Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Mental health status of frontline clinical nurses fighting the Omicron variant of COVID-19 – a cross-sectional survey in China
1
Department of Obstetrics, South China Hospital, Health Science Center, Shenzhen University, Shenzhen, Guangdong, China
2
School of Nursing, Health Science Centre, Shenzhen University, Shenzhen, Guangdong, China
3
School of Nursing, Southern Medical University, Guangzhou, Guangdong , China
Ann Agric Environ Med. 2022;29(3):375-382
HIGHLIGHTS
- *Ting Li and Xichenhui Qiu contributed equally for this manuscript
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
From March 2022, China has been in the rapid progressing stage of the Omicron outbreak. However, the mental status of clinical nurses against infection by the Omicron variant of COVID-19 has been not explored. Therefore, a nationwide online investigation with a larger sample size was conducted to explore the mental status of Chinese frontline clinical nurses, and its influencing factors using sound validated and reliable measurements.
Material and methods:
A cross-sectional study was conducted, and 1,204 clinical nurses fighting the Omicron outbreak were recruited across various provinces of China.
Results:
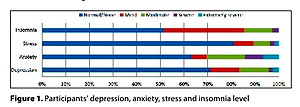
The mean age of the nurses was 30.43 (SD=6.59) years. The majority were female. The rates of these nurses with depression, anxiety, stress, and insomnia symptoms were 29.2%, 37.2%, 19.1%, and 48.8%, respectively. The variables of department, insomnia, fear with COVID-19, turnover intention, job burnout, work coping style, and public recognition of nursing, were significant factors influencing the mental status of clinical nurses.
Conclusions:
The Chinese clinical nurses fighting the Omicron variant of COVID-19 had a similar level of depression and anxiety, a higher level of insomnia, and a lower level of stress, in comparison with nurses globally who experienced the initial period of the pandemic. Targeted investigation and interventions are urgently needed for Chinese frontline clinical nurses with high levels of anxiety, depression and insomnia, who fought against infection by Omicron. Much more professional advocacy is strongly recommended during control of the pandemic and recovery to consolidate the role and influence of nurses. The contribution and visibility of nursing should be recognized not only by the medical professionals, but by the public in general.
From March 2022, China has been in the rapid progressing stage of the Omicron outbreak. However, the mental status of clinical nurses against infection by the Omicron variant of COVID-19 has been not explored. Therefore, a nationwide online investigation with a larger sample size was conducted to explore the mental status of Chinese frontline clinical nurses, and its influencing factors using sound validated and reliable measurements.
Material and methods:
A cross-sectional study was conducted, and 1,204 clinical nurses fighting the Omicron outbreak were recruited across various provinces of China.
Results:
The mean age of the nurses was 30.43 (SD=6.59) years. The majority were female. The rates of these nurses with depression, anxiety, stress, and insomnia symptoms were 29.2%, 37.2%, 19.1%, and 48.8%, respectively. The variables of department, insomnia, fear with COVID-19, turnover intention, job burnout, work coping style, and public recognition of nursing, were significant factors influencing the mental status of clinical nurses.
Conclusions:
The Chinese clinical nurses fighting the Omicron variant of COVID-19 had a similar level of depression and anxiety, a higher level of insomnia, and a lower level of stress, in comparison with nurses globally who experienced the initial period of the pandemic. Targeted investigation and interventions are urgently needed for Chinese frontline clinical nurses with high levels of anxiety, depression and insomnia, who fought against infection by Omicron. Much more professional advocacy is strongly recommended during control of the pandemic and recovery to consolidate the role and influence of nurses. The contribution and visibility of nursing should be recognized not only by the medical professionals, but by the public in general.
FUNDING
Xujuan Zheng was supported by the General Program of Stable Support Plan for Universities in Shenzhen City (Grant No. 20200804101756002); Xichenhui Qiu was supported by the Shenzhen Natural Science Fund (the Stable Support Plan Program), China (Grant No: 8940206-0221).
REFERENCES (43)
1.
World Health Organization. Tracking SARS-CoV-2 variants, 2022. https://www.who.int/en/ activities/tracking-SARS-CoV-2-variants/ (accessed: 16 May 2022 27).
2.
Gu H, Krishnan P, Ng DYM, et al. Probable Transmission of SARS-CoV-2 Omicron Variant in Quarantine Hotel, Hong Kong, China, November 2021. Emerg Infect Dis. 2022; 28(2):460–462. https:// doi.org/10.3201/eid2802.212422.
3.
Luo M, Liu Q, Wang J, Gong Z. From SARS to the Omicron variant of COVID-19: China’s policy adjustments and changes to prevent and control infectious diseases. Biosci Trends. 2022;15(6):418–423. https:// doi.org/10.5582/bst.2021.01535.
4.
China.org.cn. China’s control measures effective against Omicron variant: official, 2021. http://www.china.org.cn/china/... (accessed: 7 May, 2022).
5.
Lewis D. Will Omicron finally overpower China’s COVID defences? Nature. 2022; 604(7904):17–18. https:// doi.org/ 10.1038/d41586-022-00884-z. PMID: 35347306.
6.
Huang Y, Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: who will be the high-risk group? Psychol Health Med. 2021; 26(1): 23–34. https://doi.org/10.1080/135485....
7.
Lu W, Wang H, Lin Y, et al. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatr Res. 2020; 288: 112936. https://doi.org/10.1016/j.psyc....
8.
Maunder RG, Lancee WJ, Rourke S, et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med. 2004; 66(6): 938–942. https://doi.org/:10.1097/01.ps....
9.
Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020; 88: 901–907. https:// doi.org/10.1016/j.bbi.2020.05.026.
10.
Dziedzic B, Kobos E, Sienkiewicz Z, et al. Mental Health of Nurses during the Fourth Wave of the COVID-19 Pandemic in Poland. Int J Environ Res Public Health. 2022; 19: 1785. https:// doi.org/10.3390/ijerph19031785.
11.
Kim MY, Yang YY. Mental Health Status and Its Influencing Factors: T?h e Case of Nurses Working in COVID-19 Hospitals in South Korea. Int J Environ Res Public Health. 2021; 18: 6531. https://doi.org/10.3390/ijerph....
12.
Napoli G. Stress and depressive symptoms among Italian mental health nurses during the COVID-19 pandemic, a cross-sectional study. Arch Psychiatr Nurs. 2022; 36:41–47. https://doi.org/10.1016/j.apnu....
13.
Chui PL, Chong MC, Abdullah KL, et al. T?h e COVID-19 Global Pandemic and Its Impact on the Mental Health of Nurses in Malaysia. Healthcare 2021; 9: 1259. https://doi.org/10.3390/health....
14.
Crowe S, Howard AF, Vanderspank-Wright B, et al. T?h e effect of COVID-19 pandemic on the mental health of Canadian critical care nurses providing patient care during the early phase pandemic: A mixed method study. Intensive Crit Care Nurs. 2021; 63:102999. https://doi.org/10.1016/j.iccn....
15.
Ning X, Yu F, Huang Q, et al. T?h e mental health of neurological doctors and nurses in Hunan Province, China during the initial stages of the COVID-19 outbreak. BMC Psychiatry. 2020; 20(1):436. https://doi.org/10.1016/10.118....
16.
Shahrour G, Dardas LA. Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. J Nurs Manag. 2020; 28:1686–95. https://doi.org/10.1111/jonm.1....
17.
Hong S, Ai M, Xu XM, et al. Immediate psychological impact on nurses working at 42 government-designated hospitals during COVID-19 outbreak in China: A cross-sectional study. Nurs Outlook. 2021; 69:6–12. https://doi.org/10.1016/j.outl....
18.
Hu D, Kong Y, Li W, et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClin Med. 2020; 24: 100424. https://doi.org/10.1016/j.ecli....
19.
Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020; 3(3): e203976. https://doi.org/10.1001/jamane....
20.
Sampaio F, Sequeira C, Teixeira L. Nurses’ mental health during the covid-19 outbreak. J Occup Environ Med. 2020; 62(10):783–787. https://doi.org/10.1097/. JOM.0000000000001987.
21.
Varghese A, George G, Kondaguli SV, et al. Decline in the mental health of nurses across the globe during COVID-19: A systematic review and meta-analysis. J Glob Health. 2021; 11:05009. https://doi.org/10.7189/jogh.1....
22.
Wang K, Shi HS, Geng FL, et al. Cross-cultural validation of the Depression Anxiety Stress Scale-21 in China. Psychol Assess. 2016; 28(5):e88-e100. https://doi.org/10.1037/pas000.... E.
23.
Chan RC.K, Xu T, Huang J, et al. Extending the utility of the Depression Anxiety Stress scale by examining its psychometric properties in Chinese settings. Psychiatry Res. 2012; 200(2–3): 879–883. https://doi.org/10.1016/j.psyc....
24.
Morin CM, Belleville G, Bélanger L, et al. T?h e insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. SLEEP. 2011; 34(5):601–608. https://doi.org/10.1093/sleep/....
25.
Badiee Aval Baghyahi S, Torabi S, Gao Y, et al. Relaibility and validity of the Chinese translation of insomnia severity index (C-ISI) in Chinese patients with insomnia. Eur Psychiatry. 2011; 26(S2): 1556–1556. https://doi.org/10.1016/S0924-....
26.
Lin CY, Hou WL, Mamun MA, et al. Fear of COVID-19 Scale (FCV-19S) across countries: Measurement invariance issues. Nurs Open. 2021; 8(4):1892–1908. https://doi.org/10.1002/nop2.8....
27.
Chi X, Chen S, Chen Y, et al. Psychometric Evaluation of the Fear of COVID-19 Scale Among Chinese Population. Int J Ment Health Addict. 2022; 20(2):1273–1288. https://doi.org/10.1007/s11469....
28.
Dolan ED, Mohr D, Lempa M, et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern ed. 2015; 30(5):582–7. https://doi.org/10.1007/s11606....
29.
Schmoldt RA, Freeborn DK, Klevit HD. Physician burnout: recommendations for HMO managers. HMO Pract. 1994; 8(2):58–63.
30.
McMurray JE, Linzer M, Konrad TR, et al. T?h e work lives of women physicians results from the physician work life study. T?h e SGIM career satisfaction study group. J Gen Intern Med. 2000; 15(6):372–80. https://doi.org/10.1111/j.1525....
31.
Labrague LJ, De los Santos JAA. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J Nurs Manag. 2020; 28 (7): 1653–1661.https://doi.org/10.1111/jonm.1....
32.
Labrague LJ, De los Santos JAA. Prevalence and predictors of coronaphobia among frontline hospital and public health nurses. Public Health Nurs. 2021; 38(3): 382–389. https://doi.org/10.1111/phn.12....
33.
Tabachnick BG. Multiple Regression. In: Tabachnick BG, Fidel LS, eds. Using multivariate statistics. 7th ed. Boston: Pearson Education; 2019. p. 104–109.
34.
Zhang WT, Dong W. Chapter 6: multiple linear regression model. In: Advanced textbook for statistical analyses by SPSS. 3rd. Beijing: Higher Education Press; 2018. p. 101–123.
35.
Dal’Bosco EB, Floriano LSM, Skupien SV, et al. Mental health of nursing in coping with COVID-19 at a regional university hospital. Rev Bras Enferm. 2020; 73:e20200434. https://doi.org/10.1590/0034-7....
36.
Maben J, Bridges J. Covid-19: Supporting nurses’ psychological and mental health. J Clin Nurs. 2020; 29(15–16):2742–2750. https://doi.org/10.1111/jocn.1....
37.
Qiu D, Yu Y, Li RQ, et al. Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis. Sleep Med. 2019; 67:258–266. https://doi.org/10.1016/j.slee....
38.
Sampaio F, Sequeira C, Teixeira L. Impact of COVID-19 outbreak on nurses’ mental health: A prospective cohort study. Environ Res. 2021; 194:110620. https://doi.org/10.1016/j.envr....
39.
An Y, Yang Y, Wang A, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. 2020; 276:312–315. https://doi.10.1016/j.jad.2020....
40.
Tu ZH, He JW, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: A cross-sectional study. Medicine (Baltimore). 2020;99:e20769. https://doi.10.1097/MD.0000000....
41.
Labrague LJ, De Los Santos JAA, Fronda DC. Perceived COVID-19-associated discrimination, mental health and professional-turnover intention among frontline clinical nurses: The mediating role of resilience. Int J Ment Health Nurs. 2021; 30(6):1674–1683. https://doi. 10.1111/inm.12920.
42.
Wang YX, Guo HT, Du XW, et al. Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine (Baltimore). 2020; 26;99(26):e20965. https://doi. 10.1097/MD.0000000000020965.
43.
McDonald T. Speak truth to power and consolidate the nursing visibility gained during COVID-19. Int Nurs Rev. 2022. https://doi.org/10.1111/inr.12.... Epub ahead of print.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.