosa-Kazami SH, Bahrami A, Ahmed-Yusuf M, Saghafipour A, Armoon Z, Rajabzadeh R, Hosseini SH. Head lice infestation (Pediculus humanus capitis) prevalence and its associated factors, among the kormanj tribes in North Khorasan Province. Shiraz E Med J. 2018;20:e80292. https://doi.org/10.5812/semj.8....
11.
Pruksachatkunakorn C, Wongthanee A, Kasiwat V. Scabies in Thai orphanages. Pediatr Int. 2003;45(6):724–727. https://doi.org/10.1111/j.1442....
12.
Burkhart CN, Burkhart CG. Fomite transmission in head lice. J Am Acad Dermatol. 2007;56(6):1044–1047. https://doi.org/10.1016/S0140-....
13.
Arlian LG, Morgan MS. A review of Sarcoptes scabiei: past, present and future. Parasit Vectors. 2017;10(1):297. https://doi.org/10.1186/s13071....
14.
Arlian LG, Estes SA, Vyszenski-Moher DL. Prevalence of Sarcoptes scabiei in the homes and nursing homes of scabietic patients. J Am Acad Dermatol. 1988;19(5 Pt 1):806–811. https://doi.org/10.1016/s0190-....
15.
Louni M, Amanzougaghene N, Mana N, et al. Detection of bacterial pathogens in clade E head lice collected from Niger’s refugees in Algeria. Parasit Vectors. 2018;11(1):348. https://doi.org/10.1186/s13071....
16.
Nazari M, Azizi A. Epidemiological Pattern of Scabies and Its Social Determinant Factors in West of Iran. Health 2014;6:1972–1977. https://doi.org/10.4236/health....
17.
Arnaud A, Chosidow O, Détrez MA, et al. Prevalences of scabies and pediculosis corporis among homeless people in the Paris region: results from two randomized cross-sectional surveys (HYTPEAC study). Br J Dermatol. 2016;174(1):104–112. https://doi.org/10.1111/bjd.14....
18.
Bartosik K, Tytuła A, Zając Z, et al. Scabies and Pediculosis in Penitentiary Institutions in Poland-A Study of Ectoparasitoses in Confinement Conditions. Int J Environ Res Public Health. 2020;17(17):6086. https://doi.org/10.3390/ijerph....
19.
Di Meco E, Di Napoli A, Amato LM, et al. Infectious and dermatological diseases among arriving migrants on the Italian coasts. Eur J Public Health. 2018;28(5):910–916. https://doi.org/10.1093/eurpub....
20.
Gunning K, Kiraly B, Pippitt K. Lice and Scabies: Treatment Update. Am Fam Physician. 2019;99(10):635–642.
21.
Ogbuefi N, Kenner-Bell B. Common pediatric infestations: update on diagnosis and treatment of scabies, head lice, and bed bugs. Curr Opin Pediatr. 2021;33(4):410–415. https://doi.org/10.1097/MOP.00....
22.
Richards RN. Scabies: Diagnostic and Therapeutic Update. J Cutan Med Surg. 2021;25(1):95–101. https://doi.org/10.1177/120347....
23.
Dagne H, Biya AA, Tirfie A, Yallew WW, Dagnew B. Prevalence of pediculosis capitis and associated factors among schoolchildren in Woreta town, northwest Ethiopia. BMC Res Notes. 2019;12(1):465. https://doi.org/10.1186/s13104....
24.
Ghofleh Maramazi H, Sharififard M, Jahanifard E, et al. Pediculosis humanus capitis Prevalence as a Health Problem in Girl’s Elementary Schools, Southwest of Iran (2017–2018). J Res Health Sci. 2019;19(2):e00446.
25.
Çetinkaya Ü, Şahin S, Ulutabanca RÖ. The Epidemiology of Scabies and Pediculosis in Kayseri. Turkiye Parazitol Derg. 2018;42(2):134–137. https://doi.org/10.5152/tpd.20....
26.
Alberfkani MI, Mero WMS. The Incidence of Scabies and Head Lice and Their Associated Risk Factors among Displaced People in Cham Mishko Camp, Zakho City, Duhok Province, Iraq. Pol J Microbiol. 2020;69(4):463–469. https://doi.org/10.33073/pjm-2....
27.
Kim DH, Yun SY, Park YC, Kang SA, Yu HS. Prevalence of scabies in long-term care hospitals in South Korea. PLoS Negl Trop Dis. 2020;14(8):e0008554. https://doi.org/10.1371/journa....
28.
Villar R, Gemma M, Mirabent J, Pablo HJ, Serra C. Management of an outbreak of scabies in a social-health centre in Barcelona. Occup Environ Med. 2016:73, A144. http://dx.doi.org/10.1136/oeme....
29.
Cassell JA, Middleton J, Nalabanda A, et al. Scabies outbreaks in ten care homes for elderly people: a prospective study of clinical features, epidemiology, and treatment outcomes. Lancet Infect Dis. 2018;18(8):894–902. https://doi.org/10.1016/S1473-....
30.
Arega B, Diro E, Zewude T, et al. High levels of scabies and malnutrition amongst orphans referred to a hospital in Addis Ababa, Ethiopia. J Infect Dev Ctries. 2020;14(6.1):48S–52S. https://doi.org/10.3855/jidc.1....
31.
Morrison EJ, Middleton J, Lanza S, et al. Do we know how scabies outbreaks in residential and nursing care homes for the elderly should be managed? A systematic review of interventions using a novel approach to assess evidence quality. Epidemiol Infect. 2019;147:e250. https://doi.org/10.1017/S09502....
32.
Obasanjo OO, Wu P, Conlon M, et al. An outbreak of scabies in a teaching hospital: lessons learned. Infect Control Hosp Epidemiol. 2001;22(1):13–18. https://doi.org/10.1086/501818.
33.
Ahn YS, Lim HS. Occupational infectious diseases among Korean health care workers compensated with Industrial Accident Compensation Insurance from 1998 to 2004. Ind Health. 2008;46(5):448–454. https://doi.org/10.2486/indhea....
34.
Vijayan V, Marrero E, Gaspar A, Wisdom C, Honeycutt MD, Linam WM. Outbreak of scabies in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2019;40(5):613–614. https://doi.org/10.1017/ice.20....
35.
Leistner R, Buchwald D, Beyer M, Philipp S. Scabies outbreak among healthcare workers in a German acute care hospital. J Infect Prev. 2017;18(4):189–192. https://doi.org/10.1177/175717....
36.
Redondo-Bravo L, Fernandez-Martinez B, Gómez-Barroso D, et al. Scabies in Spain? A comprehensive epidemiological picture. PLoS One. 2021;16(11):e0258780. https://doi.org/10.1371/journa....
37.
Statistical Yearbook of Lubelskie Voivodship, Statistical Office in Lublin 2014, https://lublin.stat.gov.pl/en/...# (access: 2023.01.15).
38.
Czarkowski MP, Cielebąk E, Stępień E, Kondej B. Infectious diseases and poisonings in Poland in 2004. Warsaw 2005. http://wwwold.pzh.gov.pl/oldpa... (access: 2023.01.10).
39.
Czarkowski MP, Cielebąk E, Dacka P, Kondej B. Infectious diseases and poisonings in Poland in 2005. Warsaw 2006. http://wwwold.pzh.gov.pl/oldpa... (access: 2023.01.10).
40.
Czarkowski MP, Cielebąk E, Dacka P, Kondej B. Infectious diseases and poisonings in Poland in 2006. Warsaw 2007. http://wwwold.pzh.gov.pl/oldpa... (access: 2023.01.10).
41.
Czarkowski MP, Cielebąk E, Dacka P, Kondej B. Infectious diseases and poisonings in Poland in 2007. Warsaw 2008. http://wwwold.pzh.gov.pl/oldpa... (access: 2023.01.10).
42.
Czarkowski MP, Cielebąk E, Kondej B, Staszewska E. Infectious diseases and poisonings in Poland in 2008. Warsaw 2009. http://wwwold.pzh.gov.pl/oldpa... (access: 2023.01.10).
43.
Fu YT, Yao C, Deng YP, et al. Human pediculosis, a global public health problem. Infect Dis Poverty. 2022;11(1):58. https://doi.org/10.1186/s40249....
44.
Arlian LG, Runyan RA, Achar S, Estes SA. Survival and infectivity of Sarcoptes scabiei var. canis and var. hominis. J Am Acad Dermatol. 1984;11(2 Pt 1):210–215. https://doi.org/10.1016/s0190-....
45.
Ozdamar M, Turkoglu S. A nosocomial scabies outbreak originating from immunocompromised transplant patients in Turkey: Upholstery as a possible cause. Transpl Infect Dis. 2020;22(4):e13284. doi:10.1111/tid.13284.
46.
Xu T, Durst M, Keck T, Dixon H, Yassin MH. A scabies outbreak in an inpatient rehabilitation setting. Am J Infect Control. 2022;S0196–6553(22)00733–7. https://doi.org/10.1016/j.ajic....
47.
Buczek A, Markowska-Gosik D, Widomska D, Kawa IM. Pediculosis capitis among schoolchildren in urban and rural areas of eastern Poland. Eur J Epidemiol. 2004;19(5):491–495. https://doi.org/10.1023/b:ejep....
48.
Bartosik K, Buczek A, Zając Z, Kulisz J. Head pediculosis in schoolchildren in the eastern region of the European Union. Ann Agric Environ Med. 2015;22(4):599–603. https://doi.org/10.5604/123219....
49.
Buczek A, Pabis B, Bartosik K, Stanislawek IM, Salata M, Pabis A. Epidemiological study of scabies in different environmental conditions in central Poland. Ann Epidemiol. 2006;16(6):423–428. https://doi.org/10.1016/j.anne....
50.
Tagka A, Lambrou GI, Braoudaki M, Panagiotopoulos T, Papanikolaou E, Laggas D. Socioeconomical Factors Associated With Pediculosis (Phthiraptera: Pediculidae) in Athens, Greece. J Med Entomol. 2016;53(4):919–922. https://doi.org/10.1093/jme/tj....
51.
Saraswat N, Shankar P, Chopra A, Mitra B, Kumar S. Risk Factors Associated with Head Lice Infestation in Rural Pediatric Patients. Indian Dermatol Online J. 2020;11(1):25–28. https://doi.org/10.4103/idoj.I....
52.
Birkemoe T, Lindstedt HH, Ottesen P, Soleng A, Nass O, Rukke BA. Head lice predictors and infestation dynamics among primary school children in Norway. Fam Pract. 2016;33(1):23–29. https://doi.org/10.1093/fampra....
53.
Galassi F, Ortega-Insaurralde I, Adjemian V, Gonzalez-Audino P, Picollo MI, Toloza AC. Head lice were also affected by COVID-19: a decrease on Pediculosis infestation during lockdown in Buenos Aires. Parasitol Res. 2021;120(2):443–450. https://doi.org/10.1007/s00436....
54.
Marotta M, Toni F, Dallolio L, Toni G, Leoni E. Management of a family outbreak of scabies with high risk of spread to other community and hospital facilities. Am J Infect Control. 2018;46(7):808–813. https://doi.org/10.1016/j.ajic....
55.
Singhasivanon OU, Lawpoolsri S, Mungthin M, Yimsamran S, Soonthornworasiri N, Krudsood S. Prevalence and Alternative Treatment of Head-Lice Infestation in Rural Thailand: A Community-Based Study. Korean J Parasitol. 2019;57(5):499–504. https://doi.org/10.3347/kjp.20....
56.
Mounsey KE, Murray HC, King M, Oprescu F. Retrospective analysis of institutional scabies outbreaks from 1984 to 2013: lessons learned and moving forward. Epidemiol Infect. 2016;144(11):2462–2471. https://doi.org/10.1017/S09502....
57.
Korycinska J, Dzika E, Kloch M. Epidemiology of scabies in relation to socio-economic and selected climatic factors in north-east Poland. Ann Agric Environ Med. 2020;27(3):374–378. https://doi.org/10.26444/aaem/....
58.
Hama-Karim YH, Azize PM, Ali SI, Ezzaddin SA. Epidemiological Study of Pediculosis among Primary School Children in Sulaimani Governorate, Kurdistan Region of Iraq. J Arthropod Borne Dis. 2022;16(1):72–83. https://doi.org/10.18502/jad.v....
59.
Nejati J, Keyhani A, Tavakoli Kareshk A, et al. Prevalence and Risk Factors of Pediculosis in Primary School Children in South West of Iran. Iran J Public Health. 2018;47(12):1923–1929.
60.
Djohan V, Angora KE, Miezan S, et al. Pediculosis capitis in Abidjan, Côte d’Ivoire: Epidemiological profile and associated risk factors. Parasite Epidemiol Control. 2020;11:e00159. https://doi.org/10.1016/j.pare....
61.
Sánchez-Casas RM, Fernández-Salas I, Laguna-Aguilar M, Rodríguez-Rojas JJ, Medina-Ponce ML, Díaz-González EE. Pediculosis Affects Mexican Children from Different Socioeconomic Status Equally: A Cross-Sectional Study. J Trop Pediatr. 2021;67(3):fmaa041. https://doi.org/10.1093/tropej....
62.
Kartashova OV, Lobuteva LA, Zakharova OV, Lobuteva AV, Goykhman AA. Medical and Social Factors of Pediculosis. Open Access Maced J Med Sci. 2019;7(19):3240–3244. https://doi.org/10.3889/oamjms....
63.
Neuberg M, Banfić I, Cikač T, Ribić R, Zember S, Meštrović T. Knowledge, Attitudes, Psychosocial Perspectives and Applied Epidemiology in the Control of Head Lice (pediculosis capitis) in Croatian Preschool Children: A Qualitative Study on Childcare Professionals and Health Coordinators. Children (Basel). 2022;9(1):66. https://doi.org/10.3390/childr....
64.
Bartosik K, Janczaruk M, Zając Z, et al. Head Lice Infestation in Schoolchildren, in Poland-Is There a Chance for Change? J Clin Med. 2022;11(3):783. https://doi.org/10.3390/jcm110....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.