Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Analysis of functional efficiency and risk of falls in patients with different types of dementia – preliminary observations
1
Military Institute of Hygiene and Epidemiology, Warsaw, Poland
2
Medical University, Lodz, Poland
Corresponding author
Ann Agric Environ Med. 2024;31(1):114-118
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Dementia is a multifactorial neurological disease that affects 50 million people worldwide. It is a disorder that impairs cognitive functions, functional efficiency, balance and gait. It contributes to an increased risk of falls, reduces independence in everyday activities and deepens disability. The aim of the study was to investigate the correlation between dementia and independence related to functional efficiency and risk of falls in the elderly.
Material and methods:
The eligibility criterion for participation in the study was age over 60, the presence of cognitive disorders, including dementia, and the ability to move with the use of orthopaedic equipment or independently. A total of 51 people participated in the study, including 13 people who underwent rehabilitation procedures. Each subject was evaluated once for cognitive abilities using two types of tests: the ADL scale, MMSE (Mini-Mental state Examination) and three physical fitness tests: SPPB (Short Physical Performance Battery), TUG (Timed Up & Go) and FRT (Functional Reach Test).
Results:
The average score of the MMSE test was 13.29±6.23 points, the average of the ADL scale was 4.20±1.23 points. A positive correlation was found between the level of dementia and the independence of the examined person, as well as a positive relationship between the MMSE test and the result of the Functional Reach Test, and the relationship between the ADL scale and the SPPB and ‘Get-Up and Go’ tests.
Conclusions:
It has been demonstrated inter alia that static balance and functional efficiency depends on the patient’s independence in everyday activities, and the level of dementia may suggest the patient’s dynamic balance. In addition, the need for a broader analysis of targeted studies was recognized to confirm the conclusions obtained.
Dementia is a multifactorial neurological disease that affects 50 million people worldwide. It is a disorder that impairs cognitive functions, functional efficiency, balance and gait. It contributes to an increased risk of falls, reduces independence in everyday activities and deepens disability. The aim of the study was to investigate the correlation between dementia and independence related to functional efficiency and risk of falls in the elderly.
Material and methods:
The eligibility criterion for participation in the study was age over 60, the presence of cognitive disorders, including dementia, and the ability to move with the use of orthopaedic equipment or independently. A total of 51 people participated in the study, including 13 people who underwent rehabilitation procedures. Each subject was evaluated once for cognitive abilities using two types of tests: the ADL scale, MMSE (Mini-Mental state Examination) and three physical fitness tests: SPPB (Short Physical Performance Battery), TUG (Timed Up & Go) and FRT (Functional Reach Test).
Results:
The average score of the MMSE test was 13.29±6.23 points, the average of the ADL scale was 4.20±1.23 points. A positive correlation was found between the level of dementia and the independence of the examined person, as well as a positive relationship between the MMSE test and the result of the Functional Reach Test, and the relationship between the ADL scale and the SPPB and ‘Get-Up and Go’ tests.
Conclusions:
It has been demonstrated inter alia that static balance and functional efficiency depends on the patient’s independence in everyday activities, and the level of dementia may suggest the patient’s dynamic balance. In addition, the need for a broader analysis of targeted studies was recognized to confirm the conclusions obtained.
REFERENCES (36)
1.
Sytuacja osób starszych w Polsce w 2020 r. Available online: https://stat.gov.pl/files/gfx/... (access: 2023.01.30).
2.
Murkowski R. Stan i perspektywy procesu starzenia się ludności na świecie. Folia Oeconomica FOE. 2020; 2(347): 7–21. doi:10.18778/0208–6018.347.01.
3.
Kędziora-Kornatowska K, Polak-Szabela A. Zaburzenia otępienne u osób powyżej 60. roku życia [in:] Cybulski M, Waszkiewicz N. Psychogeriatria, PZWL Wydawnictwo Lekarskie 2017; pp. 31.
4.
Borzym A, Michalak G. Otępienie [in:] Jarema M. Otępienia i organiczne zaburzenia psychiczne w praktyce lekarza POZ, PZWL Wydawnictwo Lekarskie 2018; pp. 18.
5.
Zasadzka E, Jóźwiak A. Otępienie [in:] Wieczorkowska-Tobis, K Fizjoterapia w geriatrii, PZWL Wydawnictwo Lekarskie 2011; pp. 95–96.
7.
Bień B. Zmiany narządowe towarzyszące procesowi starzenia się [in:] Wieczorkowska-Tobis K, Talarska D. Geriatria i pielęgniarstwo geriatryczne, PZWL Wydawnictwo Lekarskie 2017; pp. 60.
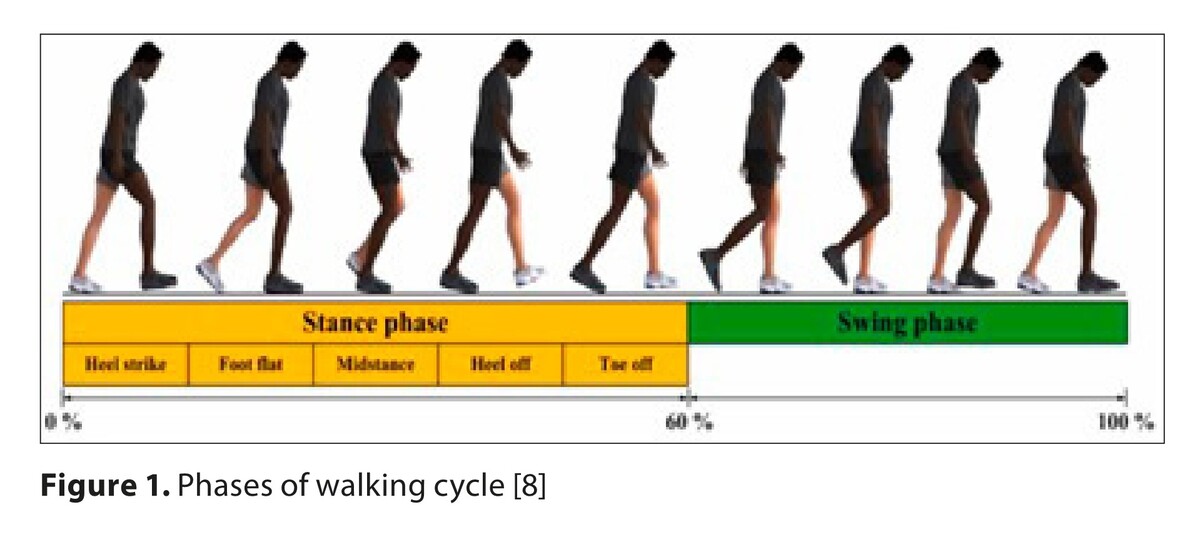
8.
Jamari J, Ammarullah M I, Santoso G, Sugiharto S, Supriyono T, Permana M S, Tri Indah Winarni, van der Heide E. Adopted walking condition for computational simulation approach on bearing of hip joint prosthesis: review over the past 30 years Heliyon. 2022; Dec 5;8(12):e 12050 doi: 10.1016/.heliyon.2022.e12050.
9.
Bień B. Zmiany narządowe towarzyszące procesowi starzenia się [in:] Wieczorkowska-Tobis K, Talarska D. Geriatria i pielęgniarstwo geriatryczne, PZWL Wydawnictwo Lekarskie 2017; pp. 61.
10.
Krajewska-Włodarczyk M. Modyfikacje chrząstki stawowej w procesie starzenia. Geriatria 2017; 11: 135–141.
11.
Czerwiński E, Berwecka K, Boczoń K. Sarkopenia – patogeneza, diagnostyka i leczenie. PZWL Wydawnictwo Lekarskie 2015; pp.185.
12.
Hiroyuki T, Yuma N, Daiki I, Yasuhiro O, Keita F, Takashi N. Clinical factors associated with activities of daily living and their decline in patients with severe dementia. Psychogeriatrics. 2020; 20(3): 327–336. doi:10.1111/psyg.12502.
13.
Janssen I, Heymsfield S, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Ger Soc. 2002; 50: 889–896.
14.
Katz S, Downs T D, Cash H R, Grotz R C. Progress in development of the index of ADL Gerontologist. 1970; 10(1):20–30. doi: 10.1093/geront/10.1_part_1.20.
15.
Folstein MF, Folstein SE, McHugh PR. „Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12(3):189–98.
16.
Gallegos M, Morgan ML, Cervigni M, Martino P, Murray J, Calandra M, Razumovskiy A, Caycho-Rodríguez T, Gallegos WLA. 45 Years of the mini-mental state examination (MMSE): A perspective from ibero-america. Dement Neuropsychol. 2022; 16(4):384–387.
17.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function:association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):85–94.
18.
Podsiadlo D, Richardson S. The timed “Up &Go”:a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
19.
Szczepańska-Gieracha J, Kowalska J, Rymaszewska J. Problemy długoterminowej hospitalizacji i rehabilitacji osób starszych z zaburzeniami poznawczymi. Psychogeriatr Pol. 2011; 8(1):1–10.
20.
Alzheimer’s Disease International. Available online: https://www.alz.co.uk/research... (access: 30.01.2023).
21.
Ferri C P, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, Hall K, Hasegawa K, Hendrie H, Huang Y, Jorm A, Mathers C, Menezes PR, Rimmer E, Scazufca M. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005; 9503: 2112–2117.
22.
Chan K Y, Adeloye D, Asante K P, Calia C, Campbell H, Danso S O, Juvekar S, Luz S, Mohan D, Muniz-Terrera G, Nitrini R, Noroozia M, Nulkar- Nyame S, Paralikar V, Rodriguez M A P, Poon A N, Reidpath D D, Rudan I, Stephan B C, Su T T, Wang H, Wilkinson H, Yassuda M S, Yu X, Ritchie C Tackling dementia globally: the Global Dementia Prevention Program (GloDePP) collaboration. J Glob Health. 2019; 9(2): 020103. doi:10.7189/jogh.09.020103.
23.
Skubal A, Ciąpała G, Ćwirlej-Sozańska A, Wiśniowska-Szurlej A, Wilmowska-Pietruszyńska A. Assessment of functional capacity and the risk of falls in the elderly with mild and moderate stage dementia. Medical Rev. 2016; 14(4): 427–438. doi: 10.15584/medrev.2016.4.6.
24.
Bürge E, Berchtold A, Maupetit C, Bourquin N, Guntena A, Dacraux D, Zumbacha S, Peeters A, Kuhne M. Does physical exercise improve ADL capacities in people over 65 years with moderate or severe dementia hospitalized in an acute psychiatric setting? A multisite randomized clinical trial. Int Psychogeriat. 2017; 29(2): 323–332. doi:10.1017/S1041610216001460.
25.
Hiroyuki T, Yuma N, Daiki I, Yasuhiro O, Keita F, Takashi N. Clinical factors associated with activities of daily living and their decline in patients with severe dementia. Psychogeriatrics. 2020; 29(2): 323–332. doi:10.1111/psyg.12502.
26.
Helvik A, Engedal K, Benth J, Selbak G A. 52 month follow-up of functional decline in nursing home residents – Degree of dementia contribute. BMC Geriatrics. 2014; 14(45): 1–10.
27.
Dos Anjos Dixe M, Madeira C, Alves S, Henriques M A, Baixinho C L. Gait Abilty and Muscle Strenght in Institutionalized Older Person with and without Cognitive Decline and Association with Falls Int J Environ Res Public Health. 2021; 3;18(21):11543. doi: 10.3390/ijerph182111543.
28.
Lindbergh C A, Dishman R K, Miller L S. Functional Disability in Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Neuropsychol Rev. 2016; 26(2): 129–159. doi:10.1007/s11065–016–9321–5.
29.
Reppermund S, Brodaty H, Crawford J, Kochan N, Draper B, Slavin M, Sachdev P. Impairment in instrumental activities of daily living with high cognitive demand is an early marker of mild cognitive impairment: The Sydney Memory and Ageing Study. Psychol Med. 2013; 43(11): 2437–2445. doi:10.1017/S003329171200308X.
30.
Staszczak-Gawełda I, Szczygielska-Babiuch A, Puzio G, Krupnik S, Stopa A, Czesak J, Żak M. Ocena sprawności funkcjonalnej osób starszych z lekkim otępieniem, Gerontol Pol. 2013; 4: 127–132.
31.
Taylor M, Close J. Dementia, Handb Clin Neurol. 2018; 159: 303–321. doi: 10.1016/B978–0–444–63916–5.00019–7.
32.
Yoon B, Choi S, Jeong J, Park K, Kim E, Hwang J, Jang J, Kim H, Hong J, Lee J, Kang J, Yoon S. Balance and Mobility Performance Along the Alzheimer’s Disease Spectrum. J Alzheimers Dis. 2019; 73(2): 633–644. doi: 10.3233/JAD-190601].
33.
Rajtar-Zembaty A, Rajtar-Zembaty J, Starowicz-Filip A. The relationship between cognitive functioning and functional capability in older adult. Geriatria 2016; 10: 78–84.
34.
Sondell A, Littbrand H, Holmberg H, Lindelöf N, Rosendahl E. Is the Effect of a High-Intensity Functional Exercise Program on Functional Balance Influenced by Applicability and Motivation among Older People with Dementia in Nursing Homes? J Nutr Health Aging. 2019; 23(10): 1011–1020. doi: 10.1007/s12603–019–1269–8.
35.
Toots A, Wiklund R, Littbrand H, Nordin E, Nordström P, Lundin-Olsson L, Gustafson Y, Rosendahl E. The Effects of Exercise on Falls in Older People With Dementia Living in Nursing Homes: A Randomized Controlled Trial. J Am Med Dir Assoc. 2019; 20(7): 835–842. doi: 10.1016/j.jamda.2018.10.009.
36.
Ansai JH, Andrade LP, Masse FAA, Gonçalves J, Takahashi ACM, Vale FAC, Rebelatto JR. Risk Factors for Falls in Older Adults With Mild Cognitive Impairment and Mild Alzheimer Disease. J Geriatr Phys Ther. 2019; 42(3):E116-E121. doi:10.1519/JPT.0000000000000135.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.