Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Body weight and assessment of sexual life – a cross-sectional study
1
Department of Humanization of Health Care and Sexology, Collegium Medicum, University of Zielona Góra, Poland
2
Department of Biomedical Aspects of Development and Sexology, Faculty of Education, Warsaw University, Warsaw,
Poland
Corresponding author
Maciej Bialorudzki
Department of Humanization of Health Care and Sexology, Collegium Medicum, University of Zielona Gora, 65-046 Zielona Góra, Licealna 9, 65-046, Zielona Gora, Poland
Department of Humanization of Health Care and Sexology, Collegium Medicum, University of Zielona Gora, 65-046 Zielona Góra, Licealna 9, 65-046, Zielona Gora, Poland
Ann Agric Environ Med. 2024;31(2):212-218
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Body weight can be one of the health effects affecting people’s well-being in its many aspects. The aim of the study was to assess the relationship between body weight and sexual life.
Material and methods:
In June 2020 a survey was conducted online on a nationwide representative group of 3,000 Poles. A year later, in June 2021thje survey was repeated on a nationwide representative group of 2,500 Poles. The data obtained from 4,266 respondents were then analyzed. Four proprietary questions were used to assess sexual life, based on which a 3-point scale was developed (2020 – α = 0.80, homogeneity 61%; 2021 – α = 0.77, homogeneity 64%).
Results:
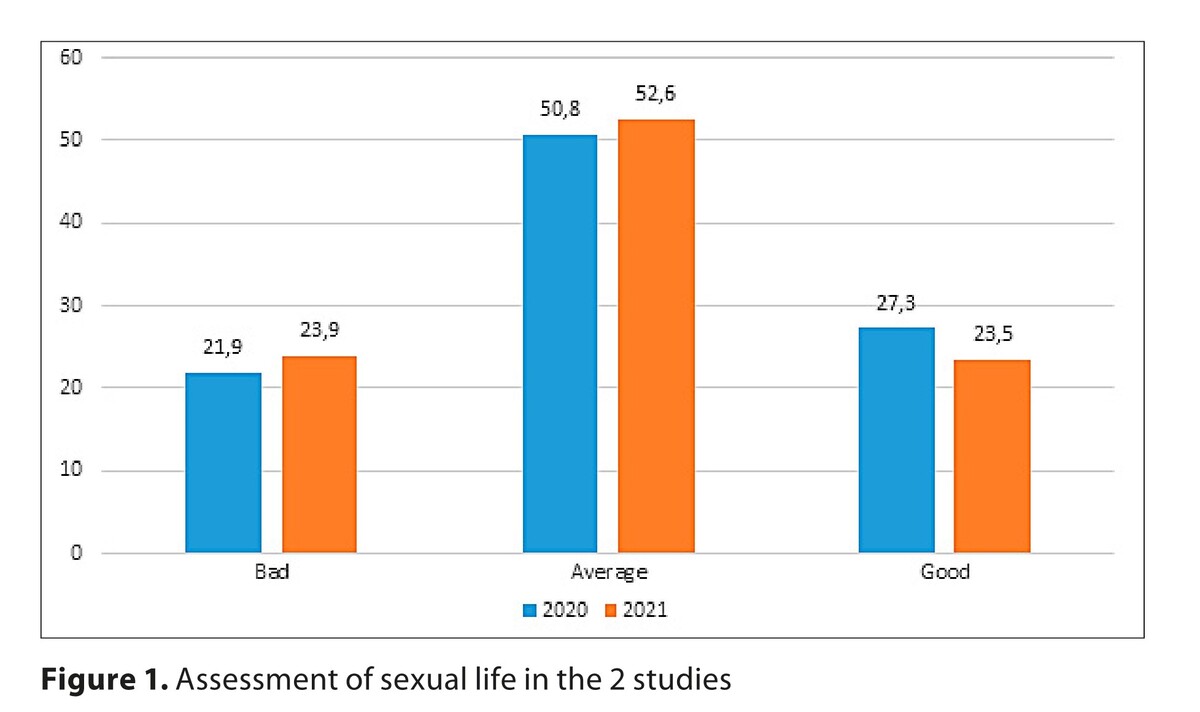
Excess body weight as measured by BMI was more common in 2021 than in 2020, which confirms the upward trend in body weight in society (55.5% vs. 52.7%). In 2020, more respondents indicated a good assessment of their sexual life than in 2021 (27.3% vs 23.5%, p=0.007). People with excessive body weight rated their sexual life as poorer on the scale (2020 p=0.003; 2021 p=0.009). Multinomial logistic regression showed that people with obesity (BMI>30) had a 1.7 higher increased risk of poor assessment of sexual life than those with normal weight (OR: 1.728; 95% CI: 1.396–2.138; p<0.001). In addition, multinomial logistic regression showed significance for the poor assessment of sexual life for the following factors: age 50–65; female. On the other hand, the following factors were associated with the good assessment of sexual life: age 18–29, being in a relationship, and the year of the study.
Conclusions:
Body weight may be one of the most important aspects affecting the assessment of a person’s sexual life. Educating patients about the correct body weight is extremely important in order to improve their health and sexual life.
Body weight can be one of the health effects affecting people’s well-being in its many aspects. The aim of the study was to assess the relationship between body weight and sexual life.
Material and methods:
In June 2020 a survey was conducted online on a nationwide representative group of 3,000 Poles. A year later, in June 2021thje survey was repeated on a nationwide representative group of 2,500 Poles. The data obtained from 4,266 respondents were then analyzed. Four proprietary questions were used to assess sexual life, based on which a 3-point scale was developed (2020 – α = 0.80, homogeneity 61%; 2021 – α = 0.77, homogeneity 64%).
Results:
Excess body weight as measured by BMI was more common in 2021 than in 2020, which confirms the upward trend in body weight in society (55.5% vs. 52.7%). In 2020, more respondents indicated a good assessment of their sexual life than in 2021 (27.3% vs 23.5%, p=0.007). People with excessive body weight rated their sexual life as poorer on the scale (2020 p=0.003; 2021 p=0.009). Multinomial logistic regression showed that people with obesity (BMI>30) had a 1.7 higher increased risk of poor assessment of sexual life than those with normal weight (OR: 1.728; 95% CI: 1.396–2.138; p<0.001). In addition, multinomial logistic regression showed significance for the poor assessment of sexual life for the following factors: age 50–65; female. On the other hand, the following factors were associated with the good assessment of sexual life: age 18–29, being in a relationship, and the year of the study.
Conclusions:
Body weight may be one of the most important aspects affecting the assessment of a person’s sexual life. Educating patients about the correct body weight is extremely important in order to improve their health and sexual life.
REFERENCES (63)
1.
Dai H, Alsalhe TA, Chalghaf N, Ricco M, Bragazzi NL, Wu J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: An analysis of the Global Burden of Disease Study. PLoS Med. 2020;17(7):e1003198. doi:10.1371/journal.pmed.1003198.
2.
Jaacks LM, Vandevijvere S, Pan A, et al. The obesity transition: stages of the global epidemic. Lancet Diabetes Endocrinol. 2019;7(3):231–240. doi:10.1016/S2213-8587(19)30026-9.
3.
Blomain ES, Dirhan DA, Valentino MA, Kim GW, Waldman SA. Mechanisms of Weight Regain following Weight Loss. ISRN Obes. 2013;2013:210524. doi:10.1155/2013/210524.
4.
World Health Organization: Obesity and overweight. https://www.who.int/news-room/... (access: 2023.06.28).
5.
Mayo Clinic. Obesity: Symptoms and Causes. https://www.mayoclinic.org/dis... (access: 2023.06.28).
6.
Truthmann J, Mensink GBM, Bosy-Westphal A, Hapke U, Scheidt-Nave C, Schienkiewitz A. Physical health-related quality of life in relation to metabolic health and obesity among men and women in Germany. Health Qual Life Outcomes. 2017;15(1):122. doi:10.1186/s12955-017-0688-7.
7.
Ng LH, Hart M, Dingle SE, et al. Prospective associations between diet quality and health-related quality of life in the Australian Diabetes, Obesity and Lifestyle (AusDiab) study. Br J Nutr. 2023;130(1):83–92. doi:10.1017/S000711452200304X.
8.
Jung FU, Luck-Sikorski C. Overweight and Lonely? A Representative Study on Loneliness in Obese People and Its Determinants. Obes Facts. 2019;12(4):440–447. doi:10.1159/000500095.
9.
Hunger JM, Major B, Blodorn A, Miller CT. Weighed down by stigma: How weight-based social identity threat contributes to weight gain and poor health. Soc Personal Psychol Compass. 2015;9(6):255–268. doi:10.1111/spc3.12172.
10.
Scully T, Ettela A, LeRoith D, Gallagher EJ. Obesity, Type 2 Diabetes, and Cancer Risk. Front Oncol. 2020;10:615375. doi:10.3389/fonc.2020.615375.
11.
Kitahara CM, Flint AJ, Berrington de Gonzalez A, et al. Association between class III obesity (BMI of 40–59 kg/m 2 ) and mortality: a pooled analysis of 20 prospective studies. PLoS Med. 2014;11(7):e1001673. doi:10.1371/journal.pmed.1001673.
12.
World Health Organization. Sexual health. https://www.who.int/health-top... (access: 2023.06.28).
13.
Epstein S, Mamo L. The proliferation of sexual health: Diverse social problems and the legitimation of sexuality. Soc Sci Med. 2017;188:176–190. doi:10.1016/j.socscimed.2017.06.033.
14.
Mollaioli D, Sansone A, Ciocca G, et al. Benefits of Sexual Activity on Psychological, Relational, and Sexual Health During the COVID-19 Breakout. J Sex Med. 2021;18(1):35–49. doi:10.1016/j.jsxm.2020.10.008.
15.
Michielsen K, Larrson EC, Kagesten A, et al. International Sexual Health And REproductive health (I-SHARE) survey during COVID-19: study protocol for online national surveys and global comparative analyses. Sex Transm Infect. 2021;97(2):88–92. doi:10.1136/sextrans-2020-054664.
16.
Masoudi M, Maasoumi R, Bragazzi NL. Effects of the COVID-19 pandemic on sexual functioning and activity: a systematic review and meta-analysis. BMC Public Health. 2022;22(1):189. doi:10.1186/s12889-021-12390-4.
17.
Izdebski Z, Słowikowska-Hilczer J, Mazur J. The Effect of the COVID-19 Pandemic on the Assessment of Sexual Life-Repeated Cross-Sectional Surveys among Polish Adults in 2017, 2020 and 2021. Int J Environ Res Public Health. 2022;19(7). doi:10.3390/ijerph19074110.
18.
Jannini EA, Limoncin E, Ciocca G, Buehler S, Krychman M. Ethical aspects of sexual medicine. Internet, vibrators, and other sex aids: toys or therapeutic instruments? J Sex Med. 2012;9(12):2994–3001. doi:10.1111/jsm.12018.
19.
Jannini EA. SM = SM: The Interface of Systems Medicine and Sexual Medicine for Facing Non-Communicable Diseases in a Gender-Dependent Manner. Sex Med Rev. 2017;5(3):349–364. doi:10.1016/j.sxmr.2017.04.002.
20.
Bialorudzki M. Sex and dietetics. What do dietetics and sexology have in common?, In: Kowalewska A, Waz K, Bialorudzki M, editors. Od seksualności do humanizacji medycyny. Benefis Zbigniewa Izdebskiego słowem pisany. Warsaw: Wydawnictwo Uniwersytetu Warszawskiego; 2022. p. 155—165.
21.
Mollaioli D, Ciocca G, Limoncin E, et al. Lifestyles and sexuality in men and women: the gender perspective in sexual medicine. Reprod Biol Endocrinol. 2020;18(1):10. doi:10.1186/s12958-019-0557-9.
22.
Corona G, Ricca V, Bandini E, et al. SIEDY scale 3, a new instrument to detect psychological component in subjects with erectile dysfunction. J Sex Med. 2012;9(8):2017–26. doi:10.1111/j.1743-6109.2012.02762.x.
23.
Harvey I, Boudreau A, Stephens JM. Adipose tissue in health and disease. Open Biol. 2020;10(12):200291. doi:10.1098/rsob.200291.
24.
Rowland DL, McNabney SM, Mann AR. Sexual Function, Obesity, and Weight Loss in Men and Women. Sex Med Rev. 2017;5(3):323–338. doi:10.1016/j.sxmr.2017.03.006.
25.
Sarwer DB, Steffen KJ. Quality of Life, Body Image and Sexual Functioning in Bariatric Surgery Patients. Eur Eat Disord Rev. 2015;23(6):504–8. doi:10.1002/erv.2412.
26.
Limoncin E, Ciocca G, Mollaioli D, Jannini EA. Sexual distress in obesity. In: Lenzi A, Migliaccio S, Donini L, editors. Multidisciplinary approach to obesity. Cham: Springer International Publishing; 2015. pp. 145–153.
27.
Larsen SH, Wagner G, Heitmann BL. Sexual function and obesity. Int J Obes (Lond). 2007;31(8):1189–98. doi:10.1038/sj.ijo.0803604.
28.
Rowland DL, McNabney SM, Mann AR. Sexual Function, Obesity, and Weight Loss in Men and Women. Sex Med Rev. 2017;5(3):323–33.
29.
Bates JN, Pastuszak AW, Khera M. Effect of Body Weight on Sexual Function in Men and Women. Curr Sex Health Rep. 2019;11(1):52–59.
30.
Cain MK, Zhang Z, Yuan KH. Univariate and multivariate skewness and kurtosis for measuring nonnormality: Prevalence, influence and estimation. Behav Res Methods. 2017;49(5):1716–1735. doi:10.3758/s13428-016-0814-1.
31.
Izdebski Z. Health and Sexual Life of Poles in 2017. Research Study in the Background since 1997. Warsaw: Wydawnictwo Uniwersytetu Warszawskiego; 2020.
32.
Izdebski Z. Sexuality of Poles at the Beginning of the 21st Century. A research study. Cracow: Wydawnictwo Uniwersytetu Jagiellońskiego; 2012.
33.
Han E, Tan MMJ, Turk E, et al. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. 2020;396(10261):1525–1534. doi:10.1016/S0140-6736(20)32007-9.
34.
Khubchandani J, Price JH, Sharma S, Wiblishauser MJ, Webb FJ. COVID-19 pandemic and weight gain in American adults: A nationwide population-based study. Diabetes Metab Syndr. 2022;16(1):102392. doi:10.1016/j.dsx.2022.102392.
35.
Vogel M, Geserick M, Gausche R, et al. Age- and weight group-specific weight gain patterns in children and adolescents during the 15 years before and during the COVID-19 pandemic. Int J Obes (Lond). 2022;46(1):144–152. doi:10.1038/s41366-021-00968-2.
36.
Li W, Li G, Xin C, Wang Y, Yang S. Challenges in the Practice of Sexual Medicine in the Time of COVID-19 in China. J Sex Med. 2020;17(7):1225–1228. doi:10.1016/j.jsxm.2020.04.380.
37.
Białorudzki M, Izdebski Z. Changes in the body mass of adult residents of rural and urban areas in the initial months of the COVID-19 pandemic vs. their mental, physical and sexual health. Ann Agric Environ Med. 2021;28(4):667–675. doi:10.26444/aaem/143561.
38.
Faubion SS, Fairbanks F, Kuhle CL, et al. Association Between Body Mass Index and Female Sexual Dysfunction: A Cross-sectional Study from the Data Registry on Experiences of Aging, Menopause, and Sexuality. J Sex Med. 2020;17(10):1971–1980. doi:10.1016/j.jsxm.2020.07.004.
39.
Ferrández Infante A, Novella Arribas B, Khan KS, et al. Obesity and female sexual dysfunctions: A systematic review of prevalence with meta-analysis. Semergen. 2023;49(7):102022. doi:10.1016/j.semerg.2023.102022.
40.
Towe M, La J, El-Khatib F, Roberts N, Yafi FA, Rubin R. Diet and Female Sexual Health. Sex Med Rev. 2020;8(2):256–264. doi:10.1016/j.sxmr.2019.08.004.
41.
Pierzak M, Głuszek S. The effect of weight reduction on the sexual function and reproductive health of obese men. Medical Studies/Studia Medyczne. 2022;38(3):233–244. doi:10.5114/ms.2022.119923.
42.
Moore RH, Sarwer DB, Lavenberg JA, et al. Relationship between sexual function and quality of life in obese persons seeking weight reduction. Obesity (Silver Spring). 2013;21(10):1966–74. doi:10.1002/oby.20398.
43.
Kessler A, Sollie S, Challacombe B, Briggs K, Van Hemelrijck M. The global prevalence of erectile dysfunction: a review. BJU Int. 2019;124(4):587–599. doi:10.1111/bju.14813.
44.
Milhausen RR, Buchholz AC, Opperman EA, Benson LE. Relationships Between Body Image, Body Composition, Sexual Functioning, and Sexual Satisfaction Among Heterosexual Young Adults. Arch Sex Behav. 2015;44(6):1621–33. doi:10.1007/s10508-014-0328-9.
45.
Salari N, Hasheminezhad R, Sedighi T, Zarei H, Shohaimi S, Mohammadi M. The global prevalence of sexual dysfunction in obese and overweight women: a systematic review and meta-analysis. BMC Womens Health. 2023;23(1):375. doi:10.1186/s12905-023-02544-4.
46.
Esfahani SB, Pal S. Obesity, mental health, and sexual dysfunction: A critical review. Health Psychol Open. 2018;5(2):2055102918786867. doi:10.1177/2055102918786867.
47.
Ramsey LR, Marotta JA, Hoyt T. Sexualized, objectified, but not satisfied: Enjoying sexualization relates to lower relationship satisfaction through perceived partner-objectification. J Soc Pers Relat. 2017;34(2), 258 278. doi:10.1177/0265407516631157.
48.
Jagstaidt V, Golay A, Pasini W. Relationships between sexuality and obesity in male patients. New Trends Exp Clin Psychiatry 1997;13:105–110.
49.
Kim JJ, Muise A, Barranti M, Mark KP, Rosen NO, Harasymchuk C, Impett E. Are Couples More Satisfied When They Match in Sexual Desire? New Insights From Response Surface Analyses. Soc Psychol Pers Sci. 2021;12(4):487–496. doi:10.1177/1948550620926770.
50.
Sutherland SE, Rehman US, Fallis EE, Goodnight JA. Understanding the phenomenon of sexual desire discrepancy in couples. Can J Hum Sex. 2015;24(2):141–150. doi:10.3138/cjhs.242.A3.
51.
Fuchs A, Matonóg A, Pilarska J, et al. The Impact of COVID-19 on Female Sexual Health. Int J Environ Res Public Health. 2020;17(19)doi:10.3390/ijerph17197152.
52.
Pauls RN, Occhino JA, Dryfhout VL. Effects of pregnancy on female sexual function and body image: a prospective study. J Sex Med. 2008;5(8):1915–22. doi:10.1111/j.1743-6109.2008.00884.x.
53.
Seal BN, Bradford A, Meston CM. The association between body esteem and sexual desire among college women. Arch Sex Behav. 2009;38(5):866–72. doi:10.1007/s10508-008-9467-1.
54.
Sanchez DT, Kiefer AK. Body concerns in and out of the bedroom: implications for sexual pleasure and problems. Arch Sex Behav. 2007;36(6):808–20. doi:10.1007/s10508-007-9205-0.
55.
Hamilton LD, Meston CM. Chronic stress and sexual function in women. J Sex Med. 2013;10(10):2443–54. doi:10.1111/jsm.12249.
56.
Wang C, Pan R, Wan X, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17(5). doi:10.3390/ijerph17051729.
57.
Rosen RC, Bachmann GA. Sexual well-being, happiness, and satisfaction, in women: the case for a new conceptual paradigm. J Sex Marital Ther. 2008;34(4):291–7; discussion 298–307. doi:10.1080/00926230802096234.
58.
Ballester-Arnal R, Nebot-Garcia JE, Ruiz-Palomino E, Giménez-García C, Gil-Llario MD. “INSIDE” Project on Sexual Health in Spain: Sexual Life During the Lockdown Caused by COVID-19. Sex Res Social Policy. 2021;18(4):1023–1041. doi:10.1007/s13178-020-00506-1.
59.
Lee DM, Nazroo J, O’Connor DB, Blake M, Pendleton N. Sexual Health and Well-being Among Older Men and Women in England: Findings from the English Longitudinal Study of Ageing. Arch Sex Behav. 2016;45(1):133–44. doi:10.1007/s10508-014-0465-1.
60.
Izdebski Z. Sexual health and life of Poles aged 50–74 in 2017. A perspective of ageing society. Warsaw: Wydawnictwo Uniwersytetu Warszawskiego; 2021.
61.
Buczak-Stec E, König HH, Hajek A. Sexual satisfaction of middle-aged and older adults: longitudinal findings from a nationally representative sample. Age Ageing. 2021;50(2):559–564. doi:10.1093/ageing/afaa161.
62.
Estill A, Mock SE, Schryer E, Eibach RP. The Effects of Subjective Age and Aging Attitudes on Mid- to Late-Life Sexuality. J Sex Res. 2018;55(2):146–151. doi:10.1080/00224499.2017.1293603.
63.
Traczyk I, Kucharska A, Sińska BI, et al. Every second adult inhabitant of Poland (aged 18–64) is overweight – results of representative cross-sectional studies conducted in 2017–2020. Ann Agric Environ Med. 2023;30(2):322–330. doi:10.26444/aaem/165913.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.