Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Susac’s syndrome – the crucial role of imaging tests for proper diagnosis
1
Department of Ophthalmology, Voivodeship Regional Hospital, Kielce, Poland
2
Jan Kochanowski University, Kielce, Poland
3
Department of Vitreoretinal Surgery, Medical University, Lublin, Poland
4
Department of Imaging Diagnostics, Voivodeship Regional Hospital, Kielce, Poland
5
Ophthalmology Clinic Boni Fratres Lodziensis, Poland
Corresponding author
Joanna Roskal-Wałek
Department of Ophthalmology, Voivodeship Regional Hospital, Grunwaldzka 45, 25-736, Kielce, Poland
Department of Ophthalmology, Voivodeship Regional Hospital, Grunwaldzka 45, 25-736, Kielce, Poland
Ann Agric Environ Med. 2022;29(2):190-200
KEYWORDS
magnetic resonance imagingoptical coherence tomographyfluorescein angiographymultiple sclerosisSusac‘s syndrome
TOPICS
ABSTRACT
Introduction:
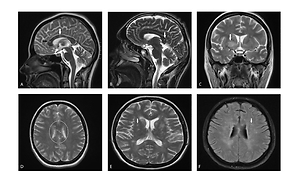
Susac’s syndrome (SS) is a rare, autoimmune-mediated endoteliopathy characterized by a clinical triad of encephalopathy, branch retinal artery occlusion, and sensorineural hearing loss. SS is also characterized by a neuroimaging triad consisting of white matter lesions, grey matter lesions, and leptomeningeal enhancement on magnetic resonance imaging (MRI). Considering the rarity of SS, as well as certain similarity to other, more frequent neurological diseases, such as multiple sclerosis (MS), this syndrome is sometimes incorrectly diagnosed and treated.
Objective:
The aim of the study is to present the current state of knowledge on SS, with particular consideration for the differential diagnostics between SS and MS, using the latest available imaging techniques, such as brain MRI, optical coherence tomography (OCT), OCT angiography (OCTA) and fluorescein angiography (FA).
Review methods:
The major electronic databases (PubMed, Google Scholar) were searched manually in order to identify the relevant studies published on SS.
Brief description of the state of knowledge:
Distinguishing SS from MS is a diagnostic challenge. In the majority of cases, patients with SS do not present the complete clinical or neuroimaging triad, and a delay in making the correct diagnosis exposes the patient to the occurrence of complications, resulting from the development of the underlying disease, or/and the application of improper treatment. In the case of SS the results of brain MRI and FA are essential for making the correct diagnosis as they may reveal pathognomonic changes.
Summary:
Imaging examinations, such as brain MRI, FA, and OCT complement each other, due to which the diagnosis of SS may be simpler, irrespective of the stage of the disease.
Susac’s syndrome (SS) is a rare, autoimmune-mediated endoteliopathy characterized by a clinical triad of encephalopathy, branch retinal artery occlusion, and sensorineural hearing loss. SS is also characterized by a neuroimaging triad consisting of white matter lesions, grey matter lesions, and leptomeningeal enhancement on magnetic resonance imaging (MRI). Considering the rarity of SS, as well as certain similarity to other, more frequent neurological diseases, such as multiple sclerosis (MS), this syndrome is sometimes incorrectly diagnosed and treated.
Objective:
The aim of the study is to present the current state of knowledge on SS, with particular consideration for the differential diagnostics between SS and MS, using the latest available imaging techniques, such as brain MRI, optical coherence tomography (OCT), OCT angiography (OCTA) and fluorescein angiography (FA).
Review methods:
The major electronic databases (PubMed, Google Scholar) were searched manually in order to identify the relevant studies published on SS.
Brief description of the state of knowledge:
Distinguishing SS from MS is a diagnostic challenge. In the majority of cases, patients with SS do not present the complete clinical or neuroimaging triad, and a delay in making the correct diagnosis exposes the patient to the occurrence of complications, resulting from the development of the underlying disease, or/and the application of improper treatment. In the case of SS the results of brain MRI and FA are essential for making the correct diagnosis as they may reveal pathognomonic changes.
Summary:
Imaging examinations, such as brain MRI, FA, and OCT complement each other, due to which the diagnosis of SS may be simpler, irrespective of the stage of the disease.
ACKNOWLEDGEMENTS
Project financed under the program the Minister of Education
and Science called “Regional Initiative of Excellence” in the
years 2019–2022, project no. 024/RID/2018/19, amount of
financing 11 999 000,00 PLN.
REFERENCES (75)
1.
Dörr J, Krautwald S, Wildemann B, et al. Characteristics of Susac syndrome: a review of all reported cases. Nat Rev Neurol. 2013;9(6):307–316. doi: 10.1038/nrneurol.2013.82.
2.
Egan RA. Diagnostic Criteria and Treatment Algorithm for Susac Syndrome. J Neuroophthalmol. 2019;39(1):60–67. doi: 10.1097/WNO.0000000000000677.
3.
Nazari F, Azimi A, Abdi S. What is Susac syndrome? – A brief review of articles. Iran J Neurol. 2014; 13(4): 209–214.
4.
Kleffner I, Duning T, Lohmann H, et al. A brief review of Susac syndrome. J Neurol Sci. 2012;322(1–2):35–40. doi: 10.1016/j.jns.2012.05.021.
5.
García-Carrasco M, Mendoza-Pinto C, Cervera R. Diagnosis and classification of Susac syndrome. Autoimmun Rev. 2014;13(4–5):347–350. doi: 10.1016/j.autrev.2014.01.038.
6.
Vishnevskia-dai V, Chapman J, Sheinfeld R, et al. Susac syndrome: clinical characteristics, clinical classification, and long-term prognosis. Medicine (Baltimore). 2016; 95(43): e5223 doi: 10.1097/MD.0000000000005223.
7.
Włoch-Targońska M, Dubiel-Braszczok B, Kotyla P. Susac syndrome – diagnostic difficulties. Alergia Astma Immunologia 2018, 23 (1): 24–28.
8.
Vattoth S, Compton CJ, Roberson GH, et al. Susac syndrome. A differential diagnosis for demyelination. Neurosciences (Riyadh). 2013;18(1):74–78.
9.
Rennebohm RM, Egan RA, Susac JO. Treatment of Susac’s Syndrome. Curr Treat Options Neurol. 2008;10(1):67–74. doi: 10.1007/s11940-008-0008-y.
10.
Seifert-Held T, Langner-Wegscheider BJ, Komposch M, et al. Susac’s syndrome: clinical course and epidemiology in a Central European population. Int J Neurosci. 2017;127(9):776–780. doi: 10.1080/00207454.2016.1254631.
11.
Wilf-Yarkoni A, Elkayam O, Aizenstein O, et al. Increased incidence of Susac syndrome: a case series study. BMC Neurol. 2020;20(1):332. doi: 10.1186/s12883-020-01892-0.
12.
Buzzard KA, Reddel SW, Yiannikas C, et al. Distinguishing Susac’s syndrome from multiple sclerosis. J Neurol. 2015;262(7):1613–1621. doi: 10.1007/s00415-014-7628-9.
13.
Fonderska P, Tomalka-Kochanowska J, Kochanowski J, et al. Susac‘s syndrome diagnostic difficulties – the neurological point of view. Neurol Neurochir Pol. 2022. doi: 10.5603/PJNNS.a2021.0082.
14.
Stefanou MI, Doycheva D, Ebrahimi A, et al. Susac-Syndrom: ein diagnostisches Chamäleon. Laryngorhinootologie. 2019;98(4):268–275. doi: 10.1055/a-0747-6916.
15.
Heng LZ, Bailey C, Lee R, et al. A review and update on the ophthalmic implications of Susac syndrome. Surv Ophthalmol. 2019;64(4):477–485. doi: 10.1016/j.survophthal.2019.01.007.
16.
Shields RA, Kleinman RA, Smith SJ, et al. A fatal case of Susac syndrome: The importance of ophthalmic examination in confirming the diagnosis. Am J Ophthalmol Case Rep. 2018;12:18–20. doi: 10.1016/j.ajoc.2018.07.004.
17.
Algahtani H, Shirah B, Amin M, et al. Susac syndrome misdiagnosed as multiple sclerosis with exacerbation by interferon beta therapy. Neuroradiol J. 2018;31(2):207–212. doi: 10.1177/1971400917712265.
18.
Laird PW, Newman NJ, Yeh S. Exacerbation of Susac syndrome retinopathy by interferon Beta-1a. Arch Ophthalmol. 2012;130(6):804–806. doi: 10.1001/archophthalmol.2011.1841.
19.
Zhovtis Ryerson L, Kister I, Snuderl M, et al. Incomplete Susac syndrome exacerbated after natalizumab. Neurol Neuroimmunol Neuroinflamm. 2015;24;2(5):e151. doi: 10.1212/NXI.0000000000000151.
20.
Roskal-Wałek J, Biskup M, Dolecka-Ślusarczyk M, et al. Manifestation of Susac syndrome during interferon beta-1a and glatiramer acetate treatment for misdiagnosed multiple sclerosis: a case report. BMC Ophthalmol. 2021;21(1):352. doi: 10.1186/s12886-021-02101-3.
21.
Sveinsson O, Kolloch J, Träisk F, et al. Susacs syndrom är ett ovanligt inflammatoriskt tillstand – Kan misstas för multipel skleros – tidig diagnos är en utmaning. Lakartidningen. 2020;117:FSSS.
22.
Turczyńska MJ, Krajewski P, Brydak-Godowska JE. Widefield fluorescein angiography in the diagnosis of susac syndrome. Retina. 2021;41(7):1553–1561. doi: 10.1097/IAE.0000000000003051.
23.
Coulette S, Lecler A, Saragoussi E, et al. Diagnosis and Prediction of Relapses in Susac Syndrome: A New Use for MR Postcontrast FLAIR Leptomeningeal Enhancement. AJNR Am J Neuroradiol. 2019;40(7):1184–1190. doi: 10.3174/ajnr.A6103.
24.
Bellanger G, Biotti D, Adam G, et al. Leptomeningeal enhancement on post-contrast FLAIR images for early diagnosis of Susac syndrome. Multiple Sclerosis J. 2021. doi:10.1177/13524585211012349.
25.
Susac JO, Murtagh FR, Egan RA, et al. MRI findings in Susac’s syndrome. Neurology. 2003;61(12):1783–1787. doi: 10.1212/01.wnl.0000103880.29693.48.
26.
Bernard JT, Romero R, Agrawal K, et al. Optical coherence tomography in Susac’s syndrome. Mult Scler Relat Disord. 2014;3(1):110–116. doi: 10.1016/j.msard.2013.05.005.
27.
Brandt AU, Zimmermann H, Kaufhold F, et al. Patterns of retinal damage facilitate differential diagnosis between Susac syndrome and MS. PLoS One. 2012;7(6):e38741. doi: 10.1371/journal.pone.0038741.
28.
Ringelstein M, Albrecht P, Kleffner I, et al. Retinal pathology in Susac syndrome detected by spectral-domain optical coherence tomography. Neurology. 2015;85(7):610–8. doi: 10.1212/WNL.0000000000001852.
29.
Farci R, Carta A, Cocco E, et al. Optical coherence tomography angiography in multiple sclerosis: A cross-sectional study. PLoS One. 2020;15(7):e0236090. doi: 10.1371/journal.pone.0236090.
30.
Spiess K, Martínez JRG. OCT Angiography: Assessment of Retinal Ischemia in Susac’s Syndrome. Ophthalmic Surg Lasers Imaging Retina. 2017;48(6):505–508. doi: 10.3928/23258160-20170601-10.
31.
Azevedo AGB, Lima LH, Müller L, et al. Anatomical and functional correlation in Susac syndrome: multimodal imaging assessment. Int J Retina Vitreous. 2017;3:39. doi: 10.1186/s40942-017-0092-9.
32.
Todorich B, Williams GA, Faia LJ. Optical Coherence Tomography Angiography Findings in Susac Syndrome. Ophthalmol Retina. 2017;1(2):164. doi: 10.1016/j.oret.2016.08.010.
33.
García-Serrano JL, Munoz de Escalona-Rojas JE, Callejas-Rubio JL, et al. Angiografía por tomografía de coherencia óptica en el diagnóstico precoz del síndrome de Susac. Neurología. 2020;35:62–63.
34.
Egan RA, Hills WL, Susac JO. Gass plaques and fluorescein leakage in Susac Syndrome. J Neurol Sci. 2010;299(1–2):97–100. doi: 10.1016/j.jns.2010.08.043.
35.
Mallam B, Damato EM, Scolding NJ, et al. Serial retinal fluorescein angiography and immune therapy in Susac’s syndrome. J Neurol Sci. 2009;285:230–234.
36.
Hamann T, Wiest M, Innes W, et al. A Novel Quantitative Assessment Method of Disease Activity in Susac’s Syndrome Based on Ultra-Wide Field Imaging. Curr Eye Res. 2021:1–7. doi: 10.1080/02713683.2021.1967402.
37.
Engisch R, Titelbaum DS, Chilver-Stainer L, et al. Susac’s syndrome: Leptomeningeal enhancement on 3D FLAIR MRI. Mult Scler. 2016;22(7):972–4. doi: 10.1177/1352458516636836.
38.
Agamanolis DP, Prayson RA, Asdaghi N, et al. Brain microvascular pathology in Susac syndrome: an electron microscopic study of five cases. Ultrastruct Pathol. 2019;43(6):229–236. doi: 10.1080/01913123.2019.1692117.
39.
Johnson P, Chan JK, Vavasour IM, et al. Quantitative MRI findings indicate diffuse white matter damage in Susac Syndrome. Mult Scler J Exp Transl Clin. 2022;8(1):20552173221078834. doi: 10.1177/20552173221078834.
40.
Rennebohm RM, Lubow M, Rusin J, et al. Aggressive immunosuppressive treatment of Susac’s syndrome in an adolescent: using treatment of dermatomyositis as a model. Pediatr Rheumatol Online J. 2008;6:3. doi: 10.1186/1546-0096-6-3.
41.
Jarius S, Kleffner I, Dorr JM, et al. Clinical, paraclinical and serological findings in Susac syndrome: an international multicenter study. J Neuroinflammation. 2014;11:46–56.
42.
Gross CC, Meyer C, Bhatia U, et al. CD8+ T cell-mediated endotheliopathy is a targetable mechanism of neuro-inflammation in Susac syndrome. Nat Commun. 2019;10(1):5779. doi: 10.1038/s41467-019-13593-5.
43.
Venditti L, Rousseau A, Ancelet C, et al. Susac syndrome following COVID-19 infection. Acta Neurol Belg. 2021;121(3):807–809. doi: 10.1007/s13760-020-01554-5.
44.
Al-Hasan Y, Hoskin JL, Wolf JC, et al. Susac Syndrome and Pregnancy. Case Rep Neurol Med. 2020;2020:6049126. doi: 10.1155/2020/6049126.
45.
Qiu J, Riminton DS, Reddel SW, et al. Pregnancy without relapse following treated Susac syndrome. Mult Scler Relat Disord. 2020;45:102357. doi: 10.1016/j.msard.2020.102357.
46.
Bucciarelli S, Cervera R, Martínez M, et al. Susac’s syndrome or catastrophic antiphospholipid syndrome? Lupus. 2004;13(8):607–608. doi: 10.1191/0961203304lu1046cr.
47.
Fernando SL, Boyle T, Smith A, et al. The Successful Use of Infliximab in a Relapsing Case of Susac’s Syndrome. Case Rep Neurol Med. 2020;2020:9317232. doi: 10.1155/2020/9317232.
48.
David C, Papo T, Ba I, et al. Hunting for the genetic basis of Susac syndrome. European Journal of Neurology. 2021;28(7):e57-e59. doi: 10.1111/ene.14836.
49.
Obelieniene D, Macaityte R, Balnyte R, et al. Characteristics of headache in relation to the manifestation of Susac syndrome. Medicina (Kaunas). 2017;53(6):420–425. doi: 10.1016/j.medici.2018.01.003.
50.
Patel VA, Dunklebarger M, Zacharia TT, et al. Otologic manifestations of Susac syndrome. Acta Otorhinolaryngol Ital. 2018;38(6):544–553. doi: 10.14639/0392-100X-2166.
51.
Dörr JS, Jarius B, Wildemann EB. et al. Eine interdisziplinäre Herausforderung Susac syndrome An interdisciplinary challenge. Nervenarzt 2011; 82(10):1250–1263 doi 10.1007/s00115-011-3280-0.
52.
TNF neutralization in MS: results of a randomized, placebo-controlled multicenter study. The Lenercept Multiple Sclerosis Study Group and The University of British Columbia MS/MRI Analysis Group. Neurology. 1999;53(3):457–65.
53.
Susac JO, Egan RA, Rennebohm RM, et al. Susac’s syndrome: 1975–2005 microangiopathy/autoimmune endotheliopathy. J Neurol Sci. 2007;257(1–2):270–272. doi: 10.1016/j.jns.2007.01.036.
54.
Filippi M, Preziosa P, Banwell BL, et al. Assessment of lesions on magnetic resonance imaging in multiple sclerosis: practical guidelines. Brain. 2019;142(7):1858–1875. doi: 10.1093/brain/awz144.
55.
Solomon AJ, Naismith RT, Cross AH. Misdiagnosis of multiple sclerosis: Impact of the 2017 McDonald criteria on clinical practice. Neurology. 2019;92(1):26–33. doi:10.1212/WNL.0000000000006583.
56.
Bruschi N, Boffa G, Inglese M. Ultra-high-field 7-T MRI in multiple sclerosis and other demyelinating diseases: from pathology to clinical practice. Eur Radiol Exp. 2020;4(1):59. doi:10.1186/s41747-020-00186-x.
57.
Chen L, Gordon LK. Ocular manifestations of multiple sclerosis. Curr Opin Ophthalmol. 2005;16(5):315–320. doi: 10.1097/01.icu.0000179804.49842.e2.
58.
Sapko K, Jamroz-Wiśniewska A, Woźniak A, et al. Susac syndrome as a multidisciplinary diagnostic challenge. Ann Agric Environ Med. 2021. doi:10.26444/aaem/136524.
59.
Zur D, Goldstein M, Barequet D, et al. Susac’s syndrome—A new ocular finding and disease outcome. Eye (Lond). 2021. doi: 10.1038/s41433-021-01464-7.
60.
Sauma J, Rivera D, Wu A, et al. Susac‘s syndrome: an update. Br J Ophthalmol. 2020;104(9):1190–1195. doi: 10.1136/bjophthalmol-2019-315597.
61.
Miller DH, Weinshenker BG, Filippi M, et al. Differential diagnosis of suspected multiple sclerosis: a consensus approach. Mult Scler. 2008;14(9):1157–74. doi: 10.1177/1352458508096878.
62.
AlBloushi AF, Dheyab AM, Al-Swaina NF, et al. Clinical findings and outcomes of uveitis associated with multiple sclerosis. Eur J Ophthalmol. 2021;31(2):482–490. doi: 10.1177/1120672120904667.
63.
Van Oevelen K, Dirven W, Tassignon MJ. et al. Retinal fluorescein angiography in Susac Syndrome: a shifting pattern of arteriolar wall hyperfluorescence–Report of two cases. Retinal Cases and Brief Reports, 2022.
64.
Britze J, Frederiksen JL. Optical coherence tomography in multiple sclerosis. Eye (Lond). 2018;32(5):884–888. doi:10.1038/s41433-017-0010-2.
65.
Zimmermann H, Oberwahrenbrock T, Brandt AU, et al. Optical coherence tomography for retinal imaging in multiple sclerosis. Degener Neurol Neuromuscul Dis. 2014;4:153–162. doi: 10.2147/DNND.S73506.
66.
Martinet N, Fardeau C, Adam R, et al. Fluorescein and indocyanine green angiographies in Susac syndrome. Retina. 2007;27(9):1238–1242. doi: 10.1097/IAE.0b013e31809ff824.
67.
Alba-Linero C, Liscombe-Sepúlveda JP, Llorenç V, et al. Use of ultra-wide field retinal imaging and optical coherence tomography angiography in the diagnosis of incomplete Susac syndrome. Eur J Ophthalmol. 2021;31(6):3238–3247. doi: 10.1177/1120672120965482.
68.
Wirth MA, Khan HM, Chan J, et al. Investigating Microangiopathy using Swept-Source Optical Coherence Tomography Angiography in Patients with Susac Syndrome. Retina. 2021. doi: 10.1097/IAE.0000000000003170.
69.
Mastropasqua R, Toto L, Senatore A, et al. Optical coherence tomography angiography findings in Susac’s syndrome: a case report. International Ophthalmology. 2018;38(4):1803–1808. doi: 10.1007/s10792-017-0653-9.
70.
Cordon B, Vilades E, Orduna E, et al. Angiography with optical coherence tomography as a biomarker in multiple sclerosis. PLoS One. 2020;15(12):e0243236. doi: 10.1371/journal.pone.0243236.
71.
Lanzillo R, Cennamo G, Criscuolo C, et al. Optical coherence tomography angiography retinal vascular network assessment in multiple sclerosis. Mult Scler. 2018;24(13):1706–1714. doi: 10.1177/1352458517729463.
72.
Feucht N, Maier M, Lepennetier G, et al. Optical coherence tomography angiography indicates associations of the retinal vascular network and disease activity in multiple sclerosis. Mult Scler. 2019;25(2):224–234. doi: 10.1177/1352458517750009.
73.
Turc G, Monnet D, Dupin N, et al. Skin involvement in Susac’s syndrome. J Neurol Sci. 2011;305(1–2):152–155. doi: 10.1016/j.jns.2011.03.001.
74.
Kleffner I, Dörr J, Ringelstein M, et al. European Susac Consortium (EuSaC). Diagnostic criteria for Susac syndrome. J Neurol Neurosurg Psychiatry. 2016;87(12):1287–1295. doi: 10.1136/jnnp-2016-314295.
75.
Rennebohm RM, Asdaghi N, Srivastava S, et al. Guidelines for treatment of Susac syndrome – An update. Int J Stroke. 2020;15(5):484–494. doi: 10.1177/1747493017751737.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.