Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Factors associated with the use of public eHealth services in Poland – a 2022 nationwide cross-sectional survey
1
Central Clinical Hospital of the Ministry of the Interior and Administration, Warsaw, Poland
2
School of Public Health, Centre of Postgraduate Medical Education, Warsaw, Poland
Corresponding author
Krzysztof Płaciszewski
Central Clinical Hospital of the Ministry of the Interior and Administration in Warsaw, 02-507, Warsaw, Poland
Central Clinical Hospital of the Ministry of the Interior and Administration in Warsaw, 02-507, Warsaw, Poland
Ann Agric Environ Med. 2023;30(1):127-134
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Poland is an example of a European country that has made significant progress in digitizing healthcare during the last 5 years. There is limited data on the use of eHealth services by different socio-economic groups in Poland during the COVID-19 pandemic The aim of the study was to characterize public attitudes towards the use of e-Health services in Poland, as well as to identify factors associated with the use of e-Health services among adults in Poland.
Material and methods:
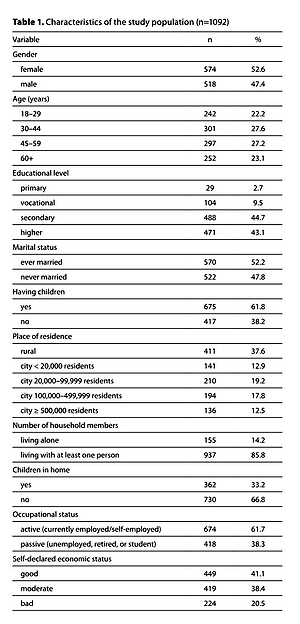
A questionnaire-based survey was carried out during 9–12 September 2022. A computer-assisted web interview methodology was used. A nationwide random quota sample of 1,092 adult Poles was selected. Questions on the use of 6 different public eHealth services in Poland and soci-economic characteristics were addressed.
Results:
Two-thirds of participants (67.1%) had received an e-prescription in the last 12 months. More than half of the participants used the Internet Patient Account (58.2%) or the patient.gov.pl website (54.9%). One-third of the participants had teleconsultation with a doctor (34.4%), and approximately one-quarter of participants had received electronic sick leave (26.9%) or used electronic information about treatment dates (26.7%). Of the ten different socio-economic factors analyzed in this study, educational level, and place of residence (p<0.05) were the most important factors associated with the use of public eHealth services among adults in Poland.
Conclusions:
Living in rural areas or small cities is associated with a lower level of public eHealth services utilization. A relatively high interest in health education through eHealth methods was observed.
Poland is an example of a European country that has made significant progress in digitizing healthcare during the last 5 years. There is limited data on the use of eHealth services by different socio-economic groups in Poland during the COVID-19 pandemic The aim of the study was to characterize public attitudes towards the use of e-Health services in Poland, as well as to identify factors associated with the use of e-Health services among adults in Poland.
Material and methods:
A questionnaire-based survey was carried out during 9–12 September 2022. A computer-assisted web interview methodology was used. A nationwide random quota sample of 1,092 adult Poles was selected. Questions on the use of 6 different public eHealth services in Poland and soci-economic characteristics were addressed.
Results:
Two-thirds of participants (67.1%) had received an e-prescription in the last 12 months. More than half of the participants used the Internet Patient Account (58.2%) or the patient.gov.pl website (54.9%). One-third of the participants had teleconsultation with a doctor (34.4%), and approximately one-quarter of participants had received electronic sick leave (26.9%) or used electronic information about treatment dates (26.7%). Of the ten different socio-economic factors analyzed in this study, educational level, and place of residence (p<0.05) were the most important factors associated with the use of public eHealth services among adults in Poland.
Conclusions:
Living in rural areas or small cities is associated with a lower level of public eHealth services utilization. A relatively high interest in health education through eHealth methods was observed.
REFERENCES (35)
1.
Hilbert M. Digital technology and social change: the digital transformation of society from a historical perspective. Dialogues Clin Neurosci. 2020;22(2):189–194. https://doi.org/10.31887/DCNS.....
2.
Statista. Number of internet and social media users worldwide as of July 2022. Accesses November 19, 2022. Available online: https://www.statista.com/stati....
3.
Rodríguez-Ríos A, Espinoza-Téllez G, Martínez-Ezquerro JD, et al. Information and Communication Technology, Mobile Devices, and Medical Education. J Med Syst. 2020;44(4):90. https://doi.org/10.1007/s10916....
4.
Jungwirth D, Haluza D. Information and communication technology and the future of healthcare: Results of a multi-scenario Delphi survey. Health Informatics J. 2019;25(1):161–173. https://doi.org/10.1177/146045....
5.
Oh H, Rizo C, Enkin M, et al. What is eHealth? a systematic review of published definitions. World Hosp Health Serv. 2005;41(1):32–40.
6.
World Health Organization. Atlas of eHealth country profiles: the use of eHealth in support of universal health coverage: based on the findings of the third global survey on eHealth 2015. WHO Global Observatory for eHealth. 2016;9–11.
7.
Sanyal C, Stolee P, Juzwishin D, et al. Economic evaluations of eHealth technologies: A systematic review. PLoS One. 2018;13(6):e0198112. https://doi.org/10.1371/journa....
8.
Schneider JA, Holland CP. eHealth Search Patterns: A Comparison of Private and Public Health Care Markets Using Online Panel Data. J Med Internet Res. 2017;19(4):e117. https://doi.org/10.2196/jmir.6....
9.
Glinkowski WM, Karlińska M, Karliński M, et al. Telemedicine and eHealth in Poland from 1995 to 2015. Adv Clin Exp Med. 2018;27(2):277–282. https://doi.org/10.17219/acem/....
10.
Płaciszewski KB. E-health – use of information and communications technology (ICT) in Polish health care system. Med Og Nauk Zdr. 2022;28(2):126–131. https://doi.org/10.26444/monz/....
11.
European Commision. eHealth: Digital health and care. Accesses November 19, 2022. Available online: https://health.ec.europa.eu/eh....
12.
Lupiánez-Villanueva F, Devaux A, Valverde-Albacete J. Benchmarking Deployment of eHealth among General Practitioners (2018). 1st ed. European Commission, 2018. https://doi.org/10.2759/511610.
13.
Golinelli D, Boetto E, Carullo G, et al. Adoption of Digital Technologies in Health Care During the COVID-19 Pandemic: Systematic Review of Early Scientific Literature. J Med Internet Res. 2020;22(11):e22280. https://doi.org/10.2196/22280.
14.
Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20(1):1193. https://doi.org/10.1186/s12889....
15.
Strzelecka A, Stachura M, Wójcik T, et al. Using affinity analysis in diagnosing the needs of patients as regards e-Health. Ann Agric Environ Med. 2020;27(3):435–441. https://doi.org/10.26444/aaem/....
16.
Nieszporska S. Priorities in the Polish health care system. Eur J Health Econ. 2017;18(1):1–5. doi: https://doi.org/10.1007/s10198....
17.
Wrzosek N, Zimmermann A, Balwicki Ł. A Survey of Patients’ Opinions and Preferences on the Use of E-Prescriptions in Poland. Int J Environ Res Public Health. 2021;18(18):9769. https://doi.org/10.3390/ijerph....
18.
Mularczyk-Tomczewska P, Zarnowski A, Gujski M, et al. Barriers to accessing health services during the COVID-19 pandemic in Poland: A nationwide cross-sectional survey among 109,928 adults in Poland. Front Public Health. 2022;10:986996. https://doi.org/10.3389/fpubh.....
19.
National Health Fund. Electronic information about treatment dates. Accesses November 19, 2022. Available online: https://terminyleczenia.nfz.go...# [Polish].
20.
Republic of Poland. Website of the Ministry of Health and the National Health Fund. Accesses November 19, 2022. Available online: https://pacjent.gov.pl/.
21.
Buliński L, Błachnio A. Health in old age, and patients’ approaches to telemedicine in Poland. Ann Agric Environ Med. 2017;24(2):322–328. https://doi.org/10.26444/aaem/....
22.
Bujnowska-Fedak MM, Waligóra J, Mastalerz-Migas A. The Internet as a Source of Health Information and Services. Adv Exp Med Biol. 2019;1211:1–16. https://doi.org/10.1007/5584_2....
23.
Żarnowski A, Jankowski M, Gujski M. Use of Mobile Apps and Wearables to Monitor Diet, Weight, and Physical Activity: A Cross-Sectional Survey of Adults in Poland. Med Sci Monit. 2022;28:e937948. https://doi.org/10.12659/MSM.9....
24.
Central Statistical Office. Information Society in Poland in 2020. Accesses November 19, 2022. Available online: https://stat.gov.pl/obszary-te....
25.
Pantyley V. Health inequalities among rural and urban population of Eastern Poland in the context of sustainable development. Ann Agric Environ Med. 2017;24(3):477–483. https://doi.org/10.5604/123219....
26.
The National Research Panel “Ariadna”. About us. Ariadna National Research Panel. Accesses November 19, 2022. Available online: https://panelariadna.com/.
27.
Central Statistical Office. National Official Register of the Territorial Division of the Country. Accesses November 18, 2022. Available online: http://eteryt.stat.gov.pl/eTer....
28.
Furlepa K, Tenderenda A, Kozłowski R, et al. Recommendations for the Development of Telemedicine in Poland Based on the Analysis of Barriers and Selected Telemedicine Solutions. Int J Environ Res Public Health. 2022;19(3):1221. https://doi.org/10.3390/ijerph....
29.
Pinkas J, Jankowski M, Szumowski Ł, et al. Public Health Interventions to Mitigate Early Spread of SARS-CoV-2 in Poland. Med Sci Monit. 2020;26:e924730. https://doi.org/10.12659/MSM.9....
30.
Kludacz-Alessandri M, Hawrysz L, Korneta P, et al. The impact of medical teleconsultations on general practitioner-patient communication during COVID- 19: A case study from Poland. PLoS One. 2021;16(7):e0254960. https://doi.org/10.1371/journa....
31.
Karwowski R, Gasiorowska J. Telemedicine consultations in obstetrics and gynecology – a population based study in Polish speaking women. Ginekol Pol. 2018;89(12):677–681. https://doi.org/10.5603/GP.a20....
32.
Grata-Borkowska U, Sobieski M, Drobnik J, et al. Perception and Attitude toward Teleconsultations among Different Healthcare Professionals in the Era of the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(18):11532. https://doi.org/10.3390/ijerph....
33.
Keene J, Li X. Age and gender differences in health service utilization. J Public Health (Oxf). 2005;27(1):74–9. https://doi.org/10.1093/pubmed....
34.
Rój J, Jankowiak M. Socioeconomic Determinants of Health and Their Unequal Distribution in Poland. Int J Environ Res Public Health. 2021;18(20):10856. https://doi.org/10.3390/ijerph....
35.
Genowska A, Fryc J, Pinkas J, et al. Social costs of loss in productivity-related absenteeism in Poland. Int J Occup Med Environ Health. 2017;30(6):917–932. https://doi.org/10.13075/ijome....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.