Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Diet and selected elements of lifestyle in the Polish population before and during the COVID-19 pandemic – a population study
1
Medical University, Warsaw, Poland
Corresponding author
Ann Agric Environ Med. 2023;30(1):118-126
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The COVID-19 pandemic led to the introduction of sanitary restrictions in many countries which necessitated numerous lifestyle changes, especially in the diet. The study aimed to compare the diet and selected lifestyle elements in the Polish population during the COVID-19 pandemic.
Material and methods:
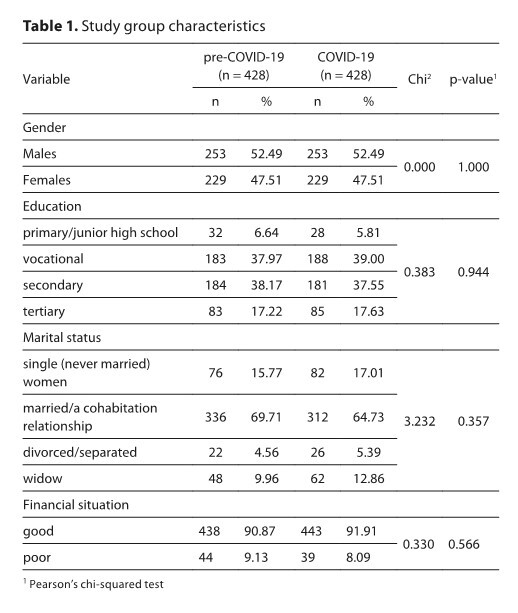
The study group consisted of 964 individuals: 482 before the COVID-19 pandemic (composed using the Propensity Score Matching method) and 482 during the pandemic. The National Health Programme 2017–2020 results were used.
Results:
During the pandemic increased, e.g. the intake of: total lipids (78.4 g vs. 83 g; p<0.035), saturated fatty acids (SFA) (30.4 g vs. 32.3 g; p=0.01), sucrose (56.5 g vs. 64.6 g; p=0.0001), calcium (602.5 mg vs. 666.6 mg; p=0.004), and folate (261.6 mcg vs. 284.7 mcg; p=0.003). When nutrient densities of pre-Covid-19 and COVID-19 diets were compared, some differences were noted; per 1,000 kcal the amounts decreased of plant protein (13.7 g vs. 13.1 g; p=0.001), carbohydrates (130.8 g vs. 128.0 g; p=0.021), fibre (9.1 g vs. 8.4 g; p=0.000), sodium (1,968.6 mg vs. 1,824.2 mg; p=0.000); while the amounts increased of total lipids (35.9 g vs. 37.0 g; p=0.001), SFA (14.1 g vs. 14.7 g; p=0.003), and sucrose (26.4 g vs. 28.4 g; p=0.001). The COVID-19 pandemic had no effect on alcohol consumption, the number of smokers increased (from 131 to 169), sleep duration during weekdays, and the number of persons with low physical activity (182 vs. 245; p<0.001).
Conclusions:
Numerous unfavourable changes occurred in the diet and lifestyle during the COVID-19 pandemic, which may contribute to the exacerbation of health problems in the future. Nutrient density in the diet combined with well-designed consumer education may underlie the development of diet recommendations.
The COVID-19 pandemic led to the introduction of sanitary restrictions in many countries which necessitated numerous lifestyle changes, especially in the diet. The study aimed to compare the diet and selected lifestyle elements in the Polish population during the COVID-19 pandemic.
Material and methods:
The study group consisted of 964 individuals: 482 before the COVID-19 pandemic (composed using the Propensity Score Matching method) and 482 during the pandemic. The National Health Programme 2017–2020 results were used.
Results:
During the pandemic increased, e.g. the intake of: total lipids (78.4 g vs. 83 g; p<0.035), saturated fatty acids (SFA) (30.4 g vs. 32.3 g; p=0.01), sucrose (56.5 g vs. 64.6 g; p=0.0001), calcium (602.5 mg vs. 666.6 mg; p=0.004), and folate (261.6 mcg vs. 284.7 mcg; p=0.003). When nutrient densities of pre-Covid-19 and COVID-19 diets were compared, some differences were noted; per 1,000 kcal the amounts decreased of plant protein (13.7 g vs. 13.1 g; p=0.001), carbohydrates (130.8 g vs. 128.0 g; p=0.021), fibre (9.1 g vs. 8.4 g; p=0.000), sodium (1,968.6 mg vs. 1,824.2 mg; p=0.000); while the amounts increased of total lipids (35.9 g vs. 37.0 g; p=0.001), SFA (14.1 g vs. 14.7 g; p=0.003), and sucrose (26.4 g vs. 28.4 g; p=0.001). The COVID-19 pandemic had no effect on alcohol consumption, the number of smokers increased (from 131 to 169), sleep duration during weekdays, and the number of persons with low physical activity (182 vs. 245; p<0.001).
Conclusions:
Numerous unfavourable changes occurred in the diet and lifestyle during the COVID-19 pandemic, which may contribute to the exacerbation of health problems in the future. Nutrient density in the diet combined with well-designed consumer education may underlie the development of diet recommendations.
ABBREVIATIONS
BMI – Body Mass Index; CAPI – Computer Assisted Personal Interviews method; CATI – Computer Assisted Telephone
Interviews method; COVID-19 – group, respondents during COVID-19 pandemic; DIETA 6.0 – 6.0 Diet Programme for
Planning and Ongoing Evaluation of Individual and Collective Nutrition in Methodical Guide of Dietary Research; GDP
– Gross Domestic Product; KomPAN – Dietary Habits and Nutrition Beliefs Questionnaire; n-3 FA – n-3 fatty acids; NHP –
National Health Programme; pre-Covid-19 group – respondents before COVID-19 pandemic; SFA – saturated fatty acid
ACKNOWLEDGEMENTS
The study was carried out under the National Health
Programme 2016–2020 (Contract Nos. 6/1/3.1.1c/
NPZ/2017/1210/644 and 6/1/3.1.1d/NPZ/2017/1210/645) of
the Ministry of Health in Warsaw, Poland.
REFERENCES (51)
1.
Budreviciute A, Damiati S, Sabir DK, et al. Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Front Public Health. 2020;8:57411. https://doi.org/10.3389/ fpubh.2020.574111.
2.
Ruthsatz M, Candeias V. Non-communicable disease prevention, nutrition and aging. Acta Biomed. 2020;91(2):379–388. https://doi.org/10.23750/abm.v....
3.
Haileamlak A. Physical Inactivity: The Major Risk Factor for Non-Communicable Diseases. Ethiop J Health Sci. 2019;29(1):810. https://doi.org/10.4314%2Fejhs....
4.
Lee IM, Shiroma EJ, Lobelo F, et al. Lancet Physical Activity Series Working Group. Effect of physical inactivity on major noncommunicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–29. https://doi.org/10.1016/S0140-....
5.
Ministry of Health. Coronavirus: Information and Recommendations Available online: https://www.gov.pl/web/koronaw...; (cited 2021 July 15).
6.
Ministry of Science and Higher Education. Restriction of Stationary Education From October 19th Due to COVID-19. Available https://www.gov.pl/web/science...; (cited 2021 July 15).
7.
Calder PC. Nutrition, immunity and COVID-19. BMJ Nutr Prev Health. 2020;3(1):74–92. http://dx.doi.org/10.1136/bmjn....
8.
Górnicka M, Drywień ME, Zielinska MA, et al. Dietary and Lifestyle Changes During COVID-19 and the Subsequent Lockdowns among Polish Adults: A Cross-Sectional Online Survey PLifeCOVID-19 Study. Nutrients. 2020:12(8):2324. https://doi.org/10.3390/nu1208....
9.
Sińska B, Jaworski M, Panczyk M, et al. The Role of Resilience and Basic Hope in the Adherence to Dietary Recommendations in the Polish Population during the COVID-19 Pandemic. Nutrients. 2021;13(6):2108. https://doi.org/10.3390/nu1306....
10.
Drywień ME, Hamulka J, Zielinska-Pokus MA, et al. The COVID-19 Pandemic Lockdowns and Changes in Body Weight among Polish Women. A Cross-Sectional Online Survey PLifeCOVID-19 Study. Sustainability. 2020;12(18):7768. https://doi.org/10.3390/su1218....
11.
Hamulka J, Jeruszka-Bielak M, Górnicka M, et al. Dietary supplements during COVID-19 outbreak. Results of Google trends analysis supported by PLifeCOVID-19 online studies. Nutrients. 2021;13(1):54. https://doi.org/10.3390/nu1301....
12.
Traczyk I, Raciborski F, Kucharska A, et al. A National Study of Nutrition and Nutritional Status of the Adult Polish Population in the Years 2017–2020 before and during the COVID-19 Pandemic—Design and Methods. Nutrients. 2021;13(8):2568. https://doi.org/10.3390/nu1308....
13.
European Food Safety Authority (EFSA). General principles for the collection of national food consumption data in the view of a pan-European dietary survey. EFSA J. 2009;7(12):1435. https://doi.org/10.2903/j.efsa....
14.
European Food Safety Authority (EFSA). Guidance on the EU Menu methodology. EFSA J. 2014;12(12):3944–77. https://doi.org/10.2903/j.efsa....
15.
Przysławski J, Borawska M, Biernat J. Metody badań sposobu żywienia osób dorosłych (Dietary Research Methods for Adults). In: Gronowska-Senger A, editor. Przewodnik metodyczny badań sposobu żywienia (Dietary Research Methodological Guide). Warszaw: The Committee of Human Nutrition Science, Polish Academy of Sciences; 2013. p. 89–94.
16.
Brzozowska A, Roszkowski W. Dietary Research. Metody badań sposobu żywienia osób starszych (Dietary Research Methods for Elderly People). In: Gronowska-Senger A, editor. Przewodnik metodyczny badań sposobu żywienia (Dietary Research Methodological Guide). Warszaw: The Committee of Human Nutrition Science, Polish Academy of Sciences; 2013. p. 96–105.
17.
Wajszczyk B, Chwojnowska Z, Nasiadko D, et al, editors. Instructions for the Use of the 6.0 Diet Program for Planning and Ongoing Evaluation of Individual and Collective Nutrition in Methodical Guide of Dietary Research. Warsaw, Poland: National Food and Nutrition Institute; 2018. Available online: https://www.pzh.gov.pl/uslugi/... (cited 2021 July 26).
18.
Jeżewska-Zychowicz M, Gawęcki J, Wadolowska L, et al. Dietary Habits and Nutrition Beliefs Questionnaire for people 15–65 years old, version 1.1.– interviewer administered questionnaire. In: Gawęcki J, editor. Dietary Habits and Nutrition Beliefs Questionnaire and the Manual for Developing of Nutritional Data. Olsztyn: The Committee of Human Nutrition Science. Polish Academy of Sciences; 2018. p.3–20. Available online: https://knozc.pan.pl/index.php... (cited 2021 July 15).
19.
Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Individuals with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/EC (General Regulation onthe Protection of Data). Available online: https://www.uodo.gov.pl/pl/131... (cited 2021 July 15).
20.
Larsson SC, Kaluza J, Wolk A. Combined impact of healthy lifestyle factors on lifespan: two prospective cohorts. J Intern Med. 2017;282(3):209–219. https://doi.org/10.1111/joim.1....
21.
Stanaway JD, Afshin A, Gakidou E, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923–1994. https://doi.org/10.1016/S0140-....
22.
Drewnowski A. Concept of a nutritious food: toward a nutrient density score. Am J Clin Nutr. 2005;82(4):721–732. https://doi.org/10.1093/ajcn/8....
23.
Connell CL, Zoellner JM, Yadrick MK, et al. Energy density, nutrient adequacy, and cost per serving can provide insight into food choices in the lower Mississippi Delta. J Nutr Educ Behav. 2012;44(2):148–153. https://doi.org/10.1016/j.jneb....
24.
Stefan N, Birkenfeld AL, Schulze MB, et al. Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrinol. 2020;16(7):341–342. https://doi.org/10.1038/s41574....
25.
Tamara A, Tahapary DL. Obesity as a predictor for a poor prognosis of COVID-19: a systematic review. Diabetes Metab Syndr. 2020;14(4):655– 659. https://doi.org/10.1016/j.dsx.....
26.
Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. https://doi.org/10.1016/S0140-....
27.
Olszanecka-Glinianowicz M, Dudek D, Filipiak KJ, et al. Leczenie nadwagi i otyłości w czasie i po pandemii. Nie czekajmy na rozwój powikłań – nowe wytyczne dla lekarzy. Nadciśnienie Tętnicze w Praktyce. 2020;6(1):1–14.
28.
Kris-Etherton PM, Krauss RM. Public health guidelines should recommend reducing saturated fat consumption as much as possible: YES. Am J Clin Nutr. 2020;112(1):13–18. https://doi.org/10.1093/ajcn/n....
29.
Astrup A, Magkos F, Bier DM, et al. Saturated Fats and Health: A Reassessment and Proposal for Food-Based Recommendations: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;76(7):844–857. https://doi.org/10.1016/j.jacc....
30.
Worm N, Weingärtner O, Schulze C, et al. Gesättigte Fettsäuren und kardiovaskuläres Risiko: Ist eine Revision der Ernährungsempfehlungen angezeigt? (Saturated fatty acids and cardiovascular risk: Is a revision of the recommendations on nutrition indicated?). Herz. 2021; Sep 23. German. https://doi.org/10.1007/s00059....
31.
Onishi JC, Häggblom MM, Shapses SA. Can Dietary Fatty Acids Affect the COVID-19 Infection Outcome in Vulnerable Populations? mBio. 2020;11(4):e01723–20. https://doi.org/10.1128/mBio.0....
32.
Lordan R. Dietary supplements and nutraceuticals market growth during the coronavirus pandemic – Implications for consumers and regulatory oversight. PharmaNutrition. 2021;18:100282. https://doi.org/10.1016/j.phan....
33.
Lordan R, Rando HM. COVID-19 Review Consortium, Greene CS. Dietary supplements and nutraceuticals under investigation for COVID-19 prevention and treatment. mSystems. 2021;6(3):e00122–21. https://doi.org/10.1128/mSyste....
34.
Kim H, Rebholz CM, Hegde S, et al. Plant-based diets, pescatarian diets and COVID-19 severity: a population-based case–control study in six countries. BMJ Nutr Prev Health. 2021;4(1):257–256. http://dx.doi.org/10.1136/bmjn....
35.
Ortiz-Prado E, Simbaña-Rivera K, Gómez-Barreno L, et al. Clinical, molecular and epidemiological characterization of the SARS-CoV2 virus and the Coronavirus Disease 2019 (COVID-19): a comprehensive literature review. Diagn Microbiol Infect Dis. 2020;98(1):115094. https://doi.org/10.1016/j.diag....
36.
Bailey RL, West Jr KP, Black RE. The epidemiology of global micronutrient deficiencies. Ann Nut Metab. 2015;66(2):22–33. https://doi.org/10.1159/000371....
37.
Rautiainen S, Manson JE, Lichtenstein AH, et al. Dietary supplements and disease prevention – a global overview. Nat Rev Endocrinol. 2016;12(7):407–420. https://doi.org/10.1038/nrendo....
38.
García-Álvarez L, Fuente-Tomás L, Sáiz PA, et al. Will changes in alcohol and tobacco use be seen during the COVID-19 lockdown? Adicciones. 2020;32(2):85–89. https://doi.org/10.20882/adicc....
39.
Palmer EOC, Trender W, Tyacke RJ, et al. Impact of COVID-19 restrictions on alcohol consumption behaviours. BJPsych Open. 2021;7,1–7. https://doi.org/10.1192/bjo.20....
40.
Sidor A, Rzymski P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients. 2020;12(6):1657. https://doi.org/10.3390/nu1206....
41.
Manthey J, Kilian C, Carr S, et al. Use of alcohol, tobacco, cannabis, and other substances during the first wave of the SARS-CoV-2 pandemic in Europe: a survey on 36,000 European substance users. Subst Abuse Treat Prev Policy. 2021;16:36. https://doi.org/10.1186/s13011....
42.
Stanton R. To QG, Khalesi S, Williams SL, et al. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int J Environ Res Public Health. 2020;17(11):4065. https://doi.org/10.3390/ijerph....
43.
Grossman ER, Benjamin-Neelon SE, Sonnenschein S. Alcohol Consumption during the COVID-19 Pandemic: A Cross-Sectional Survey of US Adults. Int J Environ Res Public Health. 2020;17(24): 9189. https://doi.org/10.3390/ijerph....
44.
Tsigaris P, Teixeira da Silva JA. Smoking Prevalence and COVID-19 in Europe. Nicotine Tob Res. 2020;22(9):1646–1649. https://doi.org/10.1093/ntr/nt....
45.
Jiménez-Ruiz CA, López-Padilla D, Alonso-Arroyo A, et al. COVID-19 and Smoking: A Systematic Review and Meta-Analysis of the Evidence. Arch Bronconeumol. 2021;57:21–34. https://doi.org/10.1016/j.arbr....
46.
Di Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;18:229. https://doi.org/10.1186/s12967....
47.
Jackson SE, Garnett C, Shahab L, et al. Association of the COVID-19 lockdown with smoking, drinking and attempts to quit in England: an analysis of 2019–20 data. Addiction. 2021;116(5):1233–1244. https://doi.org/10.1111/add.15....
48.
Morin CM, Carrier J, Bastien C, et al. Canadian Sleep and Circadian Network. Sleep and circadian rhythm in response to the COVID-19 pandemic. Can J Public Health. 2020;111(5):654–657. doi: 10.17269/s41997-020-00382-7.
49.
Mello MT, Silva A, Guerreiro RC, et al. Sleep and COVID-19: considerations about immunity, pathophysiology, and treatment. Sleep Sci. 2020;13(3): 199–209. doi: 10.5935/1984-0063.20200062.
50.
Ammar A, Brach M, Trabelsi K, et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients. 2020;12(6):1583. https://doi.org/10.3390/nu1206....
51.
Castañeda-Babarro A, Arbillaga-Etxarri A, Gutiérrez-Santamaría B, et al. Physical Activity Change during COVID-19 Confinement. Int J Environ Res Public Health. 2020;17(18):6878. https://doi.org/10.3390/ijerph....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.