Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Medical staff in Poland in 2012–2022 – challenges related to the distribution of human resources
1
Medical University, Białystok, Poland
These authors had equal contribution to this work
Corresponding author
Ann Agric Environ Med. 2024;31(3):382-387
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Today’s shortage of medical staff is a global healthcare issue. This leads to unfulfilled, growing health needs and rising wage pressure. The aim of the study is to evaluate employment trends among medical professionals in Poland from 2012–2022, paying particular attention to the employment sector, forms of employment, age, gender, and geographic distribution.
Material and methods:
A quantitative analysis was carried out using public records and documents to identify trends over a decade, by the desk research method. Sources included: Organisation for Economic Co-operation and Development databases, Central Statistical Office databases and Ministry of Health Statistical Bulletins.
Results:
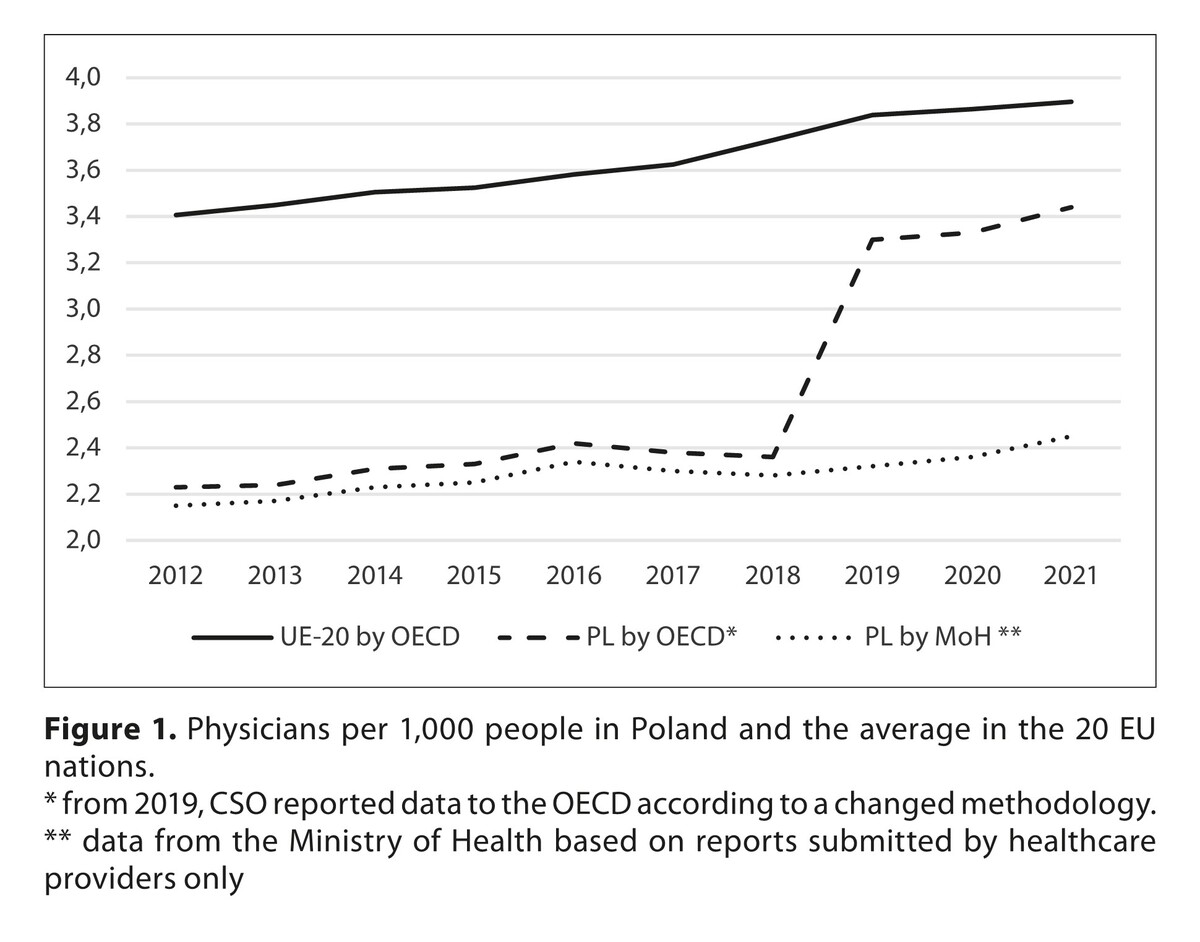
The observed increasing trend of physicians and nurses ratio after 2019, was caused mainly by a change in the methodology of calculating the indicator. There was a notable increase in the number of contracted medical professionals – 303% for nurses and 312% for midwives, and a decrease in the number of employed professionals. The number of contractors and employers in in-patient and long-term care has increased across all professional medical groups, while in outpatient care, the number has decreased. A definite ageing of medical staff was noted, with the percentage of midwives over 65 rising from 5.7% to 19.1%, and nurses over 65 rising from 5.4% to 22.3%.
Conclusions:
The demand for health services has increased, but the supply of medical staff has not kept pace with this demand. In addition to strategies related to increasing the number of human resources, solutions to better match resources to sectors of healthcare and better regional distribution should be considered. Solutions related to the skill-mix concept and the admission of new professions to the health sector may also be an opportunity for consideration.
Today’s shortage of medical staff is a global healthcare issue. This leads to unfulfilled, growing health needs and rising wage pressure. The aim of the study is to evaluate employment trends among medical professionals in Poland from 2012–2022, paying particular attention to the employment sector, forms of employment, age, gender, and geographic distribution.
Material and methods:
A quantitative analysis was carried out using public records and documents to identify trends over a decade, by the desk research method. Sources included: Organisation for Economic Co-operation and Development databases, Central Statistical Office databases and Ministry of Health Statistical Bulletins.
Results:
The observed increasing trend of physicians and nurses ratio after 2019, was caused mainly by a change in the methodology of calculating the indicator. There was a notable increase in the number of contracted medical professionals – 303% for nurses and 312% for midwives, and a decrease in the number of employed professionals. The number of contractors and employers in in-patient and long-term care has increased across all professional medical groups, while in outpatient care, the number has decreased. A definite ageing of medical staff was noted, with the percentage of midwives over 65 rising from 5.7% to 19.1%, and nurses over 65 rising from 5.4% to 22.3%.
Conclusions:
The demand for health services has increased, but the supply of medical staff has not kept pace with this demand. In addition to strategies related to increasing the number of human resources, solutions to better match resources to sectors of healthcare and better regional distribution should be considered. Solutions related to the skill-mix concept and the admission of new professions to the health sector may also be an opportunity for consideration.
REFERENCES (36)
1.
Agyeman-Manu K, Ghebreyesus TA, Maait M, Rafila A, Tom L, Lima NT, Wangmo D, Prioritising the health and care workforce shortage: protect, invest, together. Lancet Glob Health. 2023;11(8):e1162-e1164. doi:10.1016/S2214-109X(23)00224-3.
2.
Chen L, Evans T, Anand S, Boufford JI, Brown H, Chowdhury M, Cueto M, Dare L, Dussault G, Elzinga G, Fee E, Habte D, Hanvoravongchai P, Jacobs M, Kurowski C, Michael S, Pablos-Mendez A, Sewankambo N, Solimano G, Stilwell B, de Waal A, Wibulpolprasert S. Human resources for health: overcoming the crisis. Lancet. 2004;364(9449):1984–90. doi:10.1016/S0140-6736(04)17482-5.
3.
Džakula A, Relić D. Health workforce shortage – doing the right things or doing things right? Croat Med J. 2022;63(2):107–109. doi:10.3325/cmj.2022.63.107.
4.
Journal of Laws of the Republic of Poland, Warsaw, 26th August 2014, item 1125, Regulation of the Minister of Health of 21st August 2014 on the cap on medical and medical-dental student number.
5.
Journal of Laws of the Republic of Poland, Warsaw, 11th July 2013, item 1322, Regulation of the Minister of Health of 7th July 2023 on the cap on medical and medical-dental student number.
6.
OECD, Health at a Glance 2023: OECD Indicators, OECD Publishing. 2023; https://doi.org/10.1787/7a7afb... (access: 2023.12.17).
7.
Domagała A, Dubas-Jakóbczyk K, Migration intentions among physicians working in Polish hospitals – Insights from survey research. Health Policy. 2019;123(8):782–789. doi: 10.1016/j.healthpol.2019.06.008.
8.
Supreme Medical Chamber in Warsaw. Numerical Summary by the Number of Issued Certificates by Voivodeship of Residence and Period of Certificate Issuance, with a Breakdown for Certificates for Physicians, Dental Physicians, and Certificates Confirming Specialty Equivalence. Version number of the summary: 5. 2023; https://nil.org.pl/rejestry/ce... (access: 2023.12.18).
9.
World Health Organization. Regional Office for Europe. Health workforce: fact sheet on Sustainable Development Goals (SDGs): health targets. World Health Organization Regional Office for Europe. 2018; https://iris.who.int/handle/10... (access: 2023.12.18).
10.
GBD 2017 SDG Collaborators. Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health-related Sustainable Development Goals for 195 countries and territories: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):2091–2138. doi:10.1016/S0140-6736(18)32281-5.
11.
Maier CB, Kroezen M, Busse R, Wismar M, editors. Skill-mix Innovation, Effectiveness and Implementation: Improving Primary and Chronic Care. Cambridge: Cambridge University Press; 2022. doi:10.1017/9781009031929.
12.
OECD/European Union, Health at a Glance: Europe 2018: State of health in the EU cycle. OECD Publishing. 2018; https://doi.org/10.1787/health... (access: 2023.12.19).
13.
Moore N. Desk research. In: How to Do Research: The Practical Guide to Designing and Managing Research Projects. Facet; 2006. p. 106–111. doi: 10.29085/9781856049825.011.
14.
OECD, Doctors (indicator). 2023; doi:10.1787/4355e1ec-en (access: 2023.12.19).
15.
OECD, Nurses (indicator). 2023; doi:10.1787/283e64de-en (access: 2023.12.19).
16.
Central Statistical Office. Medical Staff (2012–2021). 2023; available at https://bdl.stat.gov.pl/bdl (access: 2023.12.19).
17.
e-Health Center, Ministry of Health Statistical Bulletins (indicator). 2022; available at https://ezdrowie.gov.pl/portal... (accessed: 2023.12.19).
18.
Central Statistical Office. Human resources in selected medical professions based on administrative sources between 2019 and 2020. 2023; https://stat.gov.pl/obszary-te... (access: 2023.12.20).
19.
OECD/European Union, Health at a Glance: Europe 2022, State of Health in the EU Cycle. OECD Publishing; 2022. https://doi.org/10.1787/507433... (access: 2023.12.20).
20.
Malinowska-Lipień I, Gabryś T, Kózka, M, Gniadek A, Wadas T, Ozga E, Brzostek T. Dual practice of nurses in Poland against the current staff resources. Med Pr. 2021;72(2),113–121. doi:10.13075/mp.5893.01018.
21.
Maier T, Afentakis A. Forecasting supply and demand in nursing professions: impacts of occupational flexibility and employment structure in Germany. Hum Resour Health. 2013;11,24. doi:10.1186/1478-4491-11-24.
22.
Martin CA, Medisauskaite A, Gogoi M, Teece L, Nazareth J, Pan D, et al. Discrimination, feeling undervalued, and health-care workforce attrition: an analysis from the UK-REACH study. Lancet. 2023;402(10405):845–848. doi:10.1016/S0140-6736(23)01365-X.
23.
Marcinowicz L, Owlasiuk A, Perkowska E. Exploring the ways experienced nurses in Poland view their profession: a focus group study. Int Nurs Rev. 2016;336–43. doi:10.1111/inr.12294.
24.
OECD/European Observatory on Health Systems and Policies, Poland: Country Health Profile 2023. State of Health in the EU. OECD Publishing; 2023. https://doi.org/10.1787/f597c8... (access: 2023.12.20).
25.
Tinios P, Valvis Z, Georgiadis T. Heterogeneity in Long-Term Care for Older Adults in Europe: Between Individual and Systemic Effects. J. Ageing Longev. 2022;2,1:53–177. https://doi.org/10.3390/jal202... (access: 2023.12.21).
26.
Deusdad BA, Pace C, Anttonen A. Facing the Challenges in the Development of Long-Term Care for Older People in Europe in the Context of an Economic Crisis. J Soc Serv Res. 2016;42(2):144–150. doi:10.1080/01488376.2015.1133147.
27.
Boniol M, Kunjumen T, Nair TS, Siyam A, Campbell J, Diallo K. The global health workforce stock and distribution in 2020 and 2030: a threat to equity and ‘universal’ health coverage? BMJ Glob Health. 2022;7(6):e009316. doi:10.1136/bmjgh-2022-009316.
28.
Ryan C, Bergin M, White M, Wells JSG, Ageing in the nursing workforce – a global challenge in an Irish context. Int Nurs Rev. 2019;66(2):157–164. doi:10.1111/inr.12482.
29.
Alnazly, E, Khraisat, OM, Al-Bashaireh AM, Bryant CL. Anxiety, depression, stress, fear, and social support during the COVID-19 pandemic among Jordanian healthcare workers. PLos ONE. 2021;16(3): e0247679. doi:10.1371/journal.pone.0247679.
30.
Jonsson R, Lindegård A, Björk L, Nilsson K. Organizational Hindrances to the Retention of Older Healthcare Workers. NJWLS. 2020;10(1). https://doi.org/10.18291/njwls... (access: 2023.12.21).
31.
Dobson H, Malpas CB, Burrell AJC, Gurvich C, Chen L, Kulkarni J, Winton-Brown T. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas Psychiatry. 2021;29(1):26–30. doi:10.1177/1039856220965045.
32.
Maślach D, Karczewska B, Szpak A, Charkiewicz A, Krzyżak M, Does place of residence affect patient satisfaction with hospital health care? Ann Agric Environ Med. 2020;27(1):86–90. doi:10.26444/aaem/116574.
33.
Benahmed N, Deliège D, De Wever A, Pirson M. La planification des médecins en Europe: une revue de la littérature des modèles de projection [Medical human resources planning in Europe: A literature review of the forecasting models]. Rev Epidemiol Sante Publique. 2018;66(1):63–73. doi:10.1016/j.respe.2017.10.001.
34.
Boniol M, Kunjumen T, Nair TS, Siyam A, Campbell J, Diallo K, The global health workforce stock and distribution in 2020 and 2030: a threat to equity and ‘universal’ health coverage? BMJ Glob Health. 2022;7(6):e009316. doi: 10.1136/bmjgh-2022-009316.
35.
Ministry of Health of Poland. Supply and demand model for doctors. 2023. Available at https://basiw.mz.gov.pl/mapy-i... (access: 2024.02.29).
36.
Supreme Chamber of Control’s report: Education and professional training of medical staff; KZD.410.005.00.2015, reg. no. 220/2015/P/15/060/KZD. 2015; https://www.nik.gov.pl/plik/id... (access: 2023.12.17).
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.