Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Comparison of anthropometric indicators related to overweight and obesity by place of residence in a local community with a high social deprivation rate – a cross-sectional study
1
Department of Family and Geriatric Nursing, Faculty of Health Sciences, Medical University, Lublin, Poland
2
Department of Epidemiology and Population Studies, Jagiellonian University Medical College, Kraków, Poland
Corresponding author
Grzegorz Józef Nowicki
Department of Family and Geriatric Nursing, Faculty of Health Sciences, Medical University of Lublin, Poland, Staszica 4/6, 20-081, Lublin, Poland
Department of Family and Geriatric Nursing, Faculty of Health Sciences, Medical University of Lublin, Poland, Staszica 4/6, 20-081, Lublin, Poland
Ann Agric Environ Med. 2024;31(2):248-254
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Obesity is considered a major public health concern. The aim of the study is to compare anthropometric indicators related to overweight and obesity by place of residence in a local community with a high social deprivation rate, based on the example of residents of the Janów District in eastern Poland, taking into account gender strata differences.
Material and methods:
The cross-sectional epidemiological study was carried out in a study group of 3,752 individuals. The following anthropometric measurements and laboratory tests were performed to identify the anthropometric indicators related to overweight and obesity: body mass index (BMI), waist-to-hip ratio (WHR) and waist-to-height ratio (WHtR) and body adiposity index (BAI).
Results:
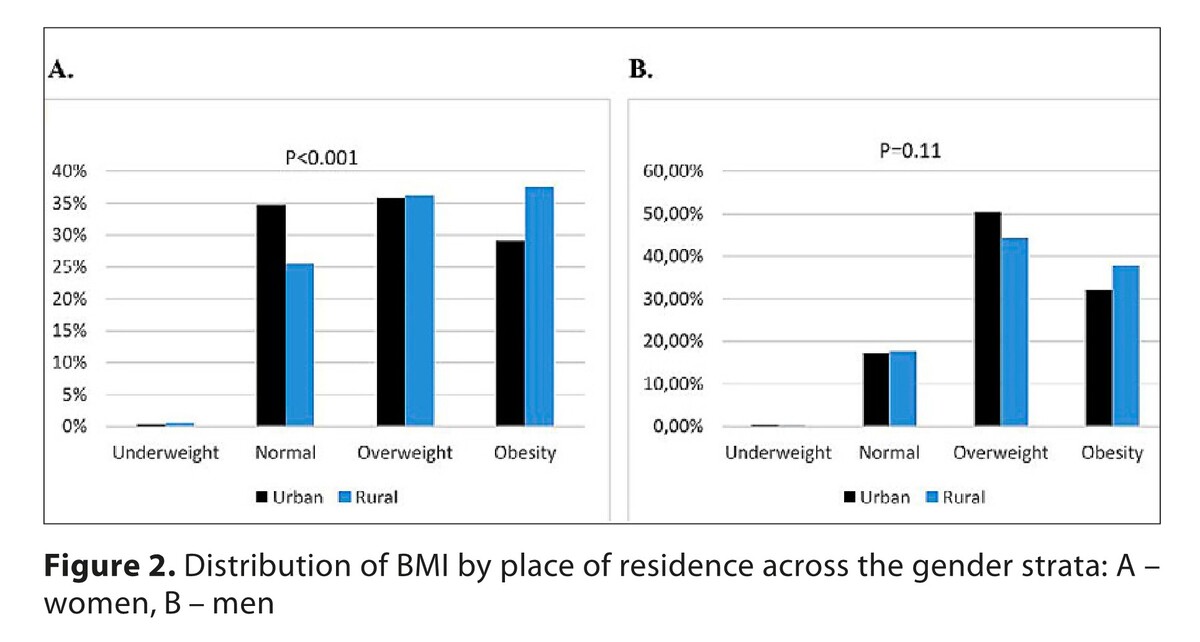
Mean age of the study group was 51.92 ± 8.15. Overweight and obesity-related indicators were more prevalent in rural than urban areas among women, and were as follows: BMI (28.77 ± 5.37 vs. 27.62 ± 5.09; p < 0.001), WHR (0.87 ± 0.07 vs. 0.85 ± 0.07; p < 0.001), WHtR (0.57 ± 0.09 vs. 0.57 ± 0.08; p < 0.001) and BAI (33.58 ± 5.48 vs. 32.82 ± 5.4; p = 0.002). Men’s mean WHR was higher in rural than in urban areas (0.96 ± 0.07 vs. 0.95 ± 0.62; p < 0.001).
Conclusions:
The study shows that women living in rural areas had a mean BMI that was 1.1 higher than that of women living in urban areas, as well as 0.02 higher WHR and WHtR and 0.8 higher BAI. In contrast, men living in rural areas had a 0.001 higher WHtR and WHR than men living in urban areas. In the multivariable models, after having considered potential confounding variables, women living in rural areas had approximately a 60% higher probability of being obese, while men had approximately a 30% higher probability of being obese.
Obesity is considered a major public health concern. The aim of the study is to compare anthropometric indicators related to overweight and obesity by place of residence in a local community with a high social deprivation rate, based on the example of residents of the Janów District in eastern Poland, taking into account gender strata differences.
Material and methods:
The cross-sectional epidemiological study was carried out in a study group of 3,752 individuals. The following anthropometric measurements and laboratory tests were performed to identify the anthropometric indicators related to overweight and obesity: body mass index (BMI), waist-to-hip ratio (WHR) and waist-to-height ratio (WHtR) and body adiposity index (BAI).
Results:
Mean age of the study group was 51.92 ± 8.15. Overweight and obesity-related indicators were more prevalent in rural than urban areas among women, and were as follows: BMI (28.77 ± 5.37 vs. 27.62 ± 5.09; p < 0.001), WHR (0.87 ± 0.07 vs. 0.85 ± 0.07; p < 0.001), WHtR (0.57 ± 0.09 vs. 0.57 ± 0.08; p < 0.001) and BAI (33.58 ± 5.48 vs. 32.82 ± 5.4; p = 0.002). Men’s mean WHR was higher in rural than in urban areas (0.96 ± 0.07 vs. 0.95 ± 0.62; p < 0.001).
Conclusions:
The study shows that women living in rural areas had a mean BMI that was 1.1 higher than that of women living in urban areas, as well as 0.02 higher WHR and WHtR and 0.8 higher BAI. In contrast, men living in rural areas had a 0.001 higher WHtR and WHR than men living in urban areas. In the multivariable models, after having considered potential confounding variables, women living in rural areas had approximately a 60% higher probability of being obese, while men had approximately a 30% higher probability of being obese.
REFERENCES (54)
1.
Lin X, Li H. Obesity: epidemiology, pathophysiology, and therapeutics. Front Endocrinol. 2021;12:706978. doi:10.3389/fendo.2021.706978.
2.
World Health Organization: Obesity and overweight. https://www.who.int/news-room/... (access: 2023.11.05).
3.
Global Burden of Disease Cancer Collaboration, Fitzmaurice C, Abate D, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the global burden of disease study. JAMA Oncol. 2019;5(12):1749–1768. doi:10.1001/jamaoncol.2019.2996.
4.
Gallus S, Lugo A, Murisic B, Bosetti C, Boffetta P, La Vecchia C. Overweight and obesity in 16 European countries. Eur J Nutr. 2015;54(5):679–689. doi:10.1007/s00394-014-0746-4.
5.
OECD/European Union (2016). Health at a glance: Europe 2016: State of health in the EU cycle, OECD Publishing, Paris, https://doi.org/10.1787/978926....
6.
Stoś K, Rychlik E, Woźniak A, et al. Prevalence and sociodemographic factors associated with overweight and obesity among adults in Poland: a 2019/2020 nationwide cross-sectional survey. Int J Environ Res Public Health. 2022;19(3):1502. doi:10.3390/ijerph19031502.
7.
Rozporządzenie Rady Ministrów z dnia 30 marca 2021 r. w sprawie Narodowego Programu Zdrowia na lata 2021–2025 (DzU 2021 poz. 642).
8.
Wilson CR, Rourke J, Oandasan IF, Bosco C. Progress made on access to rural healthcare in Canada. Can J Rural Med. 2020;25:14–9.
9.
Okobi OE, Ajayi OO, Okobi TJ, et al. The burden of obesity in the rural adult population of America. Cureus. 2021;13(6):e15770. doi:10.7759/cureus.15770.
10.
Kondro W. Health of rural Canadians lags behind urban counterparts. CMAJ. 2006;175(10):1195. doi:10.1503/cmaj.061306.
11.
Winkelmann J, Muench U, Maier CB. Time trends in the regional distribution of physicians, nurses and midwives in Europe. BMC Health Serv Res. 2020;20(1):937. doi:10.1186/s12913-020-05760-y.
12.
Połtyn-Zaradna K, Psikus P, Zatońska K. Changes in attitudes toward tobacco smoking and factors associated with quitting in 9-year observation of PURE Poland cohort study. Int J Environ Res Public Health. 2022;19(11):6564. doi:10.3390/ijerph19116564.
13.
Moreno-Llamas A, García-Mayor J, De la Cruz-Sánchez E. Urban-rural differences in trajectories of physical activity in Europe from 2002 to 2017. Health Place. 2021;69:102570. doi:10.1016/j.healthplace.2021.102570.
14.
NCD Risk Factor Collaboration (NCD-RisC). Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature. 2019;569(7755):260–264. doi:10.1038/s41586-019-1171-x.
15.
Lipoeto NI, Geok Lin K, Angeles-Agdeppa I. Food consumption patterns and nutrition transition in South-East Asia. Public Health Nutr. 2013;16(9):1637–1643. doi:10.1017/S1368980012004569.
16.
Jones-Smith JC, Popkin BM. Understanding community context and adult health changes in China: development of an urbanicity scale. Soc Sci Med. 2010;71(8):1436–1446. doi:10.1016/j.socscimed.2010.07.027.
17.
Nandi A, Sweet E, Kawachi I, Heymann J, Galea S. Associations between macrolevel economic factors and weight distributions in low- and middle-income countries: a multilevel analysis of 200,000 adults in 40 countries. Am J Public Health. 2014;104(2):e162-e171. doi:10.2105/AJPH.2013.301392.
18.
Neuman M, Kawachi I, Gortmaker S, Subramanian S. National economic development and disparities in body mass index: a cross-sectional study of data from 38 countries. PLoS One. 2014;9(6):e99327. doi:10.1371/journal.pone.0099327.
19.
Giannaros D. Twenty years after the economic restructuring of Eastern Europe: an economic review. Int Bus Econ Res J. 2008; 7: 35–38. https://doi.org/10.19030/iber.....
20.
Leinsalu M, Stirbu I, Vagerö D, et al. Educational inequalities in mortality in four Eastern European countries: divergence in trends during the post-communist transition from 1990 to 2000. Int J Epidemiol. 2009;38(2):512–525. doi:10.1093/ije/dyn248.
21.
European Commission. Food Safety, Food Law General Principles. Available online: https://ec.europa.eu/food/hori... (accessed on 25 October 2021).
22.
Statistics Poland. Statistical yearbook of Republic of Poland. Warsaw: Statistics Poland; 2021.
23.
World Obesity. Global Obesity Observatory. Poland, Obesity Prevalence. https://data.worldobesity.org/... (access: 2023.11.02).
24.
Smętkowski M, Gorzelak G, Płoszaj A, Rok J. Poviats threatened by deprivation: state, trends and prospects. EUROREG Rep Anal. 2015; 7. doi:10.13140/RG.2.2.22835.84004.
25.
Central Statistical Office (GUS). Report on results. National census of population and apartments 2011. https://stat.gov.pl/cps/rde/xb... (access: 2023.10.05).
26.
Statistical Office in Lublin, Poland. Registered unemployment in Lubelskie Voivodship in 2014. http://wuplublin.praca.gov.pl/... (access: 2023.10.05).
27.
Central Statistical Office (GUS). Beneficiaries of social assistance and family benefits in 2012. https://stat.gov.pl/files/gfx/... (access: 2023.10.05).
28.
Program PL 13. Publication of Mortality Rates for Selected Districts. http://archiwum.zdrowie.gov.pl... (access: 2023.23.10).
29.
Nowicki GJ, Ślusarska B, Piasecka H, Bartoszek A, Kocka K, Deluga A. The Status of Cardiovascular Health in Rural and Urban Areas of Janów Lubelski District in Eastern Poland: A Population-Based Study. Int J Environ Res Public Health. 2018;15(11):2388. doi:10.3390/ijerph15112388.
30.
Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452.
31.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13(3):275–286. doi:10.1111/j.1467-789X.2011.00952.x.
32.
Bergman RN, Stefanovski D, Buchanan TA, et al. A better index of body adiposity. Obesity. 2011;19(5):1083–1089. doi:10.1038/oby.2011.38.
33.
World Health Organization. Physical activity. https://www.who.int/news-room/... (access: 2023.10.05).
34.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x.
35.
Ślusarska BJ, Nowicki G, Piasecka H, et al. Validation of the Polish language version of the Patient Health Questionnaire-9 in a population of adults aged 35–64. Ann Agric Environ Med. 2019;26(3):420–424. doi:10.26444/aaem/99246.
36.
Studziński K, Tomasik T, Windak A, et al. The differences in the prevalence of cardiovascular disease, its risk factors, and achievement of therapeutic goals among urban and rural primary care patients in Poland: results from the LIPIDOGRAM 2015 study. J Clin Med. 2021;10(23):5656. doi:10.3390/jcm10235656.
37.
Pigeyre M, Rousseaux J, Trouiller P, et al. How obesity relates to socio-economic status: identification of eating behavior mediators. Int J Obes. 2016;40(11):1794–1801. doi:10.1038/ijo.2016.109.
38.
Saito Y, Oguma Y, Inoue S, Tanaka A, Kobori Y. Environmental and individual correlates of various types of physical activity among community-dwelling middle-aged and elderly Japanese. Int J Environ Res Public Health. 2013;10(5):2028–2042. doi:10.3390/ijerph10052028.
39.
Mesters I, Wahl S, Van Keulen HM. Socio-demographic, medical and social-cognitive correlates of physical activity behavior among older adults (45–70 years): a cross-sectional study. BMC Public Health. 2014;14:647. doi:10.1186/1471-2458-14-647.
40.
Sarlio-Lähteenkorva S, Silventoinen K, Lahti-Koski M, Laatikainen T, Jousilahti P. Socio-economic status and abdominal obesity among Finnish adults from 1992 to 2002. Int J Obes. 2006;30(11):1653–1660. doi:10.1038/sj.ijo.0803319.
41.
Pampel FC, Denney JT, Krueger PM. Obesity, SES, and economic development: a test of the reversal hypothesis. Soc Sci Med. 2012;74(7):1073–1081. doi:10.1016/j.socscimed.2011.12.028.
42.
Suliga E, Kozieł D, Cieśla E, Rębak D, Głuszek S. Dietary Patterns in Relation to Metabolic Syndrome among Adults in Poland: A Cross-Sectional Study. Nutrients. 2017;9(12):1366. doi:10.3390/nu9121366.
43.
Trivedi T, Liu J, Probst J, Merchant A, Jhones S, Martin AB. Obesity and obesity-related behaviors among rural and urban adults in the USA. Rural Remote Health. 2015;15(4):3267.
44.
Reis JP, Bowles HR, Ainsworth BE, Dubose KD, Smith S, Laditka JN. Nonoccupational physical activity by degree of urbanization and U.S. geographic region. Med Sci Sports Exerc. 2004;36(12):2093–2098. doi:10.1249/01.mss.0000147589.98744.85.
45.
Pickett W, King N, Lawson J, et al. Farmers, mechanized work, and links to obesity. Prev Med. 2015;70:59–63. doi:10.1016/j.ypmed.2014.11.012.
46.
Cohen SA, Cook SK, Kelley L, Foutz JD, Sando TA. A Closer Look at Rural-Urban Health Disparities: Associations Between Obesity and Rurality Vary by Geospatial and Sociodemographic Factors. J Rural Health. 2017;33(2):167–179. doi:10.1111/jrh.12207.
47.
Jaacks LM, Slining MM, Popkin BM. Recent underweight and overweight trends by rural-urban residence among women in low- and middle-income countries. J Nutr. 2015;145(2):352–357. doi:10.3945/jn.114.203562.
48.
Abeywickrama HM, Wimalasiri KMS, Koyama Y, et al. Assessment of Nutritional Status and Dietary Pattern of a Rural Adult Population in Dry Zone, Sri Lanka. Int J Environ Res Public Health. 2019;17(1):150. doi:10.3390/ijerph17010150.
49.
Martins-Silva T, Vaz JDS, Mola CL, Assunçao MCF, Tovo-Rodrigues L. Prevalence of obesity in rural and urban areas in Brazil: National Health Survey, 2013. Rev Bras Epidemiol. 2019;22:e190049. doi:10.1590/1980-549720190049.
50.
Siddiquee T, Bhowmik B, Da Vale Moreira NC, et al. Prevalence of obesity in a rural Asian Indian (Bangladeshi) population and its determinants. BMC Public Health. 2015;15:860. doi:10.1186/s12889-015-2193-4.
51.
Moniruzzaman M, Ahmed MS, Zaman MM. Physical activity levels and associated socio-demographic factors in Bangladeshi adults: a cross-sectional study. BMC Public Health. 2017;17(1):59. doi:10.1186/s12889-016-4003-z.
52.
Rezagholizadeh F, Djafarian K, Khosravi S, Shab-Bidar S. A posteriori healthy dietary patterns may decrease the risk of central obesity: findings from a systematic review and meta-analysis. Nutr Res. 2017;41:1–13. doi:10.1016/j.nutres.2017.01.006.
53.
Said-Mohamed R, Prioreschi A, Nyati LH, et al. Rural-urban variations in age at menarche, adult height, leg-length and abdominal adiposity in black South African women in transitioning South Africa. Ann Hum Biol. 2018;45(2):123–132. doi:10.1080/03014460.2018.1442497.
54.
Choi D, Choi S, Son JS, Oh SW, Park SM. Impact of Discrepancies in General and Abdominal Obesity on Major Adverse Cardiac Events. J Am Heart Assoc. 2019;8(18):e013471. doi:10.1161/JAHA.119.013471.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.