Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
COVID 19 – Possible interrelations with respiratory comorbidities caused by occupational exposure to various hazardous bioaerosols. Part II. Clinical course, diagnostics, treatment and prevention
1
Department of Pneumonology, Oncology and Allergology, Medical University, Lublin, Poland
2
Department of Medical Biology, Institute of Rural Health, Lublin, Poland
3
Department of Biological Health Hazards and Parasitology, Institute of Rural Health, Lublin, Poland
Corresponding author
Barbara Mackiewicz
Department of Pneumonology, Oncology and Allergology, Medical University, Lublin, Jaczewskiego 8, 20-954, Lublin, Poland
Department of Pneumonology, Oncology and Allergology, Medical University, Lublin, Jaczewskiego 8, 20-954, Lublin, Poland
Ann Agric Environ Med. 2021;28(1):27-43
KEYWORDS
SARS-CoV-2COVID-19clinical coursediagnosticstherapypreventioncomorbiditiesbioaerosolshypersensitivity pneumonitisODTS
TOPICS
ABSTRACT
Introduction and objective:
The course of COVID-19 caused by the SARS-CoV-2 may be aggravated by bioaerosols containing other viruses, bacteria, and fungi, occurring mainly in the occupational environment. Hence, the diagnostics and treatment of COVID-19 should address such a possibility in the anamnesis, treatment and final recommendations for avoiding of adverse exposure.
Abbreviated description of the state of knowledge:
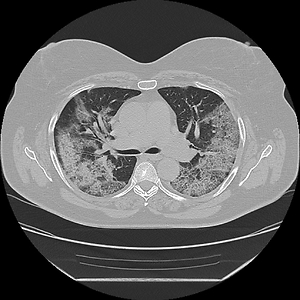
As SARS-CoV-2 attacks primarily the respiratory system and the severe manifestation of COVID-19 is interstitial pneumonia, diagnostics should include the following clinical and laboratory examinations: chest X-ray; high resolution computed tomography (HRCT); pulmonary function tests; arterial-blood gas test; genetic tests for the presence of SARS-CoV-2, in the future with the use of highly specific and sensitive nano-based biosensors; tests for the presence of specific immunity against the antigens of microorganisms causing other infectious or allergic pulmonary diseases (in the case of anamnestic indications). Because an universally accepted treatment for COVID-19 does not exist, the hitherto prescribed antiviral and immune-modulating drugs should be used be with caution. In many cases, a better alternative could be a safe supportive therapy, such as supplementation of the diet with probiotics, prebiotics, vitamins and microelements.
Summary:
The most important preventive measures against COVID-19 should include: vaccination; the use of filter or surgical masks; disinfection and sterilization; maintaining of well-functioning ventilation and air conditioning systems; reduction of the community air pollution which has been identified as an important factor increasing the COVID-19 severity. In the choice of preventive measures, the above should be considered for their potential efficacy against other bioaerosols as potential disease-aggravating agents.
The course of COVID-19 caused by the SARS-CoV-2 may be aggravated by bioaerosols containing other viruses, bacteria, and fungi, occurring mainly in the occupational environment. Hence, the diagnostics and treatment of COVID-19 should address such a possibility in the anamnesis, treatment and final recommendations for avoiding of adverse exposure.
Abbreviated description of the state of knowledge:
As SARS-CoV-2 attacks primarily the respiratory system and the severe manifestation of COVID-19 is interstitial pneumonia, diagnostics should include the following clinical and laboratory examinations: chest X-ray; high resolution computed tomography (HRCT); pulmonary function tests; arterial-blood gas test; genetic tests for the presence of SARS-CoV-2, in the future with the use of highly specific and sensitive nano-based biosensors; tests for the presence of specific immunity against the antigens of microorganisms causing other infectious or allergic pulmonary diseases (in the case of anamnestic indications). Because an universally accepted treatment for COVID-19 does not exist, the hitherto prescribed antiviral and immune-modulating drugs should be used be with caution. In many cases, a better alternative could be a safe supportive therapy, such as supplementation of the diet with probiotics, prebiotics, vitamins and microelements.
Summary:
The most important preventive measures against COVID-19 should include: vaccination; the use of filter or surgical masks; disinfection and sterilization; maintaining of well-functioning ventilation and air conditioning systems; reduction of the community air pollution which has been identified as an important factor increasing the COVID-19 severity. In the choice of preventive measures, the above should be considered for their potential efficacy against other bioaerosols as potential disease-aggravating agents.
REFERENCES (111)
1.
Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, et al. Coronavirus disease 2019–COVID-19. Clin Microbiol Rev. 2020; 33(4): e00028–20. doi: 10.1128/CMR.00028-20.
2.
Worldometers. Coronavirus statistics. https://www.worldometers.info/..., last accessed on 14 February 2021.
3.
Chams N, Chams S, Badran R, Shams A, Araji A, Raad M, et al. COVID-19: A multidisciplinary review. Front Public Health. 2020; 8: 383. doi: 10.3389/fpubh.2020.00383.
4.
Sanchez-Gonzalez MA, Moskowitz D, Issuree PD, Yatzkan G, Rizvi SA, Day K. A Pathophysiological perspective on COVID-19’s lethal complication: from viremia to hypersensitivity pneumonitis-like immune dysregulation. Infect Chemother. 2020; 52: e31.
5.
Lacey J, Dutkiewicz J. Bioaerosols and occupational lung disease. J Aerosol Sci. 1994; 25: 1371–1404.
7.
Górny RL, editor. Microbiological Corrosion of Buildings. A Guide to Detection, Health Hazards and Mitigation. CRC Press, Taylor & Francis Group, Boca Raton-London-New York 2021.
8.
Dutkiewicz J, Mackiewicz B, Lemieszek MK. COVID 19: Possible interrelations with respiratory comorbidities caused by occupational exposure to various hazardous bioaerosols. Part I. Occurrence, epidemiology and presumed origin of the pandemic. Ann Agric Environ Med. 2020; 27: 491–504.
9.
Mackiewicz B, Dutkiewicz J, Siwiec J, Kucharczyk T, Siek E, Wójcik-Fatla A, et al. Acute hypersensitivity pneumonitis in woodworkers caused by inhalation of birch dust contaminated with Pantoea agglomerans and Microbacterium barkeri. Ann Agric Environ Med. 2019; 26: 644–655.
10.
Costabel U, Miyazaki Y, Pardo A, Koschel D, Bonella F, Spagnolo P, et al. Hypersensitivity pneumonitis. Nat Rev Dis Primers. 2020; 6: 65. doi: 10.1038/s41572-020-0191-z.
11.
Raghu G, Remy-Jardin M, Ryerson CJ, Myers JL, Kreuter M, Vasakova M, et al. Diagnosis of hypersensitivity pneumonitis in adults. An official ATS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2020; 202(3): e36-e69. doi: 10.1164/rccm.202005-2032ST.
12.
Chilamakuri R, Agarwal S. COVID-19: Characteristics and therapeutics. Cells. 2021; 10: 206. https://doi.org/10.3390/cells1....
13.
Fouladirad S, Bach H. Development of coronavirus treatments using neutralizing antibodies. Microorganisms. 2021; 9: 165. https://doi.org/10.3390/microo....
14.
Tarighi P, Eftekhari S, Chizari M, Sabernavaei M, Jafari D, Mirzabeigi P. A review of potential suggested drugs for coronavirus disease (COVID-19) treatment. Eur J Pharmacol. 2021; 895: 173890. doi: 10.1016/j.ejphar.2021.173890.
15.
Trivedi N, Verma A, Kumar D. Possible treatment and strategies for COVID-19: review and assessment. Eur Rev Med Pharmacol Sci. 2020; 24: 12593–12608.
16.
Lotfi M, Hamblin MR, Rezaei N. COVID-19: Transmission, prevention, and potential therapeutic opportunities. Clinica Chimica Acta 2020; 508: 254–266.
17.
Rajput S, Paliwal D, Naithani M, Kothari A, Meena1 K, Rana S. COVID-19 and gut microbiota: a potential connection. Ind J Clin Biochem. 2021; 1–12. doi: 10.1007/s12291-020-00948-9.
18.
Vodnar D-C, Mitrea L, Teleky B-E, Szabo K, Călinoiu L-F, Nemeş S-A, Martău G-A. Coronavirus disease (COVID-19) caused by (SARS-CoV-2) infections: a real challenge for human gut microbiota. Front Cell Infect Microbiol. 2020; 10: 575559. doi: 10.3389/fcimb.2020.575559.
19.
Alagawany M, Attia YA, Farag MR, Elnesr SS, Nagadi SA, Shafi ME, et al. The strategy of boosting the immune system under the COVID-19 pandemic. Front Vet Sci. 2021; 7: 570748. doi: 10.3389/fvets.2020.570748.
20.
Griffin G, Hewison M, Hopkin J, Kenny R, Quinton R, Rhodes J, et al. Vitamin D and COVID-19: evidence and recommendations for supplementation. R Soc Open Sci. 2020; 7: 201912. https://doi.org/10.1098/rsos.2....
21.
Correia G, Rodrigues L, Gameiro da Silva M, Gonçalves T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med Hypotheses. 2020; 141: 109781.
22.
Morawska L, Tang JW, Bahnfleth W, Bluyssend PM, Boerstrae A, Buonanno G, et al. How can airborne transmission of COVID-19 indoors be minimised? Environ Int. 2020; 142: 105832.
23.
ECDC—European Centre for Disease Prevention and Control. Infection prevention and control for COVID-19 in healthcare settings. 2020; Available at https://www.ecdc.europa/eu/sit.... Accessed 3 November 2020.
24.
Urrutia-Pereira M, Mello-da-Silva CA, Solé D. COVID-19 and air pollution: A dangerous association? Allergol Immunopathol (Madr). 2020; 48(5): 496–499.
25.
Li H, Liu Z, Ge J. Scientific research progress of COVID-19/SARS-CoV-2 in the first five months. J Cell Mol Med. 2020; 24: 6558–6570.
26.
Chan KW, Wong VT, Tang SCW. COVID-19: An update on the epidemiological, clinical, preventive and therapeutic evidence and guidelines of integrative Chinese-Western Medicine for the management of 2019 novel coronavirus disease. Am J Chin Med. 2020; 48 (3): 737–762.
27.
Adhikari SP, Meng S, Wu Y-J, Mao Y-P, Ye R-X, Wang Q-Z, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020; 9: 29. doi: 10.1186/s40249-020-00646-x.
28.
Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, evaluation and treatment of Coronavirus (COVID-19). In: StatPearls (Internet), Treasure Island (FL), StatPearls Publishing 2020. PMID: 32150360.
29.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395: 507–513.
30.
Lake MA. What we know so far: COVID-19 current clinical knowledge and research. Clin Med (Lond). 2020; 20: 124–127.
31.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; 323: 1239–1242.
32.
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Mortin CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020; 584: 430–436.
33.
Berlin DA, Gulick RM, Martinez FJ. Severe Covid-19. N Engl J Med. 2020; 383: 2451–2460.
34.
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel A, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020; 395: 1417–1418.
35.
Marin BG, Aghagoli G, Lavine K, Yang L, Siff EJ, Chiang SS, et al. Predictors of COVID-19 severity: A literature review. Rev Med Virol. 2021, 31(1): 1–10, 2146. doi: 10.1002/rmv.2146.
36.
Song YG, Shin HS. COVID-19, a clinical syndrome manifesting as hypersensitivity pneumonitis. Infect Chemother. 2020; 52: 110–112.
37.
Creamer AW, Barratt SL. Prognostic factors in chronic hypersensitivity pneumonitis. Eur Respir Rev. 2020 29: 190167. doi: 10.1183/16000617.0167-2019.
38.
Ohtsuka Y, Munakata M, Tanimura K, Ukita H, Kusaka H, Masaki Y, et al. Smoking promotes insidious and chronic farmer’s lung disease, and deteriorates the clinical outcome. Intern Med. 1995; 34: 966–971.
39.
Bellanger AP, Reboux G. Studying smoking benefit in farmer’s lung to understand Covid-19. Occup Med (Lond). 2020; 12, 70: 620–621.
40.
Propper RE. Does cigarette smoking protect against SARS-CoV-2 infection? Nicotine Tob Res. 2020; 22: 1666. doi: 10.1093/ntr/ntaa073.
41.
Erdem Ö, Derin E, Sagdic K, Yilmaz EG, Inci F. Smart materials-integrated sensor technologies for COVID-19 diagnosis. Emergent Mater. 2021; 1–17. doi: 10.1007/s42247-020-00150-w.
42.
Cleverley J, Piper J, Jones MM. The role of chest radiography in confirming covid-19 pneumonia. BMJ. 2020; 370: m2426. doi: 10.1136/bmj.m2426.
43.
Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing for Coronavirus Disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020; 296: E32-E40. doi: 10.1148/radiol.2020200642.
44.
Zhang J, Zhou L, Yang Y, Peng W, Wang W, Chen X. Therapeutic and triage strategies for 2019 novel coronavirus disease in feverclinics. Lancet Respir Med. 2020; 8(3): e11-e12. doi: 10.1016/S2213-2600(20)30071-0.
45.
Guan WJ, Ni ZY, Hu Y, Lang WH, Ou CQ, He JX, et al. China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020; 382: 1708–1720.
46.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395: 497–506.
47.
Li Y, Xia L. Coronavirus Disease 2019 (COVID-19): Role of chest CT in diagnosis and management. Am J Roentgenol. 2020; 214: 1280–1286.
48.
Huang Y, Wang S, Liu Y, Zhang Y, Zheng C, Zheng Y, et al. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19). SSRN. 2020. doi: 10.21203/rs.2.24369/v1.
49.
Campos EVR, Pereira AES, De Oliveira JL, Carvalho LB, Guilger-Casagrande M, De Lima R, Fraceto LF. How can nanotechnology help to combat COVID-19? Opportunities and urgent need. J Nanobiotechnol. 2020; 18: 125. https://doi.org/10.1186/s12951....
50.
Acquah C, Jeevanandam J, Tan KX, Danquah MK. Engineered aptamers for enhanced COVID-19 theranostics. Cell Mol Bioeng. 2021; 1–13. doi: 10.1007/s12195-020-00664-7.
51.
Silva CI, Churg A, Müller NL. Hypersensitivity pneumonitis: spectrum of high-resolution CT and pathologic findings. Am J Roentgenol. 2007; 188: 334–344.
52.
Emmanuel DA, Wenzel FJ, Lawton BR. Pulmonary mycotoxicosis. Chest. 1975; 67: 293–297.
53.
Seifert SA, Von Essen S, Jacobitz K, Crouch R, Lintner CP. Organic Dust Toxic Syndrome: a review. J Toxicol Clin Toxicol. 2003; 41: 185–193.
54.
Shazia J, Nick M, Graham C, Dela Cruz CS, Gross JE, Pasnick S. Diagnosis and management of COVID-19 disease. Am J Respir Crit Care Med. 2020; 201: P19–P22.
55.
Jean S-S, Lee P-I, Hsueh P-R. Treatment options for COVID-19: The reality and challenges. J Microbiol Immunol Infect. 2020; 54: 436–443.
56.
Agostini ML, Andres EL, Sims AC, Graham RL, Sheahan TP, Lu X, et al. Coronavirus susceptibility to the antiviral remdesivir (GS-5734) is mediated by the viral polymerase and the proofreading exoribonuclease. 2018; mBio 9: e00221–18. https://doi.org/10.1128/mBio.0....
57.
Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of COVID-19 – final report. N Engl J Med. 2020; 383: 1813–1826.
58.
Martinez MA. Compounds with therapeutic potential against novel 480 respiratory 2019 coronavirus. Antimicrob Agents Chemother. 2020; 64: e00399–20. https://doi.org/10.1128/AAC.00....
59.
Stebbing J, Phelan A, Griffin I, Tucker C, Oechsle O, Smith D, Richardson P. COVID-19: combining antiviral and anti-inflammatory treatments. Lancet Infect Dis. 2020; 20: 400–402.
60.
Shah M, Ahmad B, Choi S, Woo HG. Mutations in the SARS-CoV-2 spike RBD are responsible for stronger ACE2 binding and poor anti-SARS-CoV mAbs cross-neutralization. Comput Struct Biotechnol J. 2020: 18: 3402–3414.
61.
Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. Dexamethasone in hospitalized patients with Covid-19 — preliminary report. N Engl J Med. 2020; NEJMoa2021436. doi: 10.1056/NEJMoa2021436.
62.
Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020; 180: 934–943.
63.
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020; 395: 1033–1034.
64.
Kalil AC, Patterson TF, Mehta AK, Tomashek KM, Wolfe CR, Ghazaryan V, et al. Baricitinib plus Remdesivir for hospitalized adults with COVID-19. N Engl J Med. 2020; doi: 10.1056/NEJMoa2031994.
65.
Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020; 18: 1094–1099.
66.
Katz LM. (A little) clarity on convalescent plasma for Covid-19. N Engl J Med. 2021. https://doi.org/10.1056/NEJMe2....
67.
Seifirad S. Pirfenidone: A novel hypothetical treatment for COVID-19. Med Hypotheses. 2020; 144:110005. doi: 10.1016/j.mehy.2020.110005.
68.
Tzilas V, Tzouvelekis A, Bouros B, et al. Antifibrotic treatment in 18 patients with chronic hypersensitivity pneumonitis. Eur Respir J. 2019; 54: PA4733.
69.
Talotta R, Roberston ES. Perspectives: potential therapeutic approach with inhalation of ACE2-derived peptides for SARS-CoV-2 infection. Am J Clin Exp Immunol. 2020; 9(5): 73–80.
70.
Lemieszek MK, Rzeski W, Golec M, Mackiewicz B, Zwoliński J, Dutkiewicz J, Milanowski J. Pantoea agglomerans chronic exposure induces epithelial-mesenchymal transition in human lung epithelial cells and mice lungs. Ecotoxicol Environ Saf. 2020; 194: 110416.
71.
Ochsner SA, Pillich RT, McKenna NJ. A transcriptional regulatory atlas of coronavirus infection of human cells. BioRxiv. 2020; 2020.04.24.059527. doi: 10.1101/2020.04.24.059527.
72.
Stewart CA, Gay CM, Ramkumar K, Cargill KR, Cardnell RJ, Nilsson MB, et al. SARS-CoV-2 infection induces EMT-like molecular changes, including ZEB1-mediated repression of the viral receptor ACE2, in lung cancer models. BioRxiv. 2020; 2020.05.28.122291. doi: 10.1101/2020.05.28.122291.
73.
Santacroce L, Inchingolo F, Topi S, Del Prete R, Di Cosola M, Charitos IA, Montagnani M. Potential beneficial role of probiotics on the outcome of COVID-19 patients: An evolving perspective. Diabetes Metab Syndr. 2021; 15: 295–301. doi: 10.1016/j.dsx.2020.12.040.
74.
Donati Zeppa S, Agostini D, Piccoli G, Stocchi V, Sestili P. Gut microbiota status in COVID-19: An unrecognized player? Front Cell Infect Microbiol. 2020; 10: 576551. doi: 10.3389/fcimb.2020.576551.
75.
Di Pierro F. A possible probiotic (S. salivarius K12) approach to improve oral and lung microbiotas and raise defenses against SARS-CoV-2. Minerva Med. 2020; 111: 281–283. doi: 10.23736/s0026-4806.20.06570-2.
76.
Distler O, Highland KB, Gahlemann M, Azuma A, Fischer A, Mayes MD, et al. Nintedanib for systemic sclerosis-associated interstitial lung disease. N Engl J Med. 2019; 380: 2518–2528.
77.
Flaherty KR, Wells AU, Cottin V, Devaraj A, Walsh SLF, Inoue Y, et al. Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med. 2019; 381: 1718–1727.
78.
Ferioli M, Cisternino C, Leo V, Pisani L, Palance P, Nava S. Protecting healthcare workers from SARS-CoV-2 infection: practical indications. Eur Respir Rev. 2020; 29: 200068. https://doi.org/10.1183/160006....
79.
Spinazzè A, Cattaneo A, Cavallo DM. COVID-19 outbreak in Italy: protecting worker health and the response of the Italian Industrial Hygienists Association. Ann Work Expo Health. 2020; 64: 559–564. doi: 10.1093/annweh/wxaa044.
80.
Dugdale CM, Walensky RP. Filtration efficiency, effectiveness, and availability of N95 face masks for COVID-19 prevention. JAMA Intern Med. 2020. doi: 10.1001/jamainternmed.2020.4218. Aug 11.
81.
Calina D, Docea AO, Petrakis D, Egorov AM, Ishmukhametov AA, Gabibov AG, et al. Towards effective COVID 19 vaccines: Updates, perspectives and challenges (Review). Int J Mol Med. 2020; 46: 3–16. doi: 10.3892/ijmm.2020.4596.
82.
Kandimalla R, John A, Abburi C, Vallamkondu J, Reddy PH. Current status of multiple drug molecules, and vaccines: an update in SARS-CoV-2 therapeutics. Mol Neurobiol. 2020; 57: 4106–4116.
83.
Scarabel L, Guardascione M, Dal Bo M, Toffoli G. Pharmacological strategies to prevent SARS-CoV-2 infection and treat the early phases of COVID-19. Int J Infect Dis. 2021; 104: 441–451.
84.
Herper M. Covid-19 vaccine from Pfizer and BioNTech is strongly effective, early data from large trial indicate. STAT, November 9, 2020. https://www.statnews.com/2020/....
85.
Zimmer C. Moderna’s Covid Vaccine: What You Need to Know. The New York Times, 11 November 2020.
86.
Karlsson U, Fraenkel C-J. Complete protection from covid-19 is possible for health workers. All they need is the right protective equipment. BMJ. 2020; 370: m2641. http://dx.doi.org/10.1136/bmj.....
87.
Godderis L, Boone A, Bakusic J. COVID-19: a new work-related disease threatening healthcare workers. Occup Med. 2020; 70: 315–316.
88.
Barranco R, Ventura F. Covid-19 and infection in health-care workers: An emerging problem. Medico-Legal J. 2020; 88: 65–66.
89.
Mackiewicz B, Skórska C, Dutkiewicz J. Relationship between concentrations of microbiological agents in the air of agricultural settings and occurrence of work-related symptoms in exposed persons. Ann Agric Environ Med. 2015; 22: 473–477.
90.
Dutkiewicz J, Skórska C, Mackiewicz B, Cholewa G. Prevention of the Diseases Caused by Organic dusts in the Agriculture and Agricultural Industry. Institute of Rural Health, Lublin 2000 (in Polish).
91.
Karan A, Ali K, Teelucksingh S, Sakhamuri S. The impact of air pollution on the incidence and mortality of COVID-19. Glob Health Res Policy. 2020; 5: 39. https://doi.org/10.1186/s41256....
92.
Comunian S, Dongo D, Milani C, Palestini P. Air pollution and COVID-19: The role of particulate matter in the spread and increase of COVID-19’s morbidity and mortality. Int J Environ Res Public Health. 2020; 17: 4487. doi: 10.3390/ijerph17124487.
93.
Pansini R, Fornacca D. Initial evidence of higher morbidity and mortality due to SARS-CoV-2 in regions with lower air quality. MedRxiv. 2020; https://www.medrxiv.org/conten....
94.
Félix-Arellano EE, Schilmann A, Hurtado-Díaz M, Texcalac-Sangrado JL, Riojas-Rodríguez H. Quick review: air pollution and morbi-mortality by Covid-19. Salud Publica Mex. 2020; 62: 582–589 (in Spanish).
95.
Mukherjee S, Boral S, Siddiqi H, Mishra A, Meikap BC. Present cum future of SARS-CoV-2 virus and its associated control of virus-laden air pollutants leading to potential environmental threat – a review. J Environ Chem Eng. 2021; 9: 104973. doi: 10.1016/j.jece.2020.104973.
96.
Al Huraimel K, Alhosani M, Kunhabdulla S, Stietiya MH. SARS-CoV-2 in the environment: Modes of transmission, early detection and potential role of pollutions. Sci Total Environ. 2020; 744: 140946.
97.
Wu D, Lu J, Liu Y, Hang Z, Luo L. Positive effects of COVID-19 control measures on influenza prevention. Int J Infect Dis. 2020; 95: 345–346.
98.
Samson RA, Flannigan B, Flannigan ME, et al. Health Implications of Fungi in Indoor Environments. Elsevier, Amsterdam 1994.
99.
Anderson K, Watt AD, Sinclair D, Lewis C, McSharry CP, Boyd G. Climate, intermittent humidification, and humidifier fever. Br J Ind Med.1989; 46: 671–674.
100.
Ando A, Hagiya H, Nada T, Kiura K, Waseda K, Kammei Rai K, et al. Hypersensitivity pneumonitis caused by a home ultrasonic humidifier contaminated with Candida guilliermondii. Intern Med. 2017; 56: 3109–3112.
101.
Ohnishi H, Yokoyama A, Hamada H, Manabe S, Ito R, Watanabe A, et al. Humidifier lung: Possible contribution of endotoxin-induced lung injury. Intern Med. 2002; 41: 1179–1182.
102.
Müller-Wening D, Koschel D, Stark W, Sennekamp H-J. Humidifier-associated disease in the general population. Dtsch Med Wochenschr. 2006; 131: 491–496 (in German).
103.
Morawska L, Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ Int. 2020; 139: 105730.
104.
Kumar P, Morawska L. Could fighting airborne transmission be the next line of defence against COVID-19 spread? City Environ Interact. 2019; 4: 100033.
105.
Sattar SA, Wright KE, Zargar B, Rubino JR, Iljaz MK. Airborne infectious agents and other pollutants in automobiles for domestic use: potential health impacts and approaches to risk mitigation. J Environ Public Health. 2016; 2016: 1548326. doi: 10.1155/2016/1548326.
106.
Amoatey P, Omidvarborna H, Baawain MS, Al-Mamun A. Impact of building ventilation systems and habitual indoor incense burning on SARS-CoV-2 virus transmissions in Middle Eastern countries. Sci Total Environ. 2020; 733: 139356.
107.
WHO Report on the Global Tobacco Epidemic, 2008: The MPOWER Package. World Health Organization, Geneva 2008.
108.
Larsson L, Szponar B, Ridha B, Pehrson C, Dutkiewicz J, Krysińska-Traczyk E, Sitkowska J. Identification of bacterial and fungal components in tobacco and tobacco smoke. Tob Induc Dis. 2008; Epub 4:4. doi: 10.1 186/1617-9625-4-4. http:\\www.tobaccoinduceddiseases.com/content/4/1/4.
109.
Larsson L, Szponar B, Pehrson C. Tobacco smoking increases dramatically air concentrations of endotoxin. Indoor Air. 2004; 14: 421–424.
110.
Mulrooney Eldred S. Coronavirus FAQ: Is it a good idea to buy an air cleaner for my home? NPR., September 4, 2020. https://www.npr.org/sections/g... (accessed November 14, 2020).
111.
Markowicz P, Larsson L. The surface emissions trap: a new approach in indoor air purification. J Microbiol Methods. 2012; 91: 290–294.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.