Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Shift work, body mass index and associated breast cancer risks in postmenopausal women
1
Medical University, Łódź, Poland
2
University of Łódź, Poland
Corresponding author
Ann Agric Environ Med. 2023;30(4):699-704
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Shift work increases the risk of breast cancer, but the mechanisms is still under discussion. This study evaluates the relationship between breast cancer and shift work on the basis of overweight and obesity among postmenopausal women.
Material and methods:
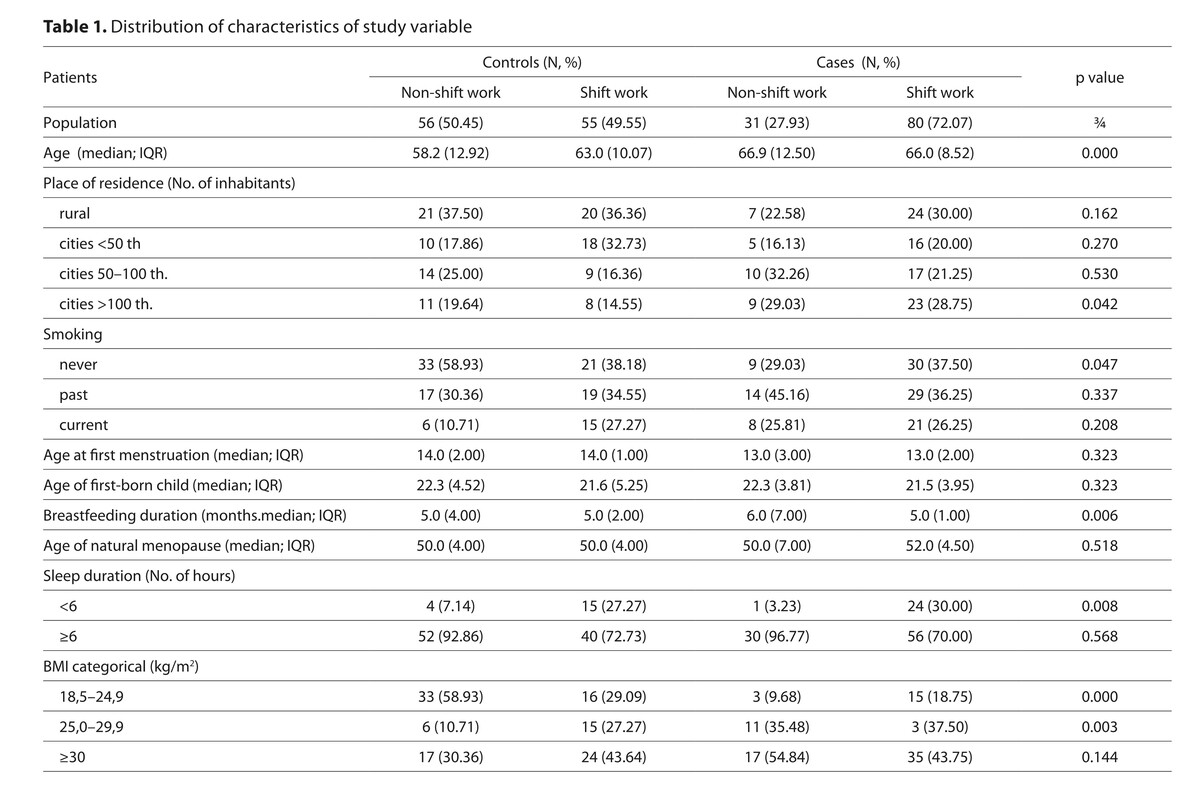
We examined this association using data from a case–control study carried between 2015 and 2019. The study involved 111 postmenopausal women with breast cancer and the same number of control participants. A self-reporting questionnaire was used for data collection. Multivariate logistic regression was conducted to find correlations between variables and determine the strength of relationships.
Results:
A 2.65-fold risk of breast cancer (OR=2.65; 95% CI: 1.34–5.22) was found among shift work women, compared with postmenopausal women not performing shift work. The association was modified by body mass index, showing a risk rate 9.84 times higher (OR=9.84; 95% CI: 2.14–45.19) among shift work and overweight women, compared to non-overweight women who had never been shift workers.
Conclusions:
About 49% of controls and 72% of cases had ever worked in a job that required shift work. The risk of breast cancer in postmenopausal women is associated with shift work, especially among overweight women. Some preventive measures to reduce the risk of breast cancer, in particular regarding a healthy lifestyle and weight control in this group of working women, should be implemented.
Shift work increases the risk of breast cancer, but the mechanisms is still under discussion. This study evaluates the relationship between breast cancer and shift work on the basis of overweight and obesity among postmenopausal women.
Material and methods:
We examined this association using data from a case–control study carried between 2015 and 2019. The study involved 111 postmenopausal women with breast cancer and the same number of control participants. A self-reporting questionnaire was used for data collection. Multivariate logistic regression was conducted to find correlations between variables and determine the strength of relationships.
Results:
A 2.65-fold risk of breast cancer (OR=2.65; 95% CI: 1.34–5.22) was found among shift work women, compared with postmenopausal women not performing shift work. The association was modified by body mass index, showing a risk rate 9.84 times higher (OR=9.84; 95% CI: 2.14–45.19) among shift work and overweight women, compared to non-overweight women who had never been shift workers.
Conclusions:
About 49% of controls and 72% of cases had ever worked in a job that required shift work. The risk of breast cancer in postmenopausal women is associated with shift work, especially among overweight women. Some preventive measures to reduce the risk of breast cancer, in particular regarding a healthy lifestyle and weight control in this group of working women, should be implemented.
ACKNOWLEDGEMENTS
This research was supported by the funds for the development
of young researchers and Ph.D. students at the Medical
University of Lodz (502-03/6-024-0/502-64-100-18) and co-
financed by Medical University of Lodz (503/6-024-01/503-
66-001 and 503/6-024-01/503-61-001-19-00).
REFERENCES (38)
1.
Kispert S, McHowat J. Recent insights into cigarette smoking as a lifestyle risk factor for breast cancer. Breast Cancer. 2017;7(9):127–132.
2.
Daly AA, Rolph R, Cutress RI, et al. A Review of Modifiable Risk Factors in Young Women for the Prevention of Breast Cancer. Breast Cancer. 2021;13:241–257.
3.
Feglia F, Collatuzzo G, Boffetta P. Occupational Cancers among Employed Women: A Narrative Review. Cancers (Basel). 2023;15(4):1334.
4.
Fenga C. Occupational exposure and risk of breast cancer. Biomed Rep. 2016;4:282–292.
5.
Briguglio G, Costa C, Teodoro M, et al. Women’s health and night shift work: Potential targets for future strategies in breast cancer (Review). Biomed Rep. 2021;15(6):98.
6.
IARC. IARC Monographs on the evaluation of carcinogenic risks to humans, In: Vol. 98. Painting, firefighting, and shiftwork. Lyon, France: International Agency for Research on Cancer; 2010.
7.
IARC. IARC Monographs on the Identification of Carcinogenic Hazards to Humans. Night shift work. Lyon, France: International Agency for Research on Cancer; 2020.
8.
Hong J, He Y, Fu R, et al. The relationship between night shift work and breast cancer incidence: A systematic review and meta-analysis of observational studies. Open Me (Wars). 2022;17(1):712–731.
9.
Liu Q, Shi J, Duan P, et al. Is shift work associated with a higher risk of overweight or obesity? A systematic review of observational studies with meta-analysis. Int J Epidemiol. 2018;47:1956–1971.
10.
Stevens RG. Electric power use and breast cancer: A hypothesis. Am J Epidemiol. 1987; 125:556–561.
11.
Cordina-Duverger E, Koudou Y, Truong T, et al. Night work and breast cancer risk defined by human epidermal growth factor receptor-2 (HER2) and hormone receptor status: A population-based case-control study in France. Chronobiol Int. 2016;33(6):783–787.
12.
Lie JA, Kjuus H, Zienolddiny S, et al. Breast cancer among nurses: is the intensity of night work related to hormone receptor status? Am J Epidemiol. 2013;178(1):110–117.
13.
Pedersen JE, Hansen J. Employment and risk of female breast cancer in Denmark. Am J Ind Med. 2022;65(5):343–356.
14.
Hansen J. Night Shift Work and Risk of Breast Cancer. Curr Environ Health Rep. 2017;4(3):325–339.
15.
Fagundo-Rivera J, Allande-Cussó R, Ortega-Moreno M, et al. Implications of Lifestyle and Occupational Factors on the Risk of Breast Cancer in Shiftwork Nurses. Healthcare (Basel). 2021;9(6):649.
16.
Cordina-Duverger E, Menegaux F, Popa A, et al. Night shift work and breast cancer: a pooled analysis of population-based case-control studies with complete work history. Eur J Epidemiol. 2018;33(4):369–379.
17.
Papantoniou K, Castano-Vinyals G, Espinosa A, et al. Breast cancer risk and night shift work in a case-control study in a Spanish population. Eur J Epidemiol. 2016;31(9):867–878.
18.
Manouchehri E, Taghipour A, Ghavami V, et al. Night-shift work duration and breast cancer risk: an updated systematic review and meta-analysis. BMC Womens Health. 2021;21(1):89.
19.
Pesch B, Harth V, Rabstein S, et al. Night work and breast cancer – results from the German GENICA study. Scand J Work Environ Health. 2010;36(2):134–141.
20.
Vlahoyiannis A, Karali E, Giannaki CD, et al. The vicious circle between physical, psychological, and physiological characteristics of shift work in nurses: a multidimensional approach. Sleep Breath. 2022;26(1):149–156.
21.
Peplońska B, Bukowska A, Sobala W. Association of Rotating Night Shift Work with BMI and Abdominal Obesity among Nurses and Midwives. PLoS One. 2015;10(7):e0133761.
22.
Zhang Q, Chair SY, Lo SHS, et al. Association between shift work and obesity among nurses: A systematic review and meta-analysis. Int J Nurs Stud. 2020;112:103757.
23.
Liu Q, Shi J, Duan P, et al. Is shift work associated with a higher risk of overweight or obesity? A systematic review of observational studies with meta-analysis. Int J Epidemiol. 2018;47(6):1956–1971.
24.
Grundy A, Cotterchio M, Kirsh VA, et al. Rotating shift work associated with obesity in men from northeastern Ontario. Health Promot Chronic Dis Prev Can. 2017;37(8):238–247.
25.
Macagnan J, Pattussi MP, Canuto R, et al. Impact of nightshift work on overweight and abdominal obesity among workers of a poultry processing plant in southern Brazil. Chronobiol Int. 2012;29(3):336–343.
26.
Vainio H, Bianchini F. IARC Handbooks of Cancer Prevent–Weight Control and Physical Activity. Lyon, France: International Agency for Research on Cancer; 2020.
27.
Lauby-Secretan B, Scoccianti C, Loomis D, et al. Body Fatness and Cancer-Viewpoint of the IARC Working Group. N Engl J Med. 2016;375(8):794–780.
28.
Park B. Changes in weight and waist circumference during menopausal transition and postmenopausal breast cancer risk. Int J Cancer. 2022;150(9):1431–1438.
29.
Chung GKK., Yeo W, Cheng A, et al. Prognostic significance of abdominal obesity and its post-diagnosis change in a Chinese breast cancer cohort. Breast Cancer Res Treat. 2022;193(3):649–658.
30.
Asaduzzaman M, Zannat IA, Akhtar PS, et al. Relation of Obesity with Breast Cancer among the Patients Attending at National Institute of Cancer Research & Hospital. Mymensingh Med J. 2020;29(3):676–683.
31.
Nagrani R, Mhatre S, Rajaraman P, et al. Central obesity increases risk of breast cancer irrespective of menopausal and hormonal receptor status in women of South Asian Ethnicity. Eur J Cancer. 2016; 66:153–161.
32.
Petrelli JM, Calle EE, Rodriguez C, et al. Body mass index, height and postmenopausal breast cancer mortality in a prospective cohort of US women. Cancer Causes Control. 2002;13:325–332.
33.
Yumuk PF, Dane F, Yumuk VD, et al. Impact of body mass index on cancer development. J BUON. 2008;13:55–59.
34.
Wang J, Yang DL, Chen ZZ, et al. Associations of body mass index with cancer incidence among populations, genders, and menopausal status: A systematic review and meta-analysis. Cancer Epidemiol. 2016;42:1–8.
35.
De Santi M, Annibalini G, Marano G, et al. Association between metabolic syndrome, insulin resistance, and IGF-1 in breast cancer survivors of DIANA-5 study. J Cancer Res Clin Oncol. 2023.
36.
Parasiliti-Caprino M, Bollati M, Merlo FD, et al. Adipose Tissue Dysfunction in Obesity: Role of Mineralocorticoid Receptor. Nutrients. 2022;9;14(22):4735.
37.
Moloney JN, Cotter TG. ROS signalling in the biology of cancer. Semin Cell Dev Biol. 2018;80:50–64.
38.
Naaman SC, Shen S, Zeytinoglu M, Iyengar NM. Obesity and Breast Cancer Risk: The Oncogenic Implications of Metabolic Dysregulation. J Clin Endocrinol Metab. 2022;107(8):2154–2166.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.