Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Geriatric Depression Scale – 30 assessments: face-to-face or telephone interviews for older people – a randomized crossover study
1
Institute of Medical Sciences, College of Medical Sciences, University of Rzeszow, Poland
2
Laboratory of Geronto-prophylaxis, Center for Innovative Research in Medical and Natural Sciences, Rzeszow of University, Poland
3
Institute of Health Sciences, College of Medical Sciences, University of Rzeszów, Poland
4
Faculty of Medicine, Lazarski University, Warsaw, Poland
5
Department of Geriatrics, Neurosciences, Orthopaedics, Centre for Geriatric Medicine (CEMI), Institute of Internal
Medicine and Geriatrics, Catholic University of the Sacred Heart, Milan, Italy
6
Rehabilitation Unit, ‘Mons. L. Novarese’ Hospital, Moncrivello, Italy
7
Physical Medicine and Rehabilitation Unit, Department of Medical and Surgical Sciences, ‘Magna Graecia’ University,
Catanzaro, Italy
8
Research Centre on Musculoskeletal Health, MusculoSkeletalHealth@UMG, ‘Magna Graecia’ University, Catanzaro, Italy
Corresponding author
Agnieszka Beata Ćwirlej-Sozańska
Institute of Health Sciences, College of Medical Sciences, University of Rzeszow, Warzywna 1a, 35-959, Rzeszów, Poland
Institute of Health Sciences, College of Medical Sciences, University of Rzeszow, Warzywna 1a, 35-959, Rzeszów, Poland
Ann Agric Environ Med. 2024;31(1):72-77
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The Geriatric Depression Scale – 30 (GDS-30) for detecting depressive disorders provides an objective and reliable outcome measure validated by many studies and scientific articles. The aim of the study was to compare the concordance of measurements using the GDS-30 conducted in face-to-face and telephone interviews.
Material and methods:
The study design was approved by the Bioethical Committee of the University of Rzeszów (Resolution No. 2022/075). Study participants were community-dwelling older people in south-eastern Poland, aged 60 years and over, with a normal cognitive status. They were divided into 2 groups, each examined with the Geriatric Depression Scale – 30 questionnaire. The first group (G1) was examined first by means of direct contact (A), and the second group (G2) by telephone (B). After an average period of 2 weeks, the study was repeated, this time swapping the method of contact: in G1 telephone contact (B) was used, in G2 face-to-face contact (A).
Results:
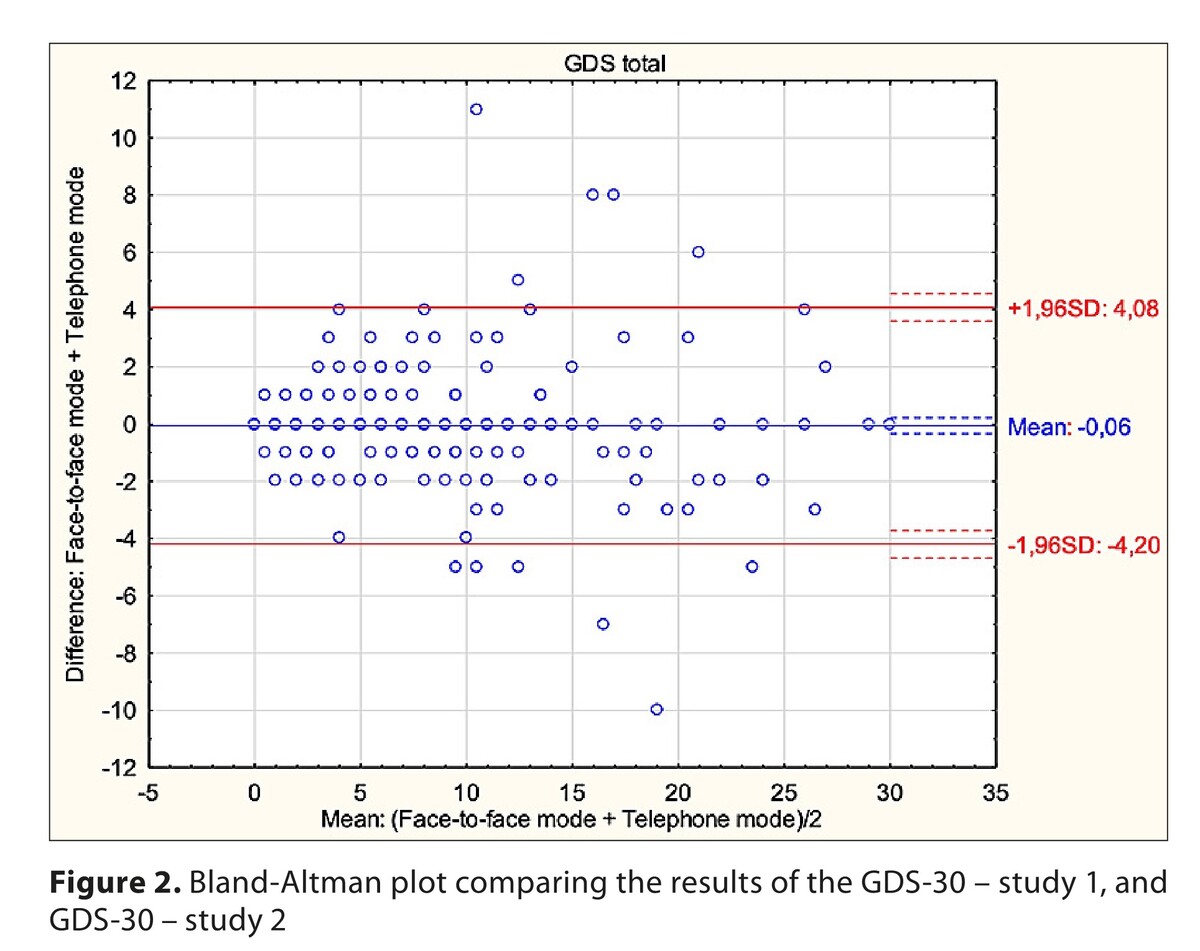
The study involved a group of 225 people (128 women and 97 men), mean aged 68.2 years, randomly divided into the 2 groups (G1 and G2). Cohen’s kappa coefficient analysis showed good (14 questions) to very good (16 questions) concordance for individual responses to questions. Analysis of Krippendorf’s alpha coefficient values showed very good concordance for results on the whole questionnaire. Good concordance of the means of measurement was also confirmed by the Bland and Altman method, where more than 95% of the sample was within the 95% concordance limits.
Discussion and Conclusions:
Findings of the study showed that the GDS-30 questionnaire had a high compliance in both face-to-face and telephone surveys.
The Geriatric Depression Scale – 30 (GDS-30) for detecting depressive disorders provides an objective and reliable outcome measure validated by many studies and scientific articles. The aim of the study was to compare the concordance of measurements using the GDS-30 conducted in face-to-face and telephone interviews.
Material and methods:
The study design was approved by the Bioethical Committee of the University of Rzeszów (Resolution No. 2022/075). Study participants were community-dwelling older people in south-eastern Poland, aged 60 years and over, with a normal cognitive status. They were divided into 2 groups, each examined with the Geriatric Depression Scale – 30 questionnaire. The first group (G1) was examined first by means of direct contact (A), and the second group (G2) by telephone (B). After an average period of 2 weeks, the study was repeated, this time swapping the method of contact: in G1 telephone contact (B) was used, in G2 face-to-face contact (A).
Results:
The study involved a group of 225 people (128 women and 97 men), mean aged 68.2 years, randomly divided into the 2 groups (G1 and G2). Cohen’s kappa coefficient analysis showed good (14 questions) to very good (16 questions) concordance for individual responses to questions. Analysis of Krippendorf’s alpha coefficient values showed very good concordance for results on the whole questionnaire. Good concordance of the means of measurement was also confirmed by the Bland and Altman method, where more than 95% of the sample was within the 95% concordance limits.
Discussion and Conclusions:
Findings of the study showed that the GDS-30 questionnaire had a high compliance in both face-to-face and telephone surveys.
REFERENCES (37)
1.
Zenebe Y, Akele B, Selassie M, et al. Prevalence and determinants of depression among old age: a systematic review and meta-analysis. Ann Gen Psychiatry. 2021;20(1):55. https://doi.org/10.1186/s12991....
2.
Corrêa ML, Carpena MX, Meucci RD, et al. Depression in the elderly of a rural region in Southern Brazil. Cien Saude Colet. 2020;25(6):2083–2092. https://doi:10.1590/1413-81232....
3.
Maier A, Riedel-Heller SG, Pabst A, et al. Risk factors and protective factors of depression in older people 65+. A systematic review. PLoS One. 2021;16(5):e0251326. https://doi:10.1371/journal.po....
4.
Lechowski Ł, Jasion A. Spatial Accessibility of Primary Health Care in Rural Areas in Poland. Int J Environ Res Public Health. 2021;2,18(17):9282. https://doi:10.3390/ijerph1817....
5.
Piras F, Banaj N, Porcari DE, et al. Later life depression as risk factor for developing dementia: epidemiological evidence, predictive models, preventive strategies and future trends. Minerva Med. 2021;112(4):456–466. https://doi.org/10.23736/S0026....
6.
World Health Organization. Ageing and health. Available online: https://www.who.int/news-room/... (access:15.06.2023).
7.
Borges MK, Aprahamian I, Romanini CV, et al. Depression as a determinant of frailty in late life. Aging Ment Health. 2021;25(12):2279–2285. https://doi:10.1080/13607863.2....
8.
Zhang Y, Chen Y, Ma L. Depression and cardiovascular disease in elderly: Current understanding. J Clin Neurosci. 2018;47:1–5. https://doi:10.1016/j.jocn.201....
9.
Meng R, Yu C, Liu N, et al. China Kadoorie Biobank Collaborative Group. Association of Depression With All-Cause and Cardiovascular Disease Mortality Among Adults in China. JAMA Netw Open. 2020; 3(2):e1921043. https://doi: 10.1001/jamanetworkopen.2019.21043.
10.
Malhi GS, Mann JJ. Depression. Lancet. 2018;392(10161):2299–2312. https://doi: 10.1016/S0140-6736(18)31948-2.
11.
World Health Organization. Mental health of older adults. Available online: https://www.who.int/news-room/.... (access:15.06.2023).
12.
Sun X, Zhou M, Huang L, et al. Depressive costs: medical expenditures on depression and depressive symptoms among rural elderly in China. Public Health. 2020;181:141–150. https://doi:10.1016/j.puhe.201....
13.
Darbà J, Marsà A. Characteristics, management and medical costs of patients with depressive disorders admitted in primary and specialised care centres in Spain between 2011 and 2016. PLoS One. 2020;15(2):e0228749. https://doi:10.1371/journal.po....
14.
Beeler PE, Cheetham M, Held U, et al. Depression is independently associated with increased length of stay and readmissions in multimorbid inpatients. Eur J Intern Med. 2020;73:59–66. https://doi: 10.1016/j.ejim.2019.11.012.
15.
Reynolds CF 3rd, Jeste DV, Sachdev PS, Blazer DG. Mental health care for older adults: recent advances and new directions in clinical practice and research. World Psychiatry. 2022;21(3):336–363. http://doi:10.1002/wps.20996.
16.
Piotrowicz K, Romanik W, Skalska A, et al. The comparison of the 1972 Hodkinson’s Abbreviated Mental Test Score (AMTS) and its variants in screening for cognitive impairment. Aging Clin Exp Res. 2019; 31(4):561–566. https://doi.org/10.1007/s40520....
17.
Yesavage JA, Brink T L, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Research. 1982;17(1):37–49. https://doi.org/10.1016/0022-3....
18.
Albiński R, Kleszczewska-Albińska A, Bedyńska S. Geriatric Depression Scale (GDS). Validity and reliability of different versions of the scale--review. Psychiatr Pol. 2011;45(4):555–62. Polish.
19.
Sozański B, Ćwirlej-Sozańska, AB, Wilmowska-Pietruszyńska A, et al. Establishing score equivalence of the GDS-30 scale and International Classification of Functioning, Disability and Health range, using Rasch analysis. Ann Agric Environ Med. 2023;30(1):105–110. https://doi.org/10.26444/aaem/....
20.
World Health Organization. Coronavirus disease (COVID19) pandemic. Available online: https://www.who. int/emergencies/diseases/novel-coronavirus-2019 (access:15.06.2023).
21.
Jakovljevic M, Bjedov S, Jaksic N, et al. COVID-19 Pandemia and Public and Global Mental Health from the Perspective of Global Health Securit. Psychiatr Danubina. 2020;32(1):6–14. https://doi.org/10.24869/psyd.....
22.
Bitkowska A, Pomaranik W, Hawrysz L, et al. Telemedycyna w czasie pandemii covid-19. Doświadczenia pacjentów z systemem w świetle wyników badań w Polsce. Przegląd Organizacji. 2021;8(979):20–27.
23.
Klaassen B, van Beijnum BJ, Hermens HJ. Usability in telemedicine systems-A literature survey. Int J Med Inform. 2016;93:57–69. http://doi: 10.1016/j.ijmedinf.2016.06.004.
24.
Mann DM, Chen J, Chunara R, et al. COVID-19 transforms health care through telemedicine: Evidence from the field. JAMIA. 2020;27(7):1132–1135. https://doi.org/10.1093/jamia/....
25.
Paolucci T, de Sire A, Ferrillo M, di Fabio D, Molluso A, Patruno A, Pesce M, Lai C, Ciacchella C, Saggino A, Agostini F, Tommasi M. Telerehabilitation proposal of mind-body technique for physical and psychological outcomes in patients with fibromyalgia. Front Physiol. 2022;26,13:917956. https://doi.org/10.3389/fphys.....
26.
Eurostat Old-Age Dependency Ratio Increasing in the EU. https://ec.europa.eu/eurostat/... (access:15.06.2023).
27.
Krishnamoorthy Y, Rajaa S, Rehman T. Diagnostic accuracy of various forms of geriatric depression scale for screening of depression among older adults: Systematic review and meta-analysis. Arch Gerontol Geriatr. 2020;87:104002. http://doi:10.1016/j.archger.2....
28.
Masson LF, McNeill G, Tomany JO, et al. Statistical approaches for assessing the relative validity of a food-frequency questionnaire: use of correlation coefficients and the kappa statistic. Public Health Nutr. 2003;6(3): 313–321. https://doi.org/10.1079/PHN200....
29.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476): 307–10.
30.
Wadolowska L. Walidacja metod i mierniki statystyczne. Przewodnik metodyczny badań sposobu żywienia. Komitet Nauki o Żywieniu Człowieka Polskiej Akademii Nauk. Gronowska-Senger A. Warszawa 2013;3:1–18. https://doi:10.13140/2.1.1438.....
31.
Martin-Khan M, Wootton R, Gray LA. systematic review of the reliability of screening for cognitive impairment in older adults by use of standardised assessment tools administered via the telephone. J Telemed Telecare. 2010;16(8):422–8.
32.
Loh PK, Ramesh P, Maher S, et al. Can patients with dementia be assessed at a distance? The use of Telehealth and standardised assessments. Internal Med J. 2004;34(5):239–242. https://doi.org/10.1111/j.1444....
33.
Monteiro IM, Boksay I, Auer SR, et al. Reliability of routine clinical instruments for the assessment of Alzheimer’s disease administered by telephone. J Geriatr Psychiatry Neurol. 1998;11(1):18–24. https://doi.org/10.1177/089198....
34.
Conwell Y, Simning A, Driffill N, et al. Validation of telephone-based behavioral assessments in aging services clients. Int Psychogeriatr. 2018;30(1):95–102. https://doi.org/10.1017/S10416....
35.
Dauphinot V, Boublay N, Moutet C, et al. Comparison of Instrumental Activities of Daily Living assessment by face-to-face or telephone interviews: a randomized, crossover study. Alzheimer’s Res Therapy. 2020;12(1):24. https://doi.org/10.1186/s13195....
36.
Bednorz A, Derejczyk J, Kozub J, et al. Zastosowanie wideo konsultacji z wykorzystaniem Geriatrycznej Skali Depresji (GDS) do rozpoznawania depresji u osób starszych, jako próba telediagnostyki w geriatrii. Geriatria. 2014; 8:141–149.
37.
Carlew AR, Fatima H, Livingstone JR, et al. Cognitive Assessment via Telephone: A Scoping Review of Instruments. Arch Clin Neuropsychol. 2020;35(8):1215–1233. https://doi.org/10.1093/arclin....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.