Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Changes in body weight in various population groups in Poland during the COVID-19 pandemic – a comparison of two cross-sectional studies
1
Department of Humanization of Health Care and Sexology, Collegium Medicum, University of Zielona Góra, Poland
2
Faculty of Management, Warsaw University, Poland
3
Faculty of Medicine, Collegium Medicum, Cardinal Stefan Wyszyński University, Warsaw, Poland
4
Department of Biomedical Aspects of Development and Sexology, Faculty of Education, Warsaw, Poland
5
Faculty of Medicine, University of Warsaw, Poland
Corresponding author
Maciej Białorudzki
Department of Humanization of Health Care and Sexology, Collegium Medicum, University of Zielona Góra,, Energetyków 2, 65-729, Zielona Góra, Poland
Department of Humanization of Health Care and Sexology, Collegium Medicum, University of Zielona Góra,, Energetyków 2, 65-729, Zielona Góra, Poland
Ann Agric Environ Med. 2024;31(3):362-370
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The disruption of daily activities caused by the COVID-19 pandemic had health consequences, especially during peak lockdown periods. The aim of the study is to assess the impact of the first year of the COVID-19 pandemic on the process of weight change among Polish adults.
Material and methods:
Two representative studies involving Polish adults aged 18–65 years were conducted, the first in June 2020 (N = 2527, from the perspective of the last 2–3 months), and the second a year later, in June 2021 (N = 2087, covering the last 12 months). Both surveys included two groups of respondents, and conducted using the CAWI method – computer-assisted web interview.
Results:
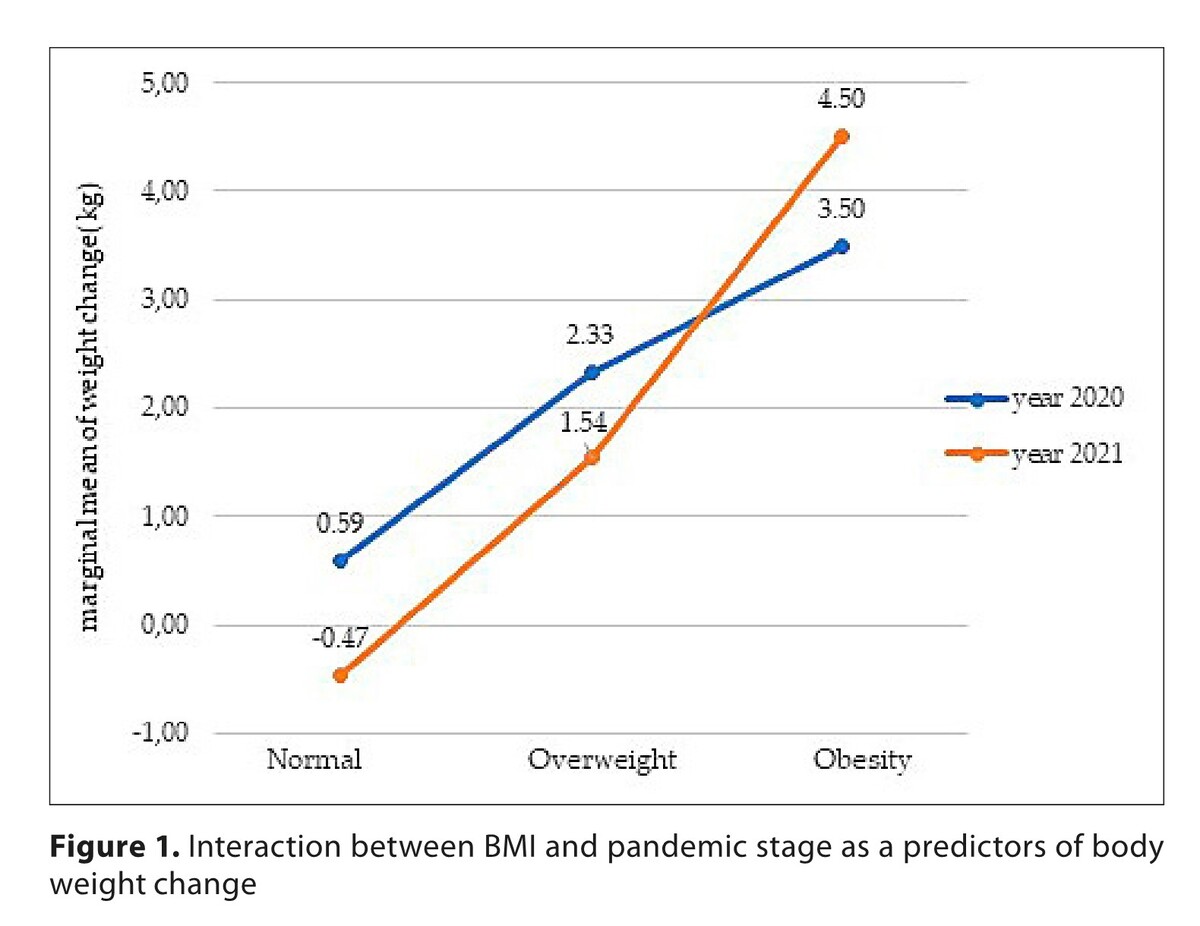
In the first period of the COVID-19 pandemic, there were more individuals with obesity than a year later (18.7% vs 19.9%), and more respondents reported weight change in 2020 than in 2021 (53% vs 49.6%). In both surveys, women were more likely to report weight gain than men (p<0.001). Statistically significant factors for weight change in 2020 and 2021 were gender, age, and in 2021, education and relationship status. Multinomial logistic regression showed that BMI, age of 18–29 and 30–49, being male, and education below high school, was significant for weight gain. While for weight loss, BMI, age 18–29 and 30–49, being male, and year of study, were statistically significant.
Conclusions:
The findings confirmed that body weight changed throughout the pandemic, depending on the time of the pandemic and selected socio-demographic factors.
The disruption of daily activities caused by the COVID-19 pandemic had health consequences, especially during peak lockdown periods. The aim of the study is to assess the impact of the first year of the COVID-19 pandemic on the process of weight change among Polish adults.
Material and methods:
Two representative studies involving Polish adults aged 18–65 years were conducted, the first in June 2020 (N = 2527, from the perspective of the last 2–3 months), and the second a year later, in June 2021 (N = 2087, covering the last 12 months). Both surveys included two groups of respondents, and conducted using the CAWI method – computer-assisted web interview.
Results:
In the first period of the COVID-19 pandemic, there were more individuals with obesity than a year later (18.7% vs 19.9%), and more respondents reported weight change in 2020 than in 2021 (53% vs 49.6%). In both surveys, women were more likely to report weight gain than men (p<0.001). Statistically significant factors for weight change in 2020 and 2021 were gender, age, and in 2021, education and relationship status. Multinomial logistic regression showed that BMI, age of 18–29 and 30–49, being male, and education below high school, was significant for weight gain. While for weight loss, BMI, age 18–29 and 30–49, being male, and year of study, were statistically significant.
Conclusions:
The findings confirmed that body weight changed throughout the pandemic, depending on the time of the pandemic and selected socio-demographic factors.
REFERENCES (54)
1.
Zachary Z, Brianna F, Brianna L, et al. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes Res Clin Pract. 2020;14(3):210–216. doi:10.1016/j.orcp.2020.05.004.
2.
Flanagan EW, Beyl RA, Fearnbach SN, Altazan AD, Martin CK, Redman LM. The Impact of COVID-19 Stay-At-Home Orders on Health Behaviors in Adults. Obesity (Silver Spring). 2021;29(2):438–445. doi:10.1002/oby.23066.
3.
Bhutani S, Cooper JA, vanDellen MR. Self-reported Changes in Energy Balance Behaviors during COVID-19-related Home Confinement: A Cross-sectional Study. Am J Health Behav. 2021;45(4):756–770. doi:10.5993/AJHB.45.4.14.
4.
Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12(6). doi:10.3390/nu12061583.
5.
World Health Organization. Available online: https://www.who.int/health-top... (access: 2023.11.14).
6.
Piaggi P. Metabolic Determinants of Weight Gain in Humans. Obesity (Silver Spring). 2019;27(5):691–699. doi:10.1002/oby.22456.
7.
Swinburn BA, Sacks G, Lo SK, et al. Estimating the changes in energy flux that characterize the rise in obesity prevalence. Am J Clin Nutr. 2009;89(6):1723–8. doi:10.3945/ajcn.2008.27061.
8.
Stuckler D, McKee M, Ebrahim S, Basu S. Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med. 2012;9(6):e1001235. doi:10.1371/journal.pmed.1001235.
9.
Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–14. doi:10.1016/S0140-6736(11)60813-1.
10.
Mendonça RD, Pimenta AM, Gea A, et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN) cohort study. Am J Clin Nutr. 2016;104(5):1433–1440. doi:10.3945/ajcn.116.135004.
11.
Bhutani S, vanDellen MR, Cooper JA. Longitudinal Weight Gain and Related Risk Behaviors during the COVID-19 Pandemic in Adults in the US. Nutrients. 2021;13(2). doi:10.3390/nu13020671.
12.
Moynihan AB, van Tilburg WA, Igou ER, Wisman A, Donnelly AE, Mulcaire JB. Eaten up by boredom: consuming food to escape awareness of the bored self. Front Psychol. 2015;6:369. doi:10.3389/fpsyg.2015.00369.
13.
Chao A, Grilo CM, White MA, Sinha R. Food cravings mediate the relationship between chronic stress and body mass index. J Health Psychol. 2015;20(6):721–9. doi:10.1177/1359105315573448.
14.
Opichka K, Smith C, Levine AS. Problematic Eating Behaviors Are More Prevalent in African American Women Who Are Overweight or Obese Than African American Women Who Are Lean or Normal Weight. Fam Community Health. 2019;42(2):81–89. doi:10.1097/FCH.0000000000000222.
15.
Błaszczyk-Bębenek E, Jagielski P, Bolesławska I, Jagielska A, Nitsch-Osuch A, Kawalec P. Nutrition Behaviors in Polish Adults before and during COVID-19 Lockdown. Nutrients. 2020;12(10). doi:10.3390/nu12103084.
16.
Batlle-Bayer L, Aldaco R, Bala A, et al. Environmental and nutritional impacts of dietary changes in Spain during the COVID-19 lockdown. Sci Total Environ. 2020;748:141410. doi:10.1016/j.scitotenv.2020.141410.
17.
Sidor A, Rzymski P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients. 2020;12(6). doi:10.3390/nu12061657.
18.
Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-Related School Closings and Risk of Weight Gain Among Children. Obesity (Silver Spring). 2020;28(6):1008–1009. doi:10.1002/oby.22813.
19.
Almandoz JP, Xie L, Schellinger JN, et al. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin Obes. 2020;10(5):e12386. doi:10.1111/cob.12386.
20.
Polidori D, Sanghvi A, Seeley RJ, Hall KD. How Strongly Does Appetite Counter Weight Loss? Quantification of the Feedback Control of Human Energy Intake. Obesity (Silver Spring). 2016;24(11):2289–2295. doi:10.1002/oby.21653.
21.
Hall KD, Kahan S. Maintenance of Lost Weight and Long-Term Management of Obesity. Med Clin North Am. 2018;102(1):183–197. doi:10.1016/j.mcna.2017.08.012.
22.
Loveman E, Frampton GK, Shepherd J, et al. The clinical effectiveness and cost-effectiveness of long-term weight management schemes for adults: a systematic review. Health Technol Assess. 2011;15(2):1–182. doi:10.3310/hta15020.
23.
Severin R, Sabbahi A, Mahmoud AM, Arena R, Phillips SA. Precision Medicine in Weight Loss and Healthy Living. Prog Cardiovasc Dis. 2019;62(1):15–20. doi:10.1016/j.pcad.2018.12.012.
24.
Wu T, Gao X, Chen M, van Dam RM. Long-term effectiveness of diet-plus-exercise interventions vs. diet-only interventions for weight loss: a meta-analysis. Obes Rev. 2009;10(3):313–23. doi:10.1111/j.1467-789X.2008.00547.x.
25.
Maclean PS, Bergouignan A, Cornier MA, Jackman MR. Biology’s response to dieting: the impetus for weight regain. Am J Physiol Regul Integr Comp Physiol. 2011;301(3):R581–600. doi:10.1152/ajpregu.00755.2010.
26.
Nordmo M, Danielsen YS. The challenge of keeping it off, a descriptive systematic review of high-quality, follow-up studies of obesity treatments. Obes Rev. 2020;21(1):e12949. doi:10.1111/obr.12949.
27.
Ross KM, Wing RR. “Memory bias” for recall of experiences during initial weight loss is affected by subsequent weight loss outcome. J Behav Med. 2018;41(1):130–137. doi:10.1007/s10865-017-9896-1.
28.
Kwasnicka D, Dombrowski SU, White M, Sniehotta F. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev. 2016;10(3):277–96. doi:10.1080/17437199.2016.1151372.
29.
Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25 Suppl 2):S102–38. doi:10.1161/01.cir.0000437739.71477.ee.
30.
Matheson EM, King DE, Everett CJ. Healthy lifestyle habits and mortality in overweight and obese individuals. J Am Board Fam Med. 2012;25(1):9–15. doi:10.3122/jabfm.2012.01.110164.
31.
Fontana L, Hu FB. Optimal body weight for health and longevity: bridging basic, clinical, and population research. Aging Cell. 2014;13(3):391–400. doi:10.1111/acel.12207.
32.
Chen C, Ye Y, Zhang Y, Pan XF, Pan A. Weight change across adulthood in relation to all cause and cause specific mortality: prospective cohort study. BMJ. 2019;367:l5584. doi:10.1136/bmj.l5584.
33.
Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity (Silver Spring). 2012;20(6):1234–9. doi:10.1038/oby.2011.140.
34.
Izdebski Z. Health and sexual life of Poles in 2017. Research study in the background since 1997. Wydawnictwo Uniwersytetu Warszawskiego, 2020.
35.
Pellegrini M, Ponzo V, Rosato R, et al. Changes in Weight and Nutritional Habits in Adults with Obesity during the “Lockdown” Period Caused by the COVID-19 Virus Emergency. Nutrients. 2020;12(7). doi:10.3390/nu12072016.
36.
Regulation of the Minister of Health of 20 March 2020 on the declaration of an epidemic in the territory of the Republic of Poland. (DzU z 2020 r. poz. 491). Polish. (access: 2023.11.14).
37.
Han E, Tan MMJ, Turk E, et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. 2020;396(10261):1525–1534. doi:10.1016/S0140-6736(20)32007-9.
38.
Khubchandani J, Price JH, Sharma S, Wiblishauser MJ, Webb FJ. COVID-19 pandemic and weight gain in American adults: A nationwide population-based study. Diabetes Metab Syndr. 2022;16(1):102392. doi:10.1016/j.dsx.2022.102392.
39.
Vogel M, Geserick M, Gausche R, et al. Age- and weight group-specific weight gain patterns in children and adolescents during the 15 years before and during the COVID-19 pandemic. Int J Obes (Lond). 2022;46(1):144–152. doi:10.1038/s41366-021-00968-2.
40.
Khan MA, Moverley Smith JE. “Covibesity,” a new pandemic. Obes Med. 2020;19:100282. doi:10.1016/j.obmed.2020.100282.
41.
Dymkowska-Malesa M, Swora-Cwynar E, Karczewski, J, et al. Stan odżywienia i skład ciała osób starszych jako przesłanki do stosowania żywienia dietetycznego. Forum Zaburzeń Metabolicznych. 2017;8(1):28–35.
42.
Statistics Poland. Health status of population in Poland in 2019. Statistics Poland, 2021.
43.
Wojtyniak B, Goryński P. Health status of Polish population and its determinants 2020. National Institute of Hygiene, 2020.
44.
Białorudzki M, Izdebski Z. Changes in the body mass of adult residents of rural and urban areas in the initial months of the COVID-19 pandemic vs. their mental, physical and sexual health. Ann Agric Environ Med. 2021;28(4):667–675. doi:10.26444/aaem/143561.
45.
Spinosa J, Christiansen P, Dickson JM, Lorenzetti V, Hardman CA. From Socioeconomic Disadvantage to Obesity: The Mediating Role of Psychological Distress and Emotional Eating. Obesity (Silver Spring). 2019;27(4):559–564. doi:10.1002/oby.22402.
46.
Caputo EL, Reichert FF. Studies of Physical Activity and COVID-19 During the Pandemic: A Scoping Review. J Phys Act Health. 2020;17(12):1275–1284. doi:10.1123/jpah.2020-0406.
47.
Zajacova A, Jehn A, Stackhouse M, Denice P, Ramos H. Changes in health behaviours during early COVID-19 and socio-demographic disparities: a cross-sectional analysis. Can J Public Health. 2020;111(6):953–962. doi:10.17269/s41997-020-00434-y.
48.
Amaro-Gahete FJ, Jurado-Fasoli L, De-la-O A, Gutierrez Á, Castillo MJ, Ruiz JR. Accuracy and Validity of Resting Energy Expenditure Predictive Equations in Middle-Aged Adults. Nutrients. 2018;10(11). doi:10.3390/nu10111635.
49.
Drywień ME, Hamulka J, Zielinska-Pukos MA, Jeruszka-Bielak M, Górnicka M. The COVID-19 Pandemic Lockdowns and Changes in Body Weight among Polish Women. A Cross-Sectional Online Survey PLifeCOVID-19 Study. Sustainability. 2020;12(18):7768. https://doi.org/10.3390/su1218....
50.
Cheikh Ismail L, Osaili TM, Mohamad MN, et al. Assessment of eating habits and lifestyle during the coronavirus 2019 pandemic in the Middle East and North Africa region: a cross-sectional study. Br J Nutr. 2021;126(5):757–766. doi:10.1017/S0007114520004547.
51.
Rogers NT, Waterlow NR, Brindle H, et al. Behavioral Change Towards Reduced Intensity Physical Activity Is Disproportionately Prevalent Among Adults With Serious Health Issues or Self-Perception of High Risk During the UK COVID-19 Lockdown. Front Public Health. 2020;8:575091. doi:10.3389/fpubh.2020.575091.
52.
Sobal J, Rauschenbach B, Frongillo EA. Marital status changes and body weight changes: a US longitudinal analysis. Soc Sci Med. 2003;56(7):1543–55. doi:10.1016/s0277-9536(02)00155-7.
53.
Martínez-de-Quel Ó, Suárez-Iglesias D, López-Flores M, Pérez CA. Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: A longitudinal study. Appetite. 2021;158:105019. doi:10.1016/j.appet.2020.105019.
54.
Olfert MD, Barr ML, Charlier CM, et al. Self-Reported vs. Measured Height, Weight, and BMI in Young Adults. Int J Environ Res Public Health. 2018;15(10):2216. Published 2018 Oct 11. doi:10.3390/ijerph15102216.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.