Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Registered incidence of acute upper respiratory tract infections diagnosed by primary care physicians in Poland – 5-year retrospective analysis of the national health insurance database
1
Department of Family Medicine, Jagiellonian University Medical College, Kraków, Poland
2
The College of Family Physicians in Poland, Warsaw, Poland
3
Agency for Health Technology Assessment and Tariff System, Warsaw, Poland
Corresponding author
Tomasz Tomasik
1. Department of Family Medicine, Jagiellonian University Medical College, Krakow, Poland 2. The College of Family Physicians in Poland
1. Department of Family Medicine, Jagiellonian University Medical College, Krakow, Poland 2. The College of Family Physicians in Poland
Ann Agric Environ Med. 2024;31(1):100-113
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Upper respiratory tract infection (URTIs), caused by a variety of viruses and sometimes by bacteria, represents the most common acute illness in primary health care. The aim of the study was to explore the registered incidence of URTIs in Poland in the period between 2015–2019, and its burden on the health care system.
Material and methods:
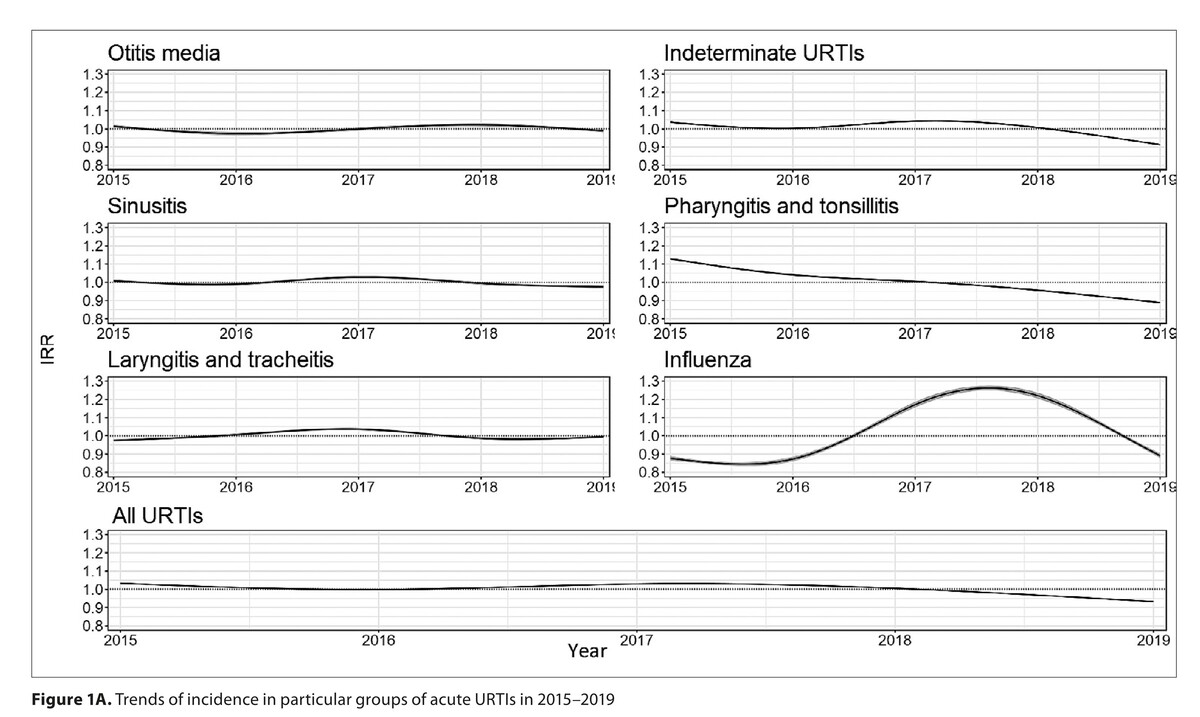
A retrospective analysis was carried out of all medical encounters in Poland registered within the national billing database of public healthcare services. Medical services provided due to acute URTIs were classified according to the ICD-10 codes. Registered Incidence Rate (RIR) was calculated yearly, in a 100,000 population. A generalised additive model was used to calculate the Incidence Rate Ratio (IRR).
Results:
In the analysed 5-year period, acute URTI was diagnosed in 24.3 million patients (61.7% of the whole population registered in PHC). The RIR of all acute URTIs in PHC was 50,762/100,000/year. Nearly 99% of consultations in this group of patients were provided by PHC physicians. Only 0.8% were referred to an OSC consultation and 0.4% were hospitalised. In PHC, indeterminate URTIs were most frequently diagnosed. The estimated IRR for children aged 1–4 years was 1.65 (95% CI: 1.64; 1.66, p<0.01) and for men 0.79 (95% CI: 0.79; 0.79; p<0.01). In the studied period, the number of patients consulted for acute URTI decreased slightly in PHC, but significantly in specialist services.
Conclusions:
The registered incidence of URTIs in Poland burdens mainly PHC physicians. Women and children aged 1–4 years are more frequent users of medical services related to URTIs. It appears that strategies for increasing patient empowerment to provide efficient self-care reducing the utilisation of PHC services are needed.
Upper respiratory tract infection (URTIs), caused by a variety of viruses and sometimes by bacteria, represents the most common acute illness in primary health care. The aim of the study was to explore the registered incidence of URTIs in Poland in the period between 2015–2019, and its burden on the health care system.
Material and methods:
A retrospective analysis was carried out of all medical encounters in Poland registered within the national billing database of public healthcare services. Medical services provided due to acute URTIs were classified according to the ICD-10 codes. Registered Incidence Rate (RIR) was calculated yearly, in a 100,000 population. A generalised additive model was used to calculate the Incidence Rate Ratio (IRR).
Results:
In the analysed 5-year period, acute URTI was diagnosed in 24.3 million patients (61.7% of the whole population registered in PHC). The RIR of all acute URTIs in PHC was 50,762/100,000/year. Nearly 99% of consultations in this group of patients were provided by PHC physicians. Only 0.8% were referred to an OSC consultation and 0.4% were hospitalised. In PHC, indeterminate URTIs were most frequently diagnosed. The estimated IRR for children aged 1–4 years was 1.65 (95% CI: 1.64; 1.66, p<0.01) and for men 0.79 (95% CI: 0.79; 0.79; p<0.01). In the studied period, the number of patients consulted for acute URTI decreased slightly in PHC, but significantly in specialist services.
Conclusions:
The registered incidence of URTIs in Poland burdens mainly PHC physicians. Women and children aged 1–4 years are more frequent users of medical services related to URTIs. It appears that strategies for increasing patient empowerment to provide efficient self-care reducing the utilisation of PHC services are needed.
REFERENCES (38)
1.
Calderaro A, Buttrini M, Farina B, et al. Respiratory Tract Infections and Laboratory Diagnostic Methods: A Study with A Focus on Syndromic Panel-Based Assays. Microorganisms. 2022;10(9). https://doi.org/10.3390/microo....
2.
Korppi M, Heikkilä P, Palmu S, et al. Antibiotic prescribing for children with upper respiratory tract infection: a Finnish nationwide 7-year observational study. Eur J Pediatr. 2022;181(8):2981–2990. https://doi.org/10.1007/s00431....
3.
Jama-Kmiecik A, Frej-Mądrzak M, Sarowska J, et al. Pathogens Causing Upper Respiratory Tract Infections in Outpatients. Adv Exp Med Biol. 2016;934:89–93. https://doi.org/10.1007/5584_2....
4.
Kardos P, Malek FA. Common Cold – an Umbrella Term for Acute Infections of Nose, Throat, Larynx and Bronchi. Pneumologie. 2017;71(4):221–226. https://doi.org/10.1055/s-0042....
5.
Jin X, Ren J, Li R, et al. Global burden of upper respiratory infections in 204 countries and territories, from 1990 to 2019. EClinicalMedicine. 2021;37:100986. https://doi.org/10.1016/j.ecli....
6.
Incze M, Grady D, Gupta A. I Have a Cold-What Do I Need to Know? JAMA Intern Med. 2018;178(9):1288. https://doi.org/10.1001/jamain....
7.
Chan CS. What do patients expect from consultations for upper respiratory tract infections? Fam Pract. 1996;13(3):229–235. https://doi.org/10.1093/fampra....
8.
Bujnowska-Fedak MM, Sapilak BJ, Steciwko A. Epidemiology of diseases and structure of morbidity in family medicine practice. Fam Med Prim Care Rev. 2011;13(2):(pp 135–139), 2011. Date of Publication: April-June 2011.):139.
9.
Pietrzykowska M, Nowicka-Sauer K, Siebert J. Respiratory tract infections in primary health care: prevalence and antibiotic prescribing in a primary care practice during one year. Fam Med Prim Care Rev. 2021;23(2):203–208. https://doi.org/10.5114/fmpcr.....
10.
de Lusignan S, Sherlock J, Akinyemi O, et al. Household presentation of influenza and acute respiratory illnesses to a primary care sentinel network: retrospective database studies (2013–2018). BMC Public Health. 2020;20(1):1748. https://doi.org/10.1186/s12889....
11.
Groeneveld JM, Ballering A V, van Boven K, et al. Sex differences in incidence of respiratory symptoms and management by general practitioners. Fam Pract. 2020;37(5):631–636. https://doi.org/10.1093/fampra....
12.
Kung K, Wong CKM, Wong SYS, et al. Patient presentation and physician management of upper respiratory tract infections: a retrospective study of over 5 million primary clinic consultations in Hong Kong. BMC Fam Pract. 2014;15:95. https://doi.org/10.1186/1471–2....
13.
Hak E, Rovers MM, Kuyvenhoven MM, et al. Incidence of GP-diagnosed respiratory tract infections according to age, gender and high-risk co-morbidity: the Second Dutch National Survey of General Practice. Fam Pract. 2006;23(3):291–294. https://doi.org/10.1093/fampra....
14.
Miyazawa A, Maeno T, Shaku F, et al. Inappropriate use of the emergency department for nonurgent conditions: Patient characteristics and associated factors at a Japanese hospital. J Gen Fam Med. 2019;20(4):146–153. https://doi.org/10.1002/jgf2.2....
15.
Chow A, Keng B, Guo H, et al. Sociodemographic and clinical factors, visit expectations and driving factors for emergency department attendance for uncomplicated upper respiratory tract infection. Emerg Med J. 2022;39(6):427–435. https://doi.org/10.1136/emerme....
16.
Kuchar E, Miśkiewicz K, Szenborn L, et al. Respiratory tract infections in children in primary healthcare in Poland. Adv Exp Med Biol. 2015;835:53–59. https://doi.org/10.1007/5584_2....
17.
American Academy of Family Physicians. Information from your family doctor. The common cold: what you should know. Am Fam Physician. 2007;75(4):522. http://www.ncbi.nlm.nih.gov/pu....
18.
Tan YSL, Hong CY, Chong PN, et al. Knowledge that upper respiratory tract infection resolves on its own is associated with more appropriate health-seeking behaviour and antibiotic cognition. Singapore Med J. 2006;47(6):518–524. http://www.ncbi.nlm.nih.gov/pu....
19.
O’Connor R, O’Doherty J, O’Regan A, et al. Medical management of acute upper respiratory infections in an urban primary care out-of-hours facility: cross-sectional study of patient presentations and expectations. BMJ Open. 2019;9(2):e025396. https://doi.org/10.1136/bmjope....
20.
McKay R, Mah A, Law MR, et al. Systematic Study of Factors Associated with Antibiotic Prescribing for Respiratory Tract Infections. Antimicrob Agents Chemother. 2016;60(7):4106–4118. https://doi.org/10.1128/AAC.00....
21.
Sauro A, Barone F, Blasio G, et al. Do influenza and acute respiratory infective diseases weigh heavily on general practitioners’ daily practice? Eur J Gen Pract. 2006;12(1):34–36. https://doi.org/10.1080/138147....
22.
Dal Negro RW, Zanasi A, Turco P, et al. Influenza and influenza-like syndromes: the subjects’ beliefs, the attitude to prevention and treatment, and the impact in Italian general population. Multidiscip Respir Med. 2018;13:7. https://doi.org/10.1186/s40248....
23.
Lancet Respiratory Medicine. Primary care at the heart of respiratory medicine in the UK. Lancet Respir Med. 2014;2(2):83. https://doi.org/10.1016/S2213–....
24.
Gulliford M, Latinovic R, Charlton J, et al. Selective decrease in consultations and antibiotic prescribing for acute respiratory tract infections in UK primary care up to 2006. J Public Health (Oxf). 2009;31(4):512–520. https://doi.org/10.1093/pubmed....
25.
Falagas ME, Mourtzoukou EG, Vardakas KZ. Sex differences in the incidence and severity of respiratory tract infections. Respir Med. 2007;101(9):1845–1863. https://doi.org/10.1016/j.rmed....
26.
de Hoog MLA, Venekamp RP, van der Ent CK, et al. Impact of early daycare on healthcare resource use related to upper respiratory tract infections during childhood: prospective WHISTLER cohort study. BMC Med. 2014;12:107. https://doi.org/10.1186/1741–7....
27.
Alexandrino AS, Santos R, Melo C, et al. Risk factors for respiratory infections among children attending day care centres. Fam Pract. 2016;33(2):161–166. https://doi.org/10.1093/fampra....
28.
Reed C, Chaves SS, Daily Kirley P, et al. Estimating influenza disease burden from population-based surveillance data in the United States. PLoS One. 2015;10(3):e0118369. https://doi.org/10.1371/journa....
29.
Thompson WW, Comanor L, Shay DK. Epidemiology of seasonal influenza: use of surveillance data and statistical models to estimate the burden of disease. J Infect Dis. 2006;194 Suppl:S82–91. https://doi.org/10.1086/507558.
30.
Bernadou A, Sommen C, Pivette M, et al. Estimating the burden of influenza-attributable severe acute respiratory infections on the hospital system in Metropolitan France, 2012–2018. BMC Infect Dis. 2023;23(1):128. https://doi.org/10.1186/s12879....
31.
Yuan Y, Wang R-T, Xia J, et al. Interventions for preventing influenza: An overview of Cochrane systematic studys and a Bayesian network metaanalysis. J Integr Med. 2021;19(6):503–514. https://doi.org/10.1016/j.joim....
32.
Demicheli V, Jefferson T, Ferroni E, et al. Vaccines for preventing influenza in healthy adults. Cochrane database Syst Rev. 2018;2(2):CD001269. https://doi.org/10.1002/146518....
33.
Demicheli V, Jefferson T, Di Pietrantonj C, et al. Vaccines for preventing influenza in the elderly. Cochrane database Syst Rev. 2018;2(2):CD004876. https://doi.org/10.1002/146518....
34.
Jefferson T, Rivetti A, Di Pietrantonj C, et al. Vaccines for preventing influenza in healthy children. Cochrane database Syst Rev. 2018;2(2):CD004879. https://doi.org/10.1002/146518....
35.
Hayes C V, Mahon B, Sides E, et al. Empowering Patients to Self-Manage Common Infections: Qualitative Study Informing the Development of an Evidence-Based Patient Information Leaflet. Antibiot (Basel, Switzerland). 2021;10(9). https://doi.org/10.3390/antibi....
36.
Wang DY, Eccles R, Bell J, et al. Management of acute upper respiratory tract infection: the role of early intervention. Expert Rev Respir Med. 2021;15(12):1517–1523. https://doi.org/10.1080/174763....
37.
Zhao Y, Dong BR, Hao Q. Probiotics for preventing acute upper respiratory tract infections. Cochrane database Syst Rev. 2022;8(8):CD006895. https://doi.org/10.1002/146518....
38.
Montesinos-Guevara C, Buitrago-Garcia D, Felix ML, et al. Vaccines for the common cold. Cochrane database Syst Rev. 2022;12(12):CD002190. https://doi.org/10.1002/146518....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.