Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Opinion of teenagers on smoking-free policy in public places and its determinants – evidence from a global youth tobacco survey in five European countries
1
Department of Hygiene and Epidemiology, Medical University, Łódź, Poland
These authors had equal contribution to this work
Corresponding author
Beata Świątkowska
Department of Hygiene and Epidemiology, Medical University of Lodz, Żeligowskiego 7/9, 90-752, Łódź, Poland
Department of Hygiene and Epidemiology, Medical University of Lodz, Żeligowskiego 7/9, 90-752, Łódź, Poland
Ann Agric Environ Med. 2024;31(2):219-226
KEYWORDS
TOPICS
- Health effects of chemical pollutants in agricultural areas , including occupational and non-occupational effects of agricultural chemicals (pesticides, fertilizers) and effects of industrial disposal (heavy metals, sulphur, etc.) contaminating the atmosphere, soil and water
- State of the health of rural communities depending on various factors: social factors, accessibility of medical care, etc.
ABSTRACT
Introduction and objective:
Smoking-free policies protect non-smokers from the negative effects of smoking, but many young adults still use products containing nicotine. The aim of this article is to analyze the factors that influence young people’s attitudes towards the ban on smoking in public places.
Material and methods:
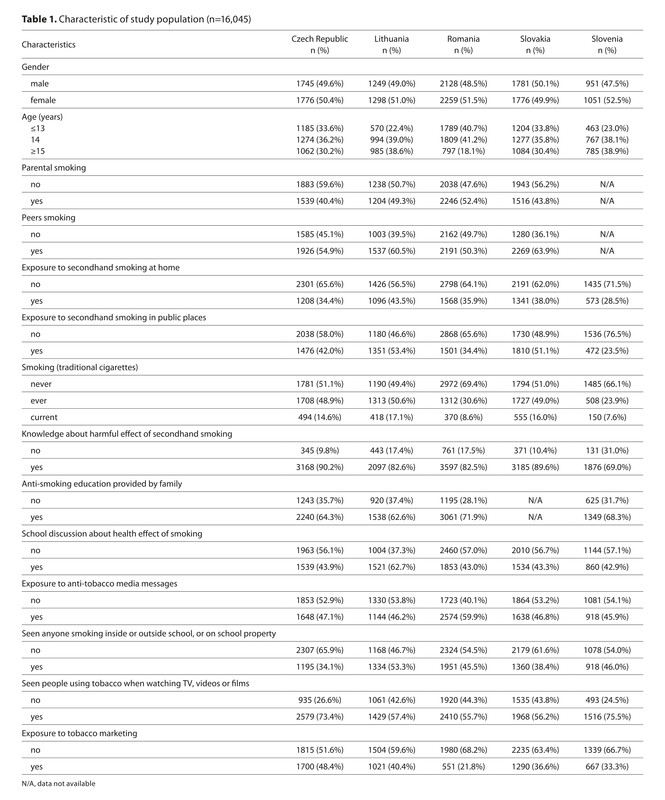
Data were obtained from a representative sample of young adults aged 13–15 from the Global Youth Tobacco Survey (GYTS) conducted in the Czech Republic, Lithuania, Romania, Slovakia and Slovenia. Logistic regression analysis was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs).
Results:
At least a quarter of the adolescents were exposed to cigarette smoking, about 40% have parents who smoke and over 50% declared that they have peers who smoke. A higher proportion of adolescents have knowledge about the harmful effects of second-hand smoking (62.6–71.9%), but at least one-fifth of young people are still exposed to the marketing of tobacco products. Compared with current smoking, those with never smoked were significantly associated with positive attitude toward to restricting smoking in all five analyzed countries, with an AOR= 4.74 (95% CI: 3.61–6.23), AOR=4.33 (95% CI: 2.32–8.07), AOR=2.85 (95% CI: 2.19–3.70) and AOR=2.45 (95% CI: 1.65–3.64), respectively. Gender, age, smoking, exposure to second-hand smoke, knowledge about the harmful effects of smoking, anti-smoking education, seeing people using tobacco and exposure to tobacco marketing, were significantly associated with the attitudes of young people towards restricting smoking in public places.
Conclusions:
The study provides useful information on factors that should be taken into account when planning anti-smoking strategies so that young people are able to resist the pressure to use tobacco products.
Smoking-free policies protect non-smokers from the negative effects of smoking, but many young adults still use products containing nicotine. The aim of this article is to analyze the factors that influence young people’s attitudes towards the ban on smoking in public places.
Material and methods:
Data were obtained from a representative sample of young adults aged 13–15 from the Global Youth Tobacco Survey (GYTS) conducted in the Czech Republic, Lithuania, Romania, Slovakia and Slovenia. Logistic regression analysis was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs).
Results:
At least a quarter of the adolescents were exposed to cigarette smoking, about 40% have parents who smoke and over 50% declared that they have peers who smoke. A higher proportion of adolescents have knowledge about the harmful effects of second-hand smoking (62.6–71.9%), but at least one-fifth of young people are still exposed to the marketing of tobacco products. Compared with current smoking, those with never smoked were significantly associated with positive attitude toward to restricting smoking in all five analyzed countries, with an AOR= 4.74 (95% CI: 3.61–6.23), AOR=4.33 (95% CI: 2.32–8.07), AOR=2.85 (95% CI: 2.19–3.70) and AOR=2.45 (95% CI: 1.65–3.64), respectively. Gender, age, smoking, exposure to second-hand smoke, knowledge about the harmful effects of smoking, anti-smoking education, seeing people using tobacco and exposure to tobacco marketing, were significantly associated with the attitudes of young people towards restricting smoking in public places.
Conclusions:
The study provides useful information on factors that should be taken into account when planning anti-smoking strategies so that young people are able to resist the pressure to use tobacco products.
ACKNOWLEDGEMENTS
This paper uses data from the Global Youth Tobacco
Survey (GYTS). GYTS is supported by the World Health
Organization and the US Centers for Disease Control and
Prevention.
REFERENCES (24)
1.
Park Lee E, Ren C, Cooper M, et al. Tobacco Product Use Among Middle and High School Students – United States, 2022. Morbidity and Mortality Weekly Report. 2022;71:45. https://www.cdc.gov/mmwr/volum... (access: 2023.08.28).
2.
Lagerweij NA, Kuipers MAG, et al. The visibility of smoking in Europe and its relationship with youth’s positive beliefs about smoking. Int J Public Health. 2019;64(9):1335–1344. https://doi:10.1007/s00038-019....
3.
Kang H, Cho SI. Cohort effects of tobacco control policy: evidence to support a tobacco-free norm through smoke-free policy. Tob Control. 2020;29(1):96–102. https://doi:10.1136/tobaccocon....
4.
U.S. Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2012. https://www.ncbi.nlm.nih.gov/b... (access: 2023.08.28).
5.
Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—2014. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. https://www.cdc.gov/tobacco/st... (access:2023.08.28).
6.
The Act of 9 November 1995 on Health Protection against the Consequences of Tobacco and Tobacco Products. J Laws 1996, No. 10, item 55, as amended.
7.
Jankowski M, Rees V, Zgliczyński WS, et al. Self-reported secondhand smoke exposure following the adoption of a national smoke-free policy in Poland: analysis of serial, cross-sectional, representative surveys, 2009–2019. BMJ Open. 2020;10(9):e039918. https://doi:10.1136/bmjopen-20....
8.
Catalano MA, Gilleskie DB. Impacts of local public smoking bans on smoking behaviors and tobacco smoke exposure. Health Econ. 2021;30(8):1719–1744. https://doi:10.1002/hec.4280.
9.
Reitsma MB, Flor LS, Mullany EC, et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and initiation among young people in 204 countries and territories, 1990–2019. Lancet Public Health. 2021;6(7):e472-e481. https://doi: 10.1016/S2468-2667(21)00102-X.
10.
Centers for Disease Control and Prevention. Global tobacco surveillance system data. https://www.cdc.gov/tobacco/gl... (access: 2023.08.28).
11.
World Health Organization. Global Youth Tobacco Survey. https://www.who.int/teams/nonc... (access: 2023.08.28).
12.
GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet. 2021;397(10292):2337–2360. https://doi:10.1016/S0140-6736....
13.
Goodchild M, Nargis N, Tursan d’Espaignet E. Global economic cost of smoking-attributable diseases. Tobacco Control. 2018;27:58–64. https://doi: 10.1136/tobaccocontrol-2016-053305.
14.
World Health Organization. WHO global report on trends in prevalence of tobacco use 2000–2025, fourth edition. WHO, Geneva, 2021 https://www.who.int/publicatio... (access: 2023.08.28).
15.
Wen H, Xie C, Shi F, et al. Trends in Deaths Attributable to Smoking in China, Japan, United Kingdom, and United States From 1990 to 2019. Int J Public Health. 2022;67:1605147. https://doi: 10.3389/ijph.2022.1605147.
16.
Harvey J, Chadi N. Canadian Paediatric Society, Adolescent Health Committee. Preventing smoking in children and adolescents: Recommendations for practice and policy. Paediatr Child Health. 2016;21(4):209–21. https://doi:10.1093/pch/21.4.2....
17.
World Health Organization. WHO Report on the Global Tobacco Epidemic, 2009: implementing smoke-free environments. https://apps.who.int/iris/hand... (access: 2023.08.28).
18.
Polanska K, Znyk M, Kaleta D. Susceptibility to tobacco use and associated factors among youth in five central and eastern European countries. BMC Public Health. 2022;11;22(1):72. https://doi:10.1186/s12889-022....
19.
National Cancer Institute. Influence of Tobacco Marketing on Smoking Behavior. https://cancercontrol.cancer.g... (access: 2023.08.28).
20.
Levy DT, Wijnhoven TMA, Levy J, et al. Potential health impact of strong tobacco control policies in 11 South Eastern WHO European Region countries. Eur J Public Health. 2018;28(4):693–701. https://doi: 10.1093/eurpub/cky028.
21.
Flor LS, Reitsma MB, Gupta V, et al. The effects of tobacco control policies on global smoking prevalence. Nat Med. 2021;27(2):239–243. https://doi:10.1038/s41591-020....
22.
Jenssen BP, Walley SC, Boykan R, et al. Protecting Children and Adolescents From Tobacco and Nicotine. Pediatrics. 2023;151(5):e2023061804. https://doi:10.1542/peds.2023-....
23.
World Health Organization. Regional Office for the Eastern Mediterranean. Young people and tobacco use https://apps.who.int/iris/bits... (access: 2023.08.28).
24.
World Health Organization. WHO report on the global tobacco epidemic, 2017: monitoring tobacco use and prevention policies https://apps.who.int/iris/hand... (access: 2023.08.28).
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.