Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Association between family meals vs. diet quality and leisure activities of young rural residents
1
Institute of Human Nutrition Sciences, University of Life Sciences, SGGW-WULS, Warsaw, Poland
2
Polish Federation of Food Industry Union of Employers
Corresponding author
Marta Sajdakowska
Institute of Human Nutrition Sciences, Warsaw University of Life Sciences, SGGW-WULS, Nowoursynowska Street 159C, 02-787, Warszawa, Poland
Institute of Human Nutrition Sciences, Warsaw University of Life Sciences, SGGW-WULS, Nowoursynowska Street 159C, 02-787, Warszawa, Poland
Ann Agric Environ Med. 2023;30(4):685-692
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Research is required to better understand the variables related to the frequency and cohesiveness of family meals. The aim of the study was to determine the association of eating meals with the family with other types of eating behaviours, sedentary behaviours, and physical activity based on a self-reported questionnaire carried out on a sample of the Polish population of rural adolescents.
Material and methods:
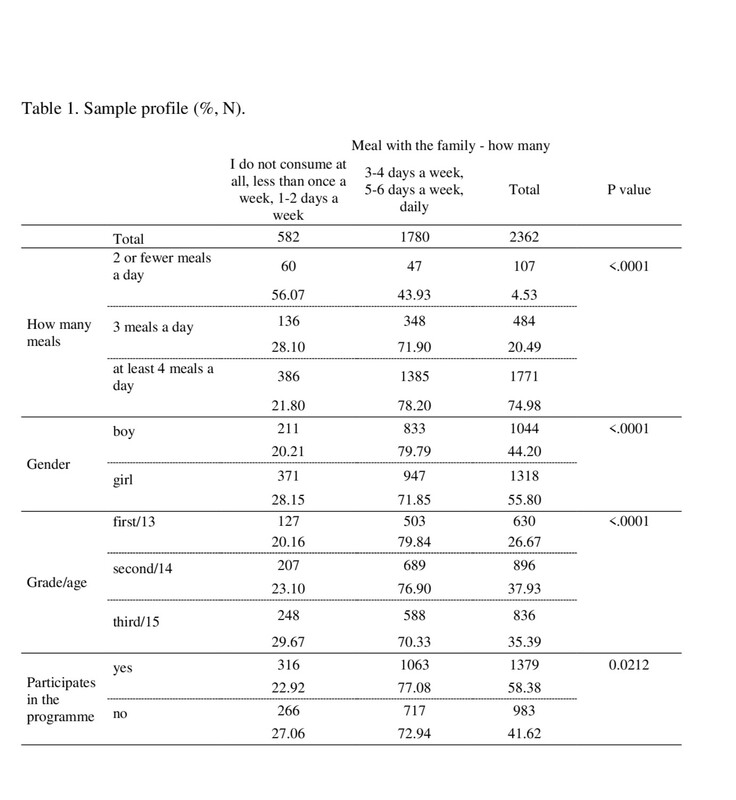
The analysis was performed among adolescents living in rural areas who participated in a survey conducted within the framework of the ‘Trzymaj formę!’ (‘Keep Fit!’) programme on eating behaviours. The survey questionnaire was completed by 2,362 teenagers aged 13–16.
Results:
Generally, positive evidence in terms of eating behaviours resulted in a higher likelihood of eating meals together with family. Not eating breakfast resulted in a decreased chance of eating meals together with the family. The results show that with regard to the use of computers at weekends, in the case of using them for a rather limited time, i.e. from 0.5–2 hours a day, there was a greater chance of having meals together.
Conclusions:
The results confirm the role of educational programmes in increasing the chances of sharing meals with the family, which confirms the validity of conducting this type of education among children and adolescents. It can be also concluded that the more positive eating behaviours of the surveyed junior high students aged 13–16, consisting in more frequent consumption of fruit, greater consumption of cereal products, and more water consumed during the day, is proof of the positive influence of parents on the nutritional behaviour of their children. This is consistent with good intra-family relationships reflected in a greater tendency to spend time together over a family meal.
Research is required to better understand the variables related to the frequency and cohesiveness of family meals. The aim of the study was to determine the association of eating meals with the family with other types of eating behaviours, sedentary behaviours, and physical activity based on a self-reported questionnaire carried out on a sample of the Polish population of rural adolescents.
Material and methods:
The analysis was performed among adolescents living in rural areas who participated in a survey conducted within the framework of the ‘Trzymaj formę!’ (‘Keep Fit!’) programme on eating behaviours. The survey questionnaire was completed by 2,362 teenagers aged 13–16.
Results:
Generally, positive evidence in terms of eating behaviours resulted in a higher likelihood of eating meals together with family. Not eating breakfast resulted in a decreased chance of eating meals together with the family. The results show that with regard to the use of computers at weekends, in the case of using them for a rather limited time, i.e. from 0.5–2 hours a day, there was a greater chance of having meals together.
Conclusions:
The results confirm the role of educational programmes in increasing the chances of sharing meals with the family, which confirms the validity of conducting this type of education among children and adolescents. It can be also concluded that the more positive eating behaviours of the surveyed junior high students aged 13–16, consisting in more frequent consumption of fruit, greater consumption of cereal products, and more water consumed during the day, is proof of the positive influence of parents on the nutritional behaviour of their children. This is consistent with good intra-family relationships reflected in a greater tendency to spend time together over a family meal.
REFERENCES (60)
1.
Mokdad AH, Forouzanfar MH, Daoud F, et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 2016;387(10036):2383–2401. doi:10.1016/S0140-6736(16)00648-6.
2.
Global Nutrition Monitoring Framework: operational guidance for tracking progress in meeting targets for 2025. Global Nutrition Monitoring Framework Targets for 2025. AEMIA. 2017. Accessed August 19, 2022. http://apps.who.int/iris/bitst... 666C3EE9F022BFD99D86?sequence=1.
3.
Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood andadult obesity in the United States 2011–2012. J Am Med Assoc JAMA. 2014;311(8):806–814. doi:10.1001/jama.2014.732.
4.
Suder A, Gomula A, Koziel S. Central overweight and obesity in Polish schoolchildren aged 7–18 years: secular changes of waist circumference between 1966 and 2012. Eur J Pediatr. 2017;176(7):909–916. doi:10.1007/ s00431-017-2938-4.
5.
Kowalkowska J, Wadolowska L, Wuenstel JW, et al. Socioeconomic Status and Overweight Prevalence in Polish Adolescents: The Impact of Single Factors and a Complex Index of Socioeconomic Status in Respect to Age and Sex. Iran J Public Health. 2014;43(7):913–25.
6.
Wadolowska L, Kowalkowska J, Czarnocinska J, et al. Comparing dietary patterns derived by two methods and their associations with obesity in Polish girls aged 13–21 years: The cross-sectional GEBaHealth study. Perspect Public Health. 2017;137(3):182–189. doi:10.1177/1757913916679859.
7.
Faienza MF, Wang DQH, Frühbeck G, et al. The dangerous link between childhood and adulthood predictors of obesity and metabolic syndrome. Intern Emerg Med. 2016;11(2):175–182. doi:10.1007/s11739-015-1382-6.
8.
Chaput JP, Pérusse L, Després JP, et al. Findings from the Quebec Family Study on the Etiology of Obesity: Genetics and Environmental Highlights. Curr Obes Rep. 2014;3(1):54–66. doi:10.1007/s13679-013- 0086-3.
9.
Serra-Majem L, Bautista-Castaño I. Etiology of obesity: two “key issues” and other emerging factors. Nutr Hosp. 2013;28(5):32–43.
10.
Wadolowska L, Kowalkowska J, Lonnie M, et al. Associations between physical activity patterns and dietary patterns in a representative sample of Polish girls aged 13–21 years: a cross-sectional study (GEBaHealth Project). BMC Public Health. 2016;16(1):1–14. doi:10.1186/s12889- 016-3367-4.
11.
European Food and Nutrition Action Plan 2015–2020. Regional Committee for Europe REGIONAL 64th Session.; 2014. Accessed August 19, 2022. http://www.euro.who.int/__ data/assets/pdf_ file/0008/253727/64wd14e_FoodNutAP_140426.pdf.
12.
Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. doi:10.1111/j.1753-4887.2011.00456.x.
13.
Xu H, Wen LM, Rissel C. Associations of parental influences with physical activity and screen time among young children: A systematic review. J Obes. 2015;2015. doi:10.1155/2015/546925.
14.
Dumith SC, Gigante DP, Domingues MR, et al. Physical activity change during adolescence: A systematic review and a pooled analysis. Int J Epidemiol. 2011;40(3):685–698. doi:10.1093/ije/dyq272.
15.
Loyen A, van Hecke L, Verloigne M, et al. Variation in population levels of physical activity in European adults according to cross-European studies: A systematic literature review within DEDIPAC. Int J Behav Nutr Phys Act. 2016;13(1):1–18. doi:10.1186/s12966-016-0398-2.
16.
Spronk I, Kullen C, Burdon C, et al. Relationship between nutrition knowledge and dietary intake. Br J Nutr. 2014;111(10):1713–1726. doi:10.1017/S0007114514000087.
17.
Baxter SD. Cognitive processes in children’s dietary recalls: Insight from methodological studies. Eur J Clin Nutr. 2009;63:S19-S32. doi:10.1038/ejcn.2008.61.
18.
Besler HT, Meseri R, Küçükerdönmez Ö, et al. Implementation of a “Balanced Nutrition Education Program” among primary school children in Turkey. Nutrition. 2018;55–56:S18-S21. doi:10.1016/j. nut.2018.07.011.
19.
Todendi PF, Martínez JA, Reuter CP, et al. Biochemical profile, eating habits, and telomere length among Brazilian children and adolescents. Nutrition. 2020;71. doi:10.1016/j.nut.2019.110645.
20.
Guzek D, Głąbska D, Lange E, et al. A polish study on the influence of food neophobia in children (10–12 years old) on the intake of vegetables and fruits. Nutrients. 2017;9(6):563. doi:10.3390/nu9060563.
21.
Guzek D, Głąbska D, Groele B, et al. Role of fruit and vegetables for the mental health of children: a systematic review. Rocz Panstw Zakl Hig. 2020;71(1):5–13. doi:10.32394/rpzh.2019.0096.
22.
de Vet E, Stok FM, de Wit JBF, et al. The habitual nature of unhealthy snacking: How powerful are habits in adolescence? Appetite. 2015;95:182–187. doi:10.1016/j.appet.2015.07.010.
23.
Dęcyk-Chęcel A. Children’s and adolescents’ eating habits. Probl Hig Epidemiol. 2017;98(2):103–109. www.phie.pl.
24.
Sygit KM, Sygit M, Wojtyła-Buciora P, et al. Environmental variations of nutritional mistakes among Polish school-age adolescents from urban and rural areas. Ann Agr Env Med. 2019;26(3):483–488.
25.
Story M, Neumar-Sztainer D, French S. Individual and environmental influences on adolescent eating behaviors. J Am Diet Assoc. 2002;102(3):S40-S51.
26.
Louzada ML da C, Baraldi LG, Steele EM, et al. Consumption of ultraprocessed foods and obesity in Brazilian adolescents and adults. Prev Med. 2015;81:9–15. doi:10.1016/j.ypmed.2015.07.018.
27.
de Andrade Previato HDR, Behrens JH. Taste-related factors and food neophobia: Are they associated with nutritional status and teenagers’ food choices? Nutrition. 2017;42:23–29. doi:10.1016/j.nut.2017.05.006.
28.
Rathi N, Riddell L, Worsley A. What influences urban Indian secondary school students’ food consumption? – A qualitative study. Appetite. 2016;105:790–797. doi:10.1016/j.appet.2016.07.018.
29.
Rosen LD, Lim AF, Felt J, et al. Media and technology use predicts ill-being among children, preteens and teenagers independent of the negative health impacts of exercise and eating habits. Comput Human Behav. 2014;35:364–375. doi:10.1016/j.chb.2014.01.036.
30.
Doggui R, Ward S, Johnson C, et al. Trajectories of beverage consumption during adolescence. Appetite. 2022;175:106092. doi:10.1016/j.appet.2022.106092.
31.
Corazza I, Pennucci F, de Rosis S. Promoting healthy eating habits among youth according to their preferences: Indications from a discrete choice experiment in Tuscany. Health Policy (New York). 2021;125(7):947–955. doi:10.1016/j.healthpol.2021.03.014.
32.
Jezewska-Zychowicz M, Gębski J, Guzek D, et al. The associations between dietary patterns and sedentary behaviors in polish adults (Lifestyle study). Nutrients. 2018;10(8):1–16. doi:10.3390/nu10081004.
33.
Shqair AQ, Pauli LA, Costa VPP, et al. Screen time, dietary patterns and intake of potentially cariogenic food in children: A systematic review. J Dent. 2019;86:17–26. doi:10.1016/j.jdent.2019.06.004.
34.
Górnicka M, Hamulka J, Wadolowska L, et al. Activity–inactivity patterns, screen time, and physical activity: The association with overweight, central obesity and muscle strength in Polish teenagers. report from the ABC of healthy eating study. Int J Environ Res Public Health. 2020;17(21):1–21. doi:10.3390/ijerph17217842.
35.
Navidad L, Padial-Ruz R, González MC. Nutrition, physical activity, and new technology programs on obesity prevention in primary education: A systematic review. Int J Environ Res Public Health. 2021;18(19):101187. doi:10.3390/ijerph181910187.
36.
Neves FS, Fontes VS, Nogueira MC, et al. Eating contexts at breakfast, lunch, and dinner: Associations with ultra-processed foods consumption and overweight in Brazilian adolescents (EVA-JF Study). Appetite. 2022;168: 105787. doi:10.1016/j.appet.2021.105787.
37.
Hamulka J, Wadolowska L, Hoffmann M, et al. Effect of an education program on nutrition knowledge, attitudes toward nutrition, diet quality, lifestyle, and body composition in polish teenagers. The ABC of healthy eating project: Design, protocol, and methodology. Nutrients. 2018;10(10):1439. doi:10.3390/nu10101439.
38.
Wadolowska L, Hamulka J, Kowalkowska J, et al. Prudent-active and fast-food-sedentary dietary-lifestyle patterns: The association with adiposity, nutrition knowledge and sociodemographic factors in Polish teenagers—The ABC of healthy eating project. Nutrients. 2018;10(12):1988. doi:10.3390/nu10121988.
39.
Wadolowska L, Hamulka J, Kowalkowska J, et al. Changes in sedentary and active lifestyle, diet quality and body composition nine months after an education program in Polish students aged 11–12 years: Report from the ABC of healthy eating study. Nutrients. 2019;11(2):331. doi:10.3390/ nu11020331.
40.
Kremer-Sadlik T, Morgenstern A. The reflective eater: Socializing French children to eating fruits and vegetables. Appetite. 2022;172:105954. doi:10.1016/j.appet.2022.105954.
41.
Schnettler B, Grunert KG, Lobos G, et al. A latent class analysis of family eating habits in families with adolescents. Appetite. 2018;129:37–48. doi:10.1016/j.appet.2018.06.035.
42.
Larson N, MacLehose R, Fulkerson JA, et al. Eating Breakfast and Dinner Together as a Family: Associations with Sociodemographic Characteristics and Implications for Diet Quality and Weight Status. J Acad Nutr Diet. 2013;113(12):1601–1609. doi:10.1016/j.jand.2013.08.011.
43.
Gutkowska K, Gantner A, Tomaszewska-Pielacha M. Znaczenie Ogólnopolskiego Programu Edukacyjnego “Trzymaj Formę!” W Profilaktyce Nadwagi i Otyłości Wśród Dzieci i Młodzieży. I. (Kiryjow J, ed.). Wydawnictwo SGGW; 2019.
44.
Gantner A. Znaczenie Ogólnopolskiego Programu Edukacyjnego “Trzymaj Formę!” W Profilaktyce Nadwagi i Otyłości Wśród Dzieci i Młodzieży. Praca doktorska/Doctoral thesis. Instytut Nauk o Żywieniu Człowieka; 2019.
45.
Oświata i wychowanie w roku szkolnym 2015/2016. Education in 2015/2016 School Year. Informacje i Opracowania Statystyczne GUS, Warsaw 2016.
46.
Wolnicka K. Wspólne posiłki w domu zapobiegają nadwadze i otyłości u dzieci i młodzieży. Accessed August 25, 2022. https://ncez.pzh.gov. pl/dzieci-i-mlodziez/wspolne-posilki-w-domu-zapobiegaja-nadwadzei- otylosci-u-dzieci-i-mlodziezy/.
47.
Woodruff SJ, Hanning RM. Associations Between Family Dinner Frequency and Specific Food Behaviors Among Grade Six, Seven, and Eight Students from Ontario and Nova Scotia. J Adolesc Health. 2009;44(5):431–436. doi:10.1016/j.jadohealth.2008.10.141.
48.
Mahmood L, González-Gil EM, Schwarz P, et al. Frequency of family meals and food consumption in families at high risk of type 2 diabetes: the Feel4Diabetes-study. Eur J Pediatr. 2022;181(6):2523–2534. doi:10.1007/s00431-022-04445-4.
49.
Wang X, Hu Y, Qin LQ, et al. Meal frequency and incidence of type 2 diabetes: A prospective study. Br J Nutr. 2021;128(2):1–6. doi:10.1017/ S0007114521003226.
50.
Agathao BT, Cunha DB, Sichieri R, et al. The role of family meal frequency in common mental disorders in children and adolescents over eight months of follow-up. PLoS One. 2021;16(2): e0243793. doi:10.1371/ journal.pone.0243793.
51.
Welsh EM, French SA, Wall M. Examining the Relationship Between Family Meal Frequency and Individual Dietary Intake: Does Family Cohesion Play a Role? J Nutr Educ Behav. 2011;43(4):229–235. doi:10.1016/j.jneb.2010.03.009.
52.
Kameyama N, Morimoto Y, Hashimoto A, et al. The relationship between family meals and mental health problems in japanese elementary school children: A cross-sectional study. Int J Environ Res Public Health. 2021;18(17):9281. doi:10.3390/ijerph18179281.
53.
Tambalis KD, Panagiotakos DB, Psarra G, et al. Breakfast skipping in Greek schoolchildren connected to an unhealthy lifestyle profile. Results from the National Action for Children’s Health program. Nutr Diet. 2019;76(3):328–335. doi:10.1111/1747-0080.12522.
54.
Wolnicka K, Taraszewska AM, Jaczewska-Schuetz J, et al. Factors within the family environment such as parents’ dietary habits and fruit and vegetable availability have the greatest influence on fruit and vegetable consumption by Polish children. Public Health Nutr. 2015;18(15):2705–2711.
55.
Caldwell AR, Terhorst L, Skidmore ER, et al. Is frequency of family meals associated with fruit and vegetable intake among preschoolers? A logistic regression analysis. J Hum Nutr Diet. 2018;31(4):505–512. doi:10.1111/jhn.12531.
56.
Goldfield GS, Cameron JD, Murray M, et al. Screen time is independently associated with health-related quality of life in overweight and obese adolescents. Acta Paediatr. 2015;104(10):e448-e454. doi:10.1111/ apa.13073.
57.
Sánchez-Miguel PA, Sevil-Serrano J, Sánchez-Oliva D, et al. School and non-school day screen time profiles and their differences in health and educational indicators in adolescents. Scand J Med Sci Sports. 2022;32(11):1668–1681. doi:10.1111/sms.14214.
58.
Fletcher E, Leech R, Mcnaughton SA, et al. Is the relationship between sedentary behaviour and cardiometabolic health in adolescents independent of dietary intake? A systematic review. Obes Rev. 2015;16(9):795–805. doi:10.1111/obr.12302.
59.
Martin KB, Bednarz JM, Aromataris EC. Interventions to control children’s screen use and their effect on sleep: A systematic review and meta-analysis. J Sleep Res. 2021;30(3):13130. doi:10.1111/jsr.13130.
60.
Harrex HAL, Skeaff SA, Black KE, et al. Sleep timing is associated with diet and physical activity levels in 9–11-year-old children from Dunedin, New Zealand: the PEDALS study. J Sleep Res. 2018;27(4):12634. doi:10.1111/jsr.12634.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.