Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Hand function after muscle transfer in spastic hemiparesis patients
1
Orthopaedic and Paediatric Department, Central Teaching Hospital, Medical University, Łódź, Poland
2
Paediatric Orthopedic and Rehabilitation Department, Medical University, Lublin, Poland
Corresponding author
Łukasz Matuszewski
Klinika Ortopedii i Rehabilitacji Dziecięcej / Pediatric Orthopedic and Rehabilitation Department, Medical University of Lublin, Poland
Klinika Ortopedii i Rehabilitacji Dziecięcej / Pediatric Orthopedic and Rehabilitation Department, Medical University of Lublin, Poland
Ann Agric Environ Med. 2025;32(2):308-312
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
In spastic hemiparesis, upper extremity issues pose challenges for orthopaedic surgeons, neurologists, physiotherapists, and occupational therapists. Various interventions aim to decrease contractures, improve hand function, and enhance mobility. The aim of the study was evaluation of hand function after tendon transfer in spastic hemiparesis in cerebral palsy.
Material and methods:
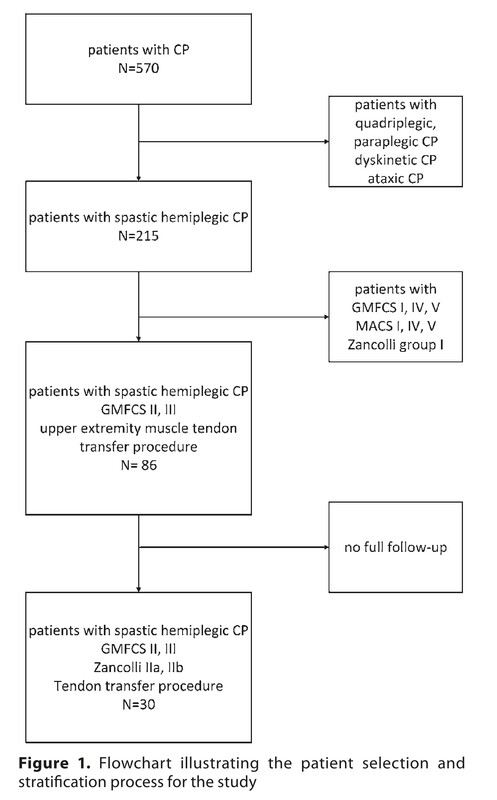
A retrospective review was performed of in- and outpatient charts (from 2006) across two centres: a referral facility for cerebral palsy and a paediatric orthopaedic clinic. Inclusion criteria was spastic hemiplegia of the upper limb, treated surgically with muscle transfer. Exclusion criteria were dystonia or other coordination disorders, bilateral involvement, or prior upper limb surgeries. Minimum follow-up – 2 years.
Results:
Thirty patients (14 females, 16 males) met the criteria; mean surgery age – 11.5 years (range 10–15). All were GMFCS II or III and MACS 2 or 3, with extrinsic-type hands per Zancolli (14 group 1, 10 group 2a, 6 group 2b). All initially underwent ray plasty, FCU-to-ECRL transfer, and pronator teres release. Two had biceps lengthening; one had finger flexor myotomy. All reported self-perceived functional gains (e.g., improved grasp, pencil holding, self-feeding), verified by therapists. Hand and forearm alignment improved without MACS classification change; function according to Zancolli classification improved.
Conclusions:
Muscle transfer surgery improved upper extremity position and function in spastic hemiplegic patients. The group for surgery has to be carefully selected. There is a need of standardization of reporting goals and outcomes in this selected population, as well as choosing the procedure required by an experienced team.
In spastic hemiparesis, upper extremity issues pose challenges for orthopaedic surgeons, neurologists, physiotherapists, and occupational therapists. Various interventions aim to decrease contractures, improve hand function, and enhance mobility. The aim of the study was evaluation of hand function after tendon transfer in spastic hemiparesis in cerebral palsy.
Material and methods:
A retrospective review was performed of in- and outpatient charts (from 2006) across two centres: a referral facility for cerebral palsy and a paediatric orthopaedic clinic. Inclusion criteria was spastic hemiplegia of the upper limb, treated surgically with muscle transfer. Exclusion criteria were dystonia or other coordination disorders, bilateral involvement, or prior upper limb surgeries. Minimum follow-up – 2 years.
Results:
Thirty patients (14 females, 16 males) met the criteria; mean surgery age – 11.5 years (range 10–15). All were GMFCS II or III and MACS 2 or 3, with extrinsic-type hands per Zancolli (14 group 1, 10 group 2a, 6 group 2b). All initially underwent ray plasty, FCU-to-ECRL transfer, and pronator teres release. Two had biceps lengthening; one had finger flexor myotomy. All reported self-perceived functional gains (e.g., improved grasp, pencil holding, self-feeding), verified by therapists. Hand and forearm alignment improved without MACS classification change; function according to Zancolli classification improved.
Conclusions:
Muscle transfer surgery improved upper extremity position and function in spastic hemiplegic patients. The group for surgery has to be carefully selected. There is a need of standardization of reporting goals and outcomes in this selected population, as well as choosing the procedure required by an experienced team.
REFERENCES (37)
1.
Miller MD, Thompson SR. Chapter 3:Cerebral Palsy. In: Miller’s Review of Orthopaedics. 8th ed. Elsevier; 2019. p. 824–840.
2.
Falisse A, Bar-On L, Desloovere K, et al. A spasticity model based on feedback from muscle force explains muscle activity during passive stretches and gait in children with cerebral palsy. PLoS One. 2018;13(12):e0208811. doi:10.1371/journal.pone.0208811.
3.
Howard JJ, Herzog W. Skeletal Muscle in Cerebral Palsy: From Belly to Myofibril. Front Neurol. 2021;12. doi:10.3389/fneur.2021.620852.
4.
Mowery CA, Gelberman RH, Rhoades CE. Upper Extremity Tendon Transfers in Cerebral Palsy. J Pediatric Orthopaed. 1985;5(1):69–72. doi:https://doi.org/10.1097/012413....
5.
Van Heest AE, Bagley A, Molitor F, et al. Tendon Transfer Surgery in Upper-Extremity Cerebral Palsy Is More Effective than Botulinum Toxin Injections or Regular, Ongoing Therapy. J Bone Joint Surg. 2015;97(7):529–536. doi:https://doi.org/10.2106/jbjs.m....
6.
Van Heest AE, House JH, Cariello C. Upper extremity surgical treatment of cerebral palsy. J Hand Surg. 1999;24(2):323–330. doi:10.1053/jhsu.1999.0323.
7.
Roth JH, O’Grady SE, Richards RS, et al. Functional outcome of upper limp tendon transfers performed in children with spastic hemiplegia. J Hand Surg British Eur Vol. 1993;18(3):299–303. doi:10.1016/0266-7681(93)90045-H.
8.
Eliasson AC, Ekholm C, Carlstedt T. Hand function in children with cerebral palsy after upper-limb tendon transfer and muscle release. Dev Med Child Neurol. 1998;40(9):612–621. doi:10.1111/j.1469-8749.1998.tb15427.x.
9.
Wagner LV, Davids JR. Assessment Tools and Classification Systems Used For the Upper Extremity in Children With Cerebral Palsy. Clin Orthop Related Res. 2012;470(5):1257–1271. doi:10.1007/s11999-011-2065-x.
10.
Zancolli EA, Zancolli ER. Surgical Management of the Hemiplegic Spastic Hand in Cerebral Palsy. Surg Clin North Am Practical Surg Hand. 1981; 61: 395–406. https://doi.org/10.1016/S0039-....
11.
Tranchida GV, Van Heest A. Preferred options and evidence for upper limb surgery for spasticity in cerebral palsy, stroke, and brain injury. J Hand Surg Eur Vol. 2020;45(1):34–42. doi:10.1177/1753193419878973.
12.
Vuillermin C. Management of Upper Extremity Manifestations of Cerebral Palsy. J Pediatric Orthop Soc North Am. 2022;4(2). doi:10.55275/JPOSNA-2022-0042.
13.
Choi JY, Rha DW, Kim SA, et al. The Dynamic Thumb-in-Palm Pattern in Children with Spastic Cerebral Palsy and Its Effects on Upper Limb Function. Children. 2021;8(1):17. doi:10.3390/children8010017.
14.
Alewijnse JV, Kreulen M, van Loon J, et al. Extensor pollicis longus rerouting for thumb-in-palm deformity in cerebral palsy: a biomechanical analysis. J Hand Surg Eur Vol. 2019;44(8):785–789. doi:10.1177/1753193419857067.
15.
Gerami H, Shahcheraghi GH, Javid M. Tendon transfer in spastic cerebral palsy upper limb. J Pediatric Orthop B. 2024;33(5):507–514. doi:10.1097/BPB.0000000000001137.
16.
Maskill L. Upper Extremity Surgery for Patients with Cerebral Palsy. In: Nowicki PD, editor. Orthopedic Care of Patients with Cerebral Palsy: A Clinical Guide to Evaluation and Management across the Lifespan. Springer International Publishing; 2020. p. 213–219. doi:10.1007/978-3-030-46574-2_10.
17.
Novak I, Morgan C, Fahey M, et al. State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy. Curr Neurol Neurosci Rep. 2020;20(2):3. doi:10.1007/s11910-020-1022-z.
18.
Trehan SK, Little KJ. Technical Pearls of Tendon Transfers for Upper Extremity Spasticity. Hand Clin. 2018;34(4):529–536. doi:10.1016/j.hcl.2018.06.009.
19.
Pontén E, von Walden F, Lenke-Ekholm C, et al. Outcome of hand surgery in children with spasticity – a 9-year follow-up study. J Pediatric Orthop B. 2019;28(4):301. doi:10.1097/BPB.0000000000000600.
20.
Sköld A, Josephsson S, Fitinghoff H, et al. Experiences of Use of the Cerebral Palsy Hemiplegic Hand in Young Persons Treated with Upper Extremity Surgery. J Hand Therapy. 2007;20(3):262–273. doi:10.1197/j.jht.2007.04.003.
21.
Gong HS, Chung CY, Park MS, et al. Functional Outcomes After Upper Extremity Surgery for Cerebral Palsy: Comparison of High and Low Manual Ability Classification System Levels. J Hand Surg. 2010;35(2):277–283.e3. doi:10.1016/j.jhsa.2009.10.028.
22.
Zancolli EA, Goldner LJ, Swanson AB. Surgery of the spastic hand in cerebral palsy: Report of the Committee on Spastic Hand Evaluation. J Hand Surg. 1983;8(5):766–772. doi:https://doi.org/10.1016/s0363-....
23.
Główny Urząd Statystyczny. Rocznik Statystyczny Rolnictwa. Published 2023. Accessed April 24, 2025. https://stat.gov.pl/download/g....
24.
Tseng SH, Lee JY, Chou YL. Association between socioeconomic status and cerebral palsy. PLOS ONE. 2018;13(1):e0191724. doi:https://doi.org/10.1371/journa....
25.
Bican R, Noritz G, Heathcock J. Children from rural Appalachia and urban communities are diagnosed with Cerebral Palsy significantly later than children from suburban communities. Arch Physical Med Rehabil. 2021;102(10):e18. doi:https://doi.org/10.1016/j.apmr....
26.
Hemachithra C, Meena N, Ramanathan R. Association of risk factors of cerebral palsy – a matched case control study. Inter J Physiother. 2020;7(2). doi:https://doi.org/10.15621/ijphy....
27.
Hedberg-Graff J, Granström F, Arner M, et al. Upper-limb contracture development in children with cerebral palsy: a population-based study. Develop Med Child Neuro. 2019;61(2):204–211. doi:10.1111/dmcn.14006.
28.
Louwers A, Warnink-Kavelaars J, Daams J, et al. Effects of upper extremity surgery on activities and participation of children with cerebral palsy: a systematic review. Dev Med Child Neurol. 2020;62(1):21–27. doi:10.1111/dmcn.14315.
29.
Van Heest AE, Ramachandran V, et al. Quantitative and Qualitative Functional Evaluation of Upper Extremity Tendon Transfers in Spastic Hemiplegia Caused by Cerebral Palsy. J Pediatric Orthop. 2008;28(6):679–683. doi:10.1097/bpo.0b013e3181831eac.
30.
Piscitelli D, Ferrarello F, Ugolini A, et al. Measurement properties of the Gross Motor Function Classification System, Gross Motor Function Classification System-Expanded & Revised, Manual Ability Classification System, and Communication Function Classification System in cerebral palsy: a systematic review with meta-analysis. Develop Med Child Neuro. 2021;63(11):1251–1261. doi:10.1111/dmcn.14910.
31.
Fitoussi F, Lallemant-Dudek P. The upper limb in children with cerebral palsy. Evaluation and treatment. Orthop Traumatol Surg Res. 2024;110(1):103763. doi:10.1016/j.otsr.2023.103763.
32.
Van Munster JC, Maathuis CG, Haga N, et al. Does surgical management of the hand in children with unilateral spastic cerebral palsy affect muscle coordination and quality of reaching? Develop Med Child Neurol. 2009;51(7):568–570. doi:10.1111/j.1469-8749.2009.03312.x.
33.
Louwers A, Warnink-Kavelaars J, Obdeijn M, et al. Effects of Upper-Extremity Surgery on Manual Performance of Children and Adolescents with Cerebral Palsy: A Multidisciplinary Approach Using Shared Decision-Making. JBJS. 2018;100(16):1416. doi:10.2106/JBJS.17.01382.
34.
Rutz E, Graham HK. Management of the Upper Limb in Cerebral Palsy. In: Panteliadis CP, editor. Cerebral Palsy: A Multidisciplinary Approach. Springer International Publishing; 2018:219–227. doi:10.1007/978-3-319-67858-0_21.
35.
Louwers A, Beelen A, Holmefur M, et al. Development of the Assisting Hand Assessment for adolescents (Ad-AHA) and validation of the AHA from 18 months to 18 years. Dev Med Child Neurol. 2017;58(12):1303–1309. doi:10.1111/dmcn.13168.
36.
Surveillance of Cerebral Palsy in Europe (SCPE), Johnson A (corresp.). Prevalence and Characteristics of Children with Cerebral Palsy in Europe. Develop Med Child Neurol. 2007;44(9):633–640. doi:https://doi.org/10.1111/j.1469....
37.
Brown JK, Van Rensburg F, Lakie GWM, et al. A neurological study of hand function of hemiplegic children. Develop Med Child Neurol. 1987;29(3):287–304. doi:10.1111/j.1469-8749.1987.tb02482.x.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.