Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Selected routine laboratory tests in the clinical assessment of patients with obstructive sleep apnea
1
Chair and Department of Internal Medicine, Medical University, Lublin, Poland
2
Individual Specialist Medical Practice, Lublin, Poland
3
Institute of Rural Health, Lublin, Poland
4
Collegium Medicum, Jan Kochanowski University, Kielce, Poland
5
I Chair and Department of Oncological Gynaecology and Gynaecology, Independent Public Hospital No 1, Lublin, Poland
Corresponding author
Klaudia Brożyna-Tkaczyk
Chair and Department of Internal Medicine, Medical University of Lublin, Staszica 16 St., 20-081, Lublin, Poland
Chair and Department of Internal Medicine, Medical University of Lublin, Staszica 16 St., 20-081, Lublin, Poland
Ann Agric Environ Med. 2023;30(4):737-742
KEYWORDS
C-reactive proteinobstructive sleep apneafasting glucoselipid profilehaematological parametersNT-proBNPhypoxia
TOPICS
ABSTRACT
Introduction:
Obstructive sleep apnea (OSA) is a chronic disease characterized by repetitive complete or partial occlusion of the upper airways during sleep with respiratory muscle effort, which leads to consecutive apneas and hypopneas. Obstruction of the upper airways during sleep leads to repetitive episodes of disrupted airflow and consequent changes in blood oxygenation, resulting in hypoxaemia and hypercapnia. Intermittent hypoxaemia induces the production of pro-inflammatory factors and promotes metabolic dysregulation and platelet aggregation.
Objective:
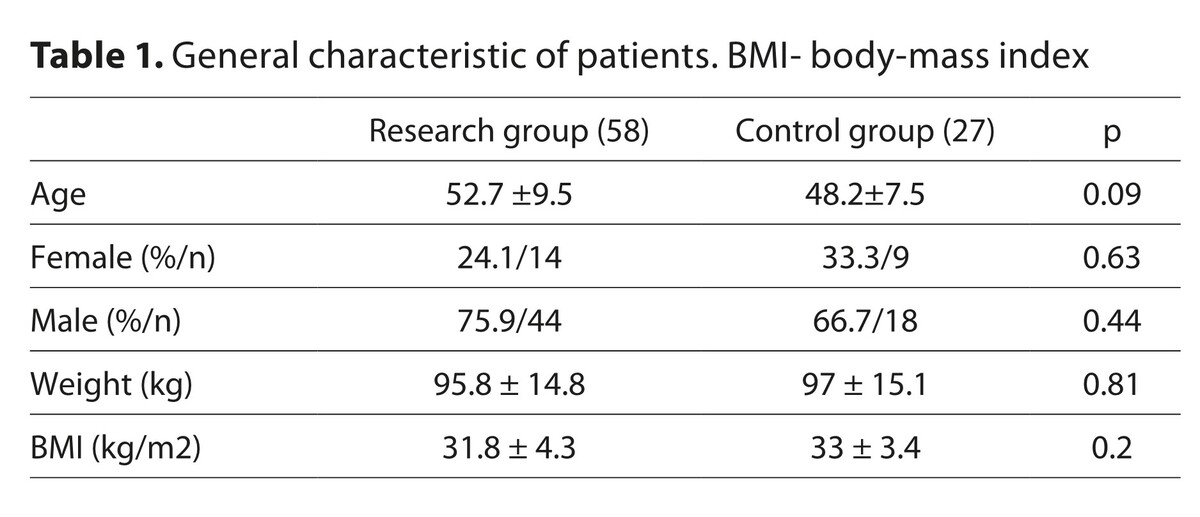
The main aim of this study was to determine differences, if any, in selected standard parameters in routine laboratory tests often used in GP practice between patients with obstructive sleep apnea, without comorbidities, and a well-defined control group with the absence of this syndrome proven in polygraphic examination.
Material and methods:
Of the 192 clinically assessed persons with suspected OSA and admitted to the Internal Medicine Department in Lublin, 85 were qualified for the study after application of exclusion criteria. Demographic and health behaviour-related data, medical history regarding sleep habits and cardiovascular disease, were collected from each patient.
Results:
Apart from significantly higher MCV and MCH among the cpontrol group, no significant differences were found between patients with obstructive sleep apnea and the control group.
Conclusions:
The results can be useful for the holistic assessment of the health status of patients with newly-diagnosed OSA.
Obstructive sleep apnea (OSA) is a chronic disease characterized by repetitive complete or partial occlusion of the upper airways during sleep with respiratory muscle effort, which leads to consecutive apneas and hypopneas. Obstruction of the upper airways during sleep leads to repetitive episodes of disrupted airflow and consequent changes in blood oxygenation, resulting in hypoxaemia and hypercapnia. Intermittent hypoxaemia induces the production of pro-inflammatory factors and promotes metabolic dysregulation and platelet aggregation.
Objective:
The main aim of this study was to determine differences, if any, in selected standard parameters in routine laboratory tests often used in GP practice between patients with obstructive sleep apnea, without comorbidities, and a well-defined control group with the absence of this syndrome proven in polygraphic examination.
Material and methods:
Of the 192 clinically assessed persons with suspected OSA and admitted to the Internal Medicine Department in Lublin, 85 were qualified for the study after application of exclusion criteria. Demographic and health behaviour-related data, medical history regarding sleep habits and cardiovascular disease, were collected from each patient.
Results:
Apart from significantly higher MCV and MCH among the cpontrol group, no significant differences were found between patients with obstructive sleep apnea and the control group.
Conclusions:
The results can be useful for the holistic assessment of the health status of patients with newly-diagnosed OSA.
REFERENCES (73)
1.
Wang Y, Xu H, Qian Y, et al. Patients with Obstructive Sleep Apnea Display Decreased Flow-Mediated Dilatation: Evidence from a Meta-Analysis. Med Sci Monit. 2017;23:1069–1082. https://doi.org/10.12659/MSM.8....
2.
Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the Global Prevalence and Burden of Obstructive Sleep Apnoea: A Literature-Based Analysis. Lancet Respir Med. 2019;7(8):687–698. https://doi.org/10.1016/S2213-....
3.
Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi:10.1093/aje/kws342.
4.
Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217–1239. doi:10.1164/rccm.2109080.
5.
Milicic Ivanovski D, Milicic Stanic B, Kopitovic I. Comorbidity Profile and Predictors of Obstructive Sleep Apnea Severity and Mortality in Non-Obese Obstructive Sleep Apnea Patients. Medicina (Kaunas). 2023;59(5):873. doi:10.3390/medicina59050873.
6.
Eisele HJ, Markart P, Schulz R. Obstructive Sleep Apnea, Oxidative Stress, and Cardiovascular Disease: Evidence from Human Studies. Oxid Med Cell Longev. 2015;2015:608438. doi:10.1155/2015/608438.
7.
Li Y, Wang Y. Obstructive Sleep Apnea-hypopnea Syndrome as a Novel Potential Risk for Aging. Aging Dis. 2021;12(2):586–596. doi:10.14336/AD.2020.0723.
8.
Güneş ZY, Günaydin FM. The relationship between the systemic immune-inflammation index and obstructive sleep apnea. Sleep Breath. 2023;10.1007/s11325-023-02913-1. doi:10.1007/s11325-023-02913-1.
9.
Wang L, Fang X, Xu C, et al. Epworth sleepiness scale is associated with hypothyroidism in male patients with obstructive sleep apnea. Front Endocrinol (Lausanne). 2022;13:1010646. doi:10.3389/fendo.2022.1010646.
10.
Semelka M, Wilson J, Floyd R. Diagnosis and Treatment of Obstructive Sleep Apnea in Adults. Am Fam Physician. 2016;94(5):355–360.
11.
Andrade L, Paiva T. Ambulatory Versus Laboratory Polysomnography in Obstructive Sleep Apnea: Comparative Assessment of Quality, Clinical Efficacy, Treatment Compliance, and Quality of Life. J Clin Sleep Med. 2018;14(8):1323–1331. doi:10.5664/jcsm.7264.
12.
Yamauchi M, Nakano H, Maekawa J, et al. Oxidative stress in obstructive sleep apnea. Chest. 2005;127(5):1674–1679. doi:10.1378/chest.127.5.1674.
13.
Eisele HJ, Markart P, Schulz R. Obstructive Sleep Apnea, Oxidative Stress, and Cardiovascular Disease: Evidence from Human Studies. Oxid Med Cell Longev. 2015;2015:60843.
14.
Antonescu-Turcu A, Parthasarathy S. CPAP and bi-level PAP therapy: new and established roles. Respir Care. 2010;55(9):1216–1229.
15.
Fan Z, Lu X, Long H, et al. The association of hemocyte profile and obstructive sleep apnea. J Clin Lab Anal. 2019;33(2):e22680. doi:10.1002/jcla.22680.
16.
Bülbül Y, Aydin Özgür E, Örem A. Platelet indices in obstructive sleep apnea: the role of mean platelet volume, platelet distribution widht and plateletcrit. Obstrüktif uyku apnesinde trombosit indisleri: Ortalama trombosit hacmi, trombosit dagilim genişligi ve plateletcritin yeri. Tuberk Toraks. 2016;64(3):206–210. doi:10.5578/tt.29170.
17.
Kivanc T, Kulaksizoglu S, Lakadamyali H, et al. Importance of laboratory parameters in patients with obstructive sleep apnea and their relationship with cardiovascular diseases. J Clin Lab Anal. 2018;32(1):e22199. doi:10.1002/jcla.22199.
18.
Wu M, Zhou L, Zhu D, et al. Hematological indices as simple, inexpensive and practical severity markers of obstructive sleep apnea syndrome: a meta-analysis. J Thorac Dis. 2018;10(12):6509–6521. doi:10.21037/jtd.2018.10.105.
19.
Cummins E, Waseem R, Piyasena D, et al. Can the complete blood count be used as a reliable screening tool for obstructive sleep apnea? Sleep Breath. 2022;26(2):613–620. doi:10.1007/s11325-021-02383-3.
20.
Yasuoka Y, Izumi Y, Sands JM, et al. Progress in the Detection of Erythropoietin in Blood, Urine, and Tissue. Molecules. 2023;28(11):4446. https://doi.org/10.3390/molecu....
21.
Di Lorenzo B, Pau MC, Zinellu E, et al. Association between Red Blood Cell Distribution Width and Obstructive Sleep Apnea Syndrome: A Systematic Review and Meta-Analysis. J Clin Med. 2023;12(9):3302. doi:10.3390/jcm12093302.
22.
Morell-Garcia D, Toledo-Pons N, Sanchis P, et al. Red cell distribution width: a new tool for the severity prediction of sleep apnoea syndrome in children. ERJ Open Res. 2020;6(4):00278–2019. doi:10.1183/23120541.00278-2019.
23.
Nagao T, Hirokawa M. Diagnosis and treatment of macrocytic anemias in adults. J Gen Fam Med. 2017;18(5):200–204. doi:10.1002/jgf2.31.
24.
Tonelli M, Sacks F, Arnold M, et al. Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation. 2008;117(2):163–68.
25.
Gunbatar H, Sertogullarindan B, Ekin S, et al. The correlation between red blood cell distribution width levels with the severity of obstructive sleep apnea and carotid intima media thickness. Med Sci Monit. 2014;20:2199–2204. doi:10.12659/MSM.891001.
26.
Varol E, Ozturk O, Gonca T, et al. Mean platelet volume is increased in patients with severe obstructive sleep apnea. Scand J Clin Lab Invest. 2010;70(7):497–502. doi:10.3109/00365513.2010.520733.
27.
Hui DS, Ko FW, Fok JP, et al. The effects of nasal continuous positive airway pressure on platelet activation in obstructive sleep apnea syndrome. Chest. 2004;125(5):1768–1775. doi:10.1378/chest.125.5.1768.
28.
Nkambule BB, Mxinwa V, Nyambuya TM, et al. The mean platelet volume and atherosclerotic cardiovascular-risk factors in adults with obesity: a systematic review and meta-analysis of observational studies. BMC Nutr. 2022;8(1):47. doi:10.1186/s40795-022-00541-8.
29.
Nena E, Papanas N, Steiropoulos P, et al. Mean Platelet Volume and Platelet Distribution Width in non-diabetic subjects with obstructive sleep apnoea syndrome: new indices of severity? Platelets. 2012;23(6):447–454. doi:10.3109/09537104.2011.632031.
30.
Beyan C, Kaptan K, Ifran A. Platelet count, mean platelet volume, platelet distribution width, and plateletcrit do not correlate with optical platelet aggregation responses in healthy volunteers. J Thromb Thrombolysis. 2006;22(3):161–164. doi:10.1007/s11239-006-9014-7.
31.
Volná J, Kemlink D, Kalousová M, et al. Biochemical oxidative stress-related markers in patients with obstructive sleep apnea. Med Sci Monit. 2011;17(9):CR491-CR497. doi:10.12659/msm.881935.
32.
Qiao YX, Xiao Y. Asthma and Obstructive Sleep Apnea. Chin Med J (Engl). 2015;128(20):2798–2804. doi:10.4103/0366-6999.167361.
33.
Cao Y, Wu S, Zhang L, et al. Association of allergic rhinitis with obstructive sleep apnea: A meta-analysis. Medicine (Baltimore). 2018;97(51):e13783. doi:10.1097/MD.0000000000013783.
34.
Andersen CJ, Vance TM. Gender Dictates the Relationship between Serum Lipids and Leukocyte Counts in the National Health and Nutrition Examination Survey 1999–2004. J Clin Med. 2019;8(3):365. doi:10.3390/jcm8030365.
35.
Franco-Peláez JA, Martín-Reyes R, Pello-Lázaro AM, et al. Monocyte Chemoattractant Protein-1 Is an Independent Predictor of Coronary Artery Ectasia in Patients with Acute Coronary Syndrome. J Clin Med. 2020;9(9):3037.
36.
Adedayo AM, Olafiranye O, Smith D, et al. Obstructive sleep apnea and dyslipidemia: evidence and underlying mechanism. Sleep Breath. 2014;18(1):13–18. doi:10.1007/s11325-012-0760-9.
37.
Chen B, Guo M, Peker Y, et al. Effect of Continuous Positive Airway Pressure on Lipid Profiles in Obstructive Sleep Apnea: A Meta-Analysis. J Clin Med. 2022;11(3):596.
38.
Kollar B, Siarnik P, Hluchanova A, et al. The impact of sleep apnea syndrome on the altered lipid metabolism and the redox balance. Lipids Health Dis. 2021;20(1):175. doi:10.1186/s12944-021-01604-8.
39.
Tan KC, Chow WS, Lam JC, et al. HDL dysfunction in obstructive sleep apnea. Atherosclerosis. 2006;184(2):377–382. doi:10.1016/j.atherosclerosis.2005.04.024.
40.
Akbarian S, Ghahjaverestan NM, Yadollahi A, et al. Noncontact Sleep Monitoring With Infrared Video Data to Estimate Sleep Apnea Severity and Distinguish Between Positional and Nonpositional Sleep Apnea: Model Development and Experimental Validation. J Med Internet Res. 2021;23(11):e26524. doi:10.2196/26524.
41.
Kim NH, Cho NH, Yun CH, et al. Association of obstructive sleep apnea and glucose metabolism in subjects with or without obesity. Diabetes Care. 2013;36(12):3909–3915. doi:10.2337/dc13-0375.
42.
Sajkov D, Mupunga B, Bowden JJ, et al. Narrative Review: Obesity, Type 2 DM and Obstructive Sleep Apnoea—Common Bedfellows. Diabetology. 2022; 3(3):447–459. https://doi.org/10.3390/diabet....
43.
Zhou M, Guo B, Wang Y, et al. The Association Between Obstructive Sleep Apnea and Carotid Intima–Media Thickness: A Systematic Review and Meta-Analysis. Angiology. 2017;68(7):575–583. doi:10.1177/0003319716665985.
44.
Vgontzas AN, Zoumakis E, Bixler EO, et al. Adverse effects of modest sleep restriction on sleepiness, performance, and inflammatory cytokines. J Clin Endocrinol Metab. 2004;89(5):2119–2126. doi:10.1210/jc.2003-031562.
45.
Bilbao AV, Goldschmied J, Jang A, et al. A preliminary study on the relationship between sleep, depression and cardiovascular dysfunction in a 4 sample population. Int J Cardiol Heart Vasc. 2021;35:100814.
46.
Orrù G, Storari M, Scano A, et al. Obstructive Sleep Apnea, oxidative stress, inflammation and endothelial dysfunction-An overview of predictive laboratory biomarkers. Eur Rev Med Pharmacol Sci. 2020;24(12):6939–6948. doi:10.26355/eurrev_202006_21685.
47.
Yi M, Zhao W, Fei Q, et al. Causal analysis between altered levels of interleukins and obstructive sleep apnea. Front Immunol. 2022;13:888644. doi:10.3389/fimmu.2022.888644.
48.
Zaidi H, Aksnes T, Åkra S, et al. Abdominal Adipose Tissue Associates With Adiponectin and TNFα in Middle-Aged Healthy Men. Front Endocrinol (Lausanne). 2022;13:874977.
49.
Zeng Y, He X, Jiang W, et al. Ten Representative Saponins on Tissue Factor Expression in Human Monocytes: Structure–Activity Relationships and Molecular Docking. Nat Prod Commun. 2020;15(3). doi:10.1177/1934578X20913684.
50.
Mastino P, Rosati D, de Soccio G, et al. Oxidative Stress in Obstructive Sleep Apnea Syndrome: Putative Pathways to Hearing System Impairment. Antioxidants. 2023;12(7):1430. https://doi.org/10.3390/antiox....
51.
Kheirandish-Gozal L, Gozal D. Obstructive Sleep Apnea and Inflammation: Proof of Concept Based on Two Illustrative Cytokines. Inter J Molecular Sci. 2019;20(3):459. https://doi.org/10.3390/ijms20....
52.
Lima AM, Franco CM, Castro CM, et al. Contribuição da apnéia obstrutiva do sono para o estresse oxidativo da obesidade. Arq Bras Endocrinol Metabol. 2008;52(4):668–676. doi:10.1590/s0004-27302008000400013.
53.
Meszaros M, Bikov A. Obstructive Sleep Apnoea and Lipid Metabolism: The Summary of Evidence and Future Perspectives in the Pathophysiology of OSA-Associated Dyslipidaemia. Biomedicines. 2022;10(11):2754. https://doi.org/10.3390/biomed....
54.
Haemmerle G, Lass A, Zimmermann R, et al. Defective lipolysis and altered energy metabolism in mice lacking adipose triglyceride lipase. Science. 2006;312(5774):734–737. doi:10.1126/science.1123965.
55.
Wang H, Bell M, Sreenivasan U, et al. Unique regulation of adipose triglyceride lipase (ATGL) by perilipin 5, a lipid droplet-associated protein. J Biol Chem. 2011;286(18):15707–15715. doi:10.1074/jbc.M110.207779.
56.
Walther LM, Wirtz PH. Physiological reactivity to acute mental stress in essential hypertension-a systematic review. Front Cardiovasc Med. 2023;10:1215710. doi:10.3389/fcvm.2023.1215710.
57.
Vallat R, Shah VD, Redline S, Attia P, Walker MP. Broken sleep predicts hardened blood vessels. PLoS Biol. 2020;18(6):e3000726.
58.
Franck G, Mawson T, Sausen G, et al. Flow Perturbation Mediates Neutrophil Recruitment and Potentiates Endothelial Injury via TLR2 in Mice: Implications for Superficial Erosion. Circ Res. 2017;121(1):31–42. doi:10.1161/CIRCRESAHA.117.310694.
59.
Geovanini GR, Wang R, Weng J, et al. Elevations in neutrophils with obstructive sleep apnea: The Multi-Ethnic Study of Atherosclerosis (MESA). Int J Cardiol. 2018;257:318–323. doi:10.1016/j.ijcard.2017.10.121.
60.
Fan Z, Lu X, Long H, et al. The association of hemocyte profile and obstructive sleep apnea. J Clin Lab Anal. 2019;33(2):e2268.
61.
Shah AD, Denaxas S, Nicholas O, et al. Neutrophil Counts and Initial Presentation of 12 Cardiovascular Diseases: A CALIBER Cohort Study. J Am Coll Cardiol. 2017;69(9):1160–1169. doi:10.1016/j.jacc.2016.12.022.
62.
Farrell PC, Richards G. Recognition and treatment of sleep-disordered breathing: an important component of chronic disease management. J Transl Med. 2017;15(1):114. doi:10.1186/s12967-017-1211-y.
63.
Cakmak VA, Ozsu S, Gulsoy A, et al. The Significance of the Relative Lymphocyte Count as an Independent Predictor of Cardiovascular Disease in Patients with Obstructive Sleep Apnea Syndrome. Med Princ Pract. 2016;25(5):455–460. doi:10.1159/000447697.
64.
Finamore P, Scarlata S, Cardaci V, et al. Exhaled Breath Analysis in Obstructive Sleep Apnea Syndrome: A Review of the Literature. Medicina. 2019;55(9):538. https://doi.org/10.3390/medici....
65.
Song KH, Lee J, Jung HR, et al. Turning behaviors of T cells climbing up ramp-like structures are regulated by myosin light chain kinase activity and lamellipodia formation. Sci Rep. 2017;7(1):11533.
66.
Lintermans LL, Stegeman CA, Heeringa P, Abdulahad WH. T cells in vascular inflammatory diseases. Front Immunol. 2014;5:504.
67.
Sun X, Yu W, Wang M, et al. Association between rest-activity rhythm and cognitive function in the elderly: The U.S. National Health and Nutrition Examination Survey, 2011–2014. Front Endocrinol (Lausanne). 2023;14:1135085. doi:10.3389/fendo.2023.1135085.
68.
Tan HL, Gozal D, Samiei A, et al. T regulatory lymphocytes and endothelial function in pediatric obstructive sleep apnea. PLoS One. 2013;8(7):e69710. doi:10.1371/journal.pone.0069710.
69.
Baessler A, Nadeem R, Harvey M, et al. Treatment for sleep apnea by continuous positive airway pressure improves levels of inflammatory markers – a meta-analysis. J Inflamm (Lond). 2013;10:13.
70.
Abdul Razak MR, Chirakalwasan N. Obstructive sleep apnea and asthma. Asian Pac J Allergy Immunol. 2016;34(4):265–271. doi:10.12932/AP0828.
71.
Shi H, Huang T, Ma Y, et al. Sleep Duration and Snoring at Midlife in Relation to Healthy Aging in Women 70 Years of Age or Older. Nat Sci Sleep. 2021;13:411–422. doi:10.2147/NSS.S302452.
72.
Wang TY, Lo YL, Lin SM, et al. Obstructive sleep apnoea accelerates FEV1 decline in asthmatic patients. BMC Pulm Med. 2017;17(1):55. doi:10.1186/s12890-017-0398-2.
73.
Teodorescu M, Polomis DA, Gangnon RE, et al. Asthma Control and Its Relationship with Obstructive Sleep Apnea (OSA) in Older Adults. Sleep Disord. 2013;2013:251567. doi:10.1155/2013/251567.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.