Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Changes in the body mass of adult residents of rural and urban areas in the initial months of the COVID-19 pandemic vs. their mental, physical and sexual health
1
Faculty Of Health Sciences, Medical University, Warsaw, Poland
2
Department of Humanization of Health Care and Sexology, Collegium Medicum, University of Zielona Góra, Poland
3
Department of Biomedical Aspects of Development and Sexology, Faculty of Education, Warsaw University, Poland
Corresponding author
Maciej Białorudzki
Faculty Of Health Sciences Medical University of Warsaw, Żwirki i Wigury 61, 512-523, Warszawa, Poland
Faculty Of Health Sciences Medical University of Warsaw, Żwirki i Wigury 61, 512-523, Warszawa, Poland
Ann Agric Environ Med. 2021;28(4):667-675
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
A change in the body mass may be one of the health consequence of the COVID-19 pandemic, and may affect the health condition measured in many dimensions. The paper aims at assessment of the level and determinants of the body mass changes and stress level in the initial months of the COVID-19 pandemic, and the interrelation of these two factors.
Material and methods:
Data were collected in June 2020, as a cross-sectional on-line survey. The representative sample of 2,535 Poles aged 18–65 was analysed. The main outcome is the Cohen’s stress index PSS-4. Among thirteen independent variables, five were related to the change observed during the pandemic (including the body mass change and satisfaction with sexual life).
Results:
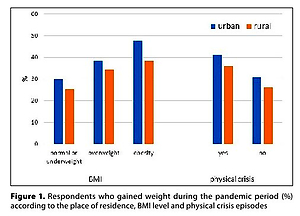
Increase of the body mass within the period of the pandemic was declared by 33.9% of the respondents, including 36.1% in urban and 30.9% in rural areas (p=0.026). The average increase of body mass was 5.11 kg. The increase of body mass was related to the existing overweight and obesity, occurrence of chronic diseases, episodes of physical and mental crisis, and decrease of interest in sexual activity. The average index of stress in the initial months of the pandemic was 6.38±2.94. Multivariate regression analysis showed eight independent predictors of stress in the whole group, seven in towns and five in rural areas. The significance of the relationship with the body mass increase was proved only among residents of rural areas.
Conclusions:
The initial months of the COVID-19 pandemic were reflected, to a different extent, among residents of urban and rural areas. Body mass change and sexual health indicators remained significant predictors of stress level, even after analyses were corrected for other covariates.
A change in the body mass may be one of the health consequence of the COVID-19 pandemic, and may affect the health condition measured in many dimensions. The paper aims at assessment of the level and determinants of the body mass changes and stress level in the initial months of the COVID-19 pandemic, and the interrelation of these two factors.
Material and methods:
Data were collected in June 2020, as a cross-sectional on-line survey. The representative sample of 2,535 Poles aged 18–65 was analysed. The main outcome is the Cohen’s stress index PSS-4. Among thirteen independent variables, five were related to the change observed during the pandemic (including the body mass change and satisfaction with sexual life).
Results:
Increase of the body mass within the period of the pandemic was declared by 33.9% of the respondents, including 36.1% in urban and 30.9% in rural areas (p=0.026). The average increase of body mass was 5.11 kg. The increase of body mass was related to the existing overweight and obesity, occurrence of chronic diseases, episodes of physical and mental crisis, and decrease of interest in sexual activity. The average index of stress in the initial months of the pandemic was 6.38±2.94. Multivariate regression analysis showed eight independent predictors of stress in the whole group, seven in towns and five in rural areas. The significance of the relationship with the body mass increase was proved only among residents of rural areas.
Conclusions:
The initial months of the COVID-19 pandemic were reflected, to a different extent, among residents of urban and rural areas. Body mass change and sexual health indicators remained significant predictors of stress level, even after analyses were corrected for other covariates.
REFERENCES (38)
1.
Regulation of the Minister of Health of 20 March 2020 on the declaration of an epidemic in the territory of the Republic of Poland. (DzU z 2020 r. poz. 491). Polish. (access: 2021.08.14).
2.
Moccia L, Janiri D, Pepe M, et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun. 2020; 87: 75–79. doi: 10.1016/j.bbi.2020.04.048.
3.
Pfefferbaum B, North CS. Mental Health and the Covid-19 Pandemic. N Engl J Med. 2020; 383(6): 510–512. doi: 10.1056/NEJMp2008017.
4.
Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020; 395(10227): 912–920. doi: 10.1016/S0140-6736(20)30460-8.
5.
Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020; 7(10): 883–892. doi: 10.1016/S2215-0366(20)30308-4.
6.
Kumar A, Nayar KR. COVID 19 and its mental health consequences. J Ment Health. 2021; 30(1): 1–2. doi: 10.1080/09638237.2020.1757052.
7.
Yau YH, Potenza MN. Stress and eating behaviors. Minerva Endocrinol. 2013; 38(3): 255–67.
8.
Maniscalco JW, Kreisler AD, Rinaman L. Satiation and stress-induced hypophagia: examining the role of hindbrain neurons expressing prolactin-releasing Peptide or glucagon-like Peptide 1. Front Neurosci. 2012; 6: 199. doi: 10.3389/fnins.2012.00199.
9.
Razzoli M, Bartolomucci A. The Dichotomous Effect of Chronic Stress on Obesity. Trends Endocrinol Metab. 2016; 27(7): 504–515. doi: 10.1016/j.tem.2016.04.007.
10.
Maniscalco JW, Rinaman L. Interoceptive modulation of neuro-endocrine, emotional, and hypophagic responses to stress. Physiol Behav. 2017; 176: 195–206. doi: 10.1016/j.physbeh.2017.01.027.
11.
Spinosa J, Christiansen P, Dickson JM, Lorenzetti V, Hardman CA. From Socioeconomic Disadvantage to Obesity: The Mediating Role of Psychological Distress and Emotional Eating. Obesity (Silver Spring). 2019; 27(4): 559–564. doi: 10.1002/oby.22402.
12.
Almandoz JP, Xie L, Schellinger JN, et al. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin Obes. 2020; 10(5): e12386. doi: 10.1111/cob.12386.
13.
Batlle-Bayer L, Aldaco R, Bala A, et al. Environmental and nutritional impacts of dietary changes in Spain during the COVID-19 lockdown. Sci Total Environ. 2020; 748: 141410. doi: 10.1016/j.scitotenv.2020.141410.
14.
Sidor A, Rzymski P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients. 2020; 12(6). doi: 10.3390/nu12061657.
15.
Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020; 12(6). doi: 10.3390/nu12061583.
16.
Phillipou A, Meyer D, Neill E, et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19pandemic in Australia: Initial results from the COLLATE project. Int J Eat Disord. 2020; 53(7): 1158–1165. doi: 10.1002/eat.23317.
17.
Wojtynia B, Goryński P, editor. Health status of Polish population and its determinants 2020.
18.
Flentje A, Obedin-Maliver J, Lubensky ME, Dastur Z, Neilands T, Lunn MR. Depression and Anxiety Changes Among Sexual and Gender Minority People Coinciding with Onset of COVID-19 Pandemic. J Gen Intern Med. 2020; 35(9): 2788–2790. doi: 10.1007/s11606-020-05970-4.
19.
Jacob L, Smith L, Butler L, et al. Challenges in the Practice of Sexual Medicine in the Time of COVID-19 in the United Kingdom. J Sex Med. 2020; 17(7): 1229–1236. doi: 10.1016/j.jsxm.2020.05.001.
20.
World Health Organization and others. Sexual health and its linkages to reproductive health: an operational approach, 2017. https://www.who.int/reproducti... sexual_health/sh-linkages-rh/en/ (access: 2021.08.14).
21.
Li G, Tang D, Song B, et al. Impact of the COVID-19 Pandemic on Partner Relationships and Sexual and Reproductive Health: Cross-Sectional, Online Survey Study. J Med Internet Res. 2020; 22(8): e20961. doi: 10.2196/20961.
22.
Fuchs A, Matonóg A, Pilarska J, et al. The Impact of COVID-19 on Female Sexual Health. Int J Environ Res Public Health. 2020; 17(19) doi: 10.3390/ijerph17197152.
23.
Larsen SH, Wagner G, Heitmann BL. Sexual function and obesity. Int J Obes (Lond). 2007; 31(8): 1189–98. doi: 10.1038/sj.ijo.0803604.
24.
Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res (Korean Soc Nurs Sci). 2012; 6(4): 121–7. doi: 10.1016/j.anr.2012.08.004.
25.
Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020; 16(1): 57. doi: 10.1186/s12992-020-00589-w.
26.
Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007; 23(11–12): 887–94. doi: 10.1016/j.nut.2007.08.008.
27.
Simon GE, Von Korff M, Saunders K, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006; 63(7): 824–30. doi: 10.1001/archpsyc.63.7.824.
28.
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020; 323(20): 2052–2059. doi: 10.1001/jama.2020.6775.
29.
Laitner MH, Minski SA, Perri MG. The role of self-monitoring in the maintenance of weight loss success. Eat Behav. 2016; 21: 193–7. doi: 10.1016/j.eatbeh.2016.03.005.
30.
Zhang J, Zhu L, Li S, et al. Rural-urban disparities in knowledge, behaviors, and mental health during COVID-19 pandemic: A community-based cross-sectional survey. Medicine (Baltimore). 2021; 100(13): e25207. doi: 10.1097/MD.0000000000025207.
31.
Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. 2020; 78: 185–193. doi: 10.1016/j.ijsu.2020.04.018.
32.
Hossain MM, Sultana A, Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiol Health. 2020; 42: e2020038. doi: 10.4178/epih.e2020038.
33.
Arafat SMY, Alradie-Mohamed A, Kar SK, Sharma P, Kabir R. Does COVID-19 pandemic affect sexual behaviour? A cross-sectional, cross-national online survey. Psychiatry Res. 2020; 289: 113050. doi: 10.1016/j.psychres.2020.113050.
34.
Li W, Li G, Xin C, Wang Y, Yang S. Challenges in the Practice of Sexual Medicine in the Time of COVID-19 in China. J Sex Med. 2020; 17(7): 1225–1228. doi: 10.1016/j.jsxm.2020.04.380.
35.
Coombe J, Kong FYS, Bittleston H, et al. Love during lockdown: findings from an online survey examining the impact of COVID-19 on the sexual health of people living in Australia. Sex Transm Infect. 2021; 97(5): 357–362. doi: 10.1136/sextrans-2020-054688.
36.
Izdebski Z. Health and sexual life of Poles in 2017. Research study in the background since 1997. Wydawnictwo Uniwersytetu Warszawskiego Warsaw, 2020; 1.
37.
Hamilton LD, Meston CM. Chronic stress and sexual function in women. J Sex Med. 2013; 10(10): 2443–54. doi:10.1111/jsm.12249.
38.
Wang C, Pan R, Wan X, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020; 17(5). doi: 10.3390/ijerph17051729.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.