Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
COVID 19 – Possible interrelations with respiratory comorbidities caused by occupational exposure to various hazardous bioaerosols. Part I. Occurrence, epidemiology and presumed origin of the pandemic
1
Department of Biological Health Hazards and Parasitology, Institute of Rural Heath, Lublin, Poland
2
Department of Pneumonology, Oncology and Allergology, Medical University, Lublin, Poland
3
Department of Medical Biology, Institute of Rural Heath, Lublin, Poland
Corresponding author
Jacek Dutkiewicz
Department of Biological Health Hazards and Parasitology, Institute of Rural Health, Jaczewskiego 2, 20-090 Lublin, Poland
Department of Biological Health Hazards and Parasitology, Institute of Rural Health, Jaczewskiego 2, 20-090 Lublin, Poland
Ann Agric Environ Med. 2020;27(4):491-504
KEYWORDS
allergensbyssinosisoccupational exposurebioaerosolsendotoxincomorbiditiesODTSCOVID-19SARS-CoV-2hypersensitivity pneumonitis
TOPICS
ABSTRACT
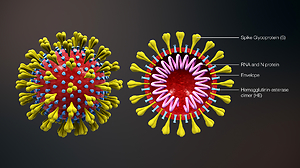
The occupational bioaerosols containing viruses, bacteria, fungi, microbial toxins and plant or animal particles, may evoke infectious, allergic or immunotoxic diseases which may co-exist as comorbidities with COVID-19 and exacerbate the course of disease. They include hypersensitivity pneumonitis (HP) caused mostly by bacteria, fungi, and particles containing animal proteins, and immunotoxic diseases such as organic dust toxic syndrome (ODTS) and byssinosis, caused mostly by bacterial and fungal toxins. The two most probable scenarios of possible interrelations between these three comorbidities (CM) and COVID-19 are: 1) ‘Triggering’ – when infection with SARS-CoV-2 triggers severe CM after bioaerosol exposure; 2) ‘Reverse triggering’ when exposure to bioaerosol exacerbates a symptomless or mild course of COVID-19, and evokes a severe disease. The occupations mostly endangered by COVID-19 as the result of exposure to SARS-CoV-2 bioaerosol, or to other bioaerosols which may exacerbate this disease, include: health care workers, social workers, breeders of fur animals, slaughterhouse workers, workers engaged in the processing and selling of seafood, and probably also agricultural workers, mainly in the developing countries. The authors present a hypothesis for the origin of the present pandemic. It assumes that a mild form of the present SARS-CoV-2 that is supposedly circulating among the Chinese population in the eastern part of the country, mutated under the influence of as yet unknown factor(s) present in the Chinese seafood markets, probably component(s) of bioaerosols, into the virulent and highly contagious form, known as the present SARS-CoV-2, under a scenario similar to that the authors have named ‘Reverse triggering’.
Dutkiewicz J, Mackiewicz B, Lemieszek MK. COVID 19: Possible interrelations with respiratory comorbidities caused by occupational exposure to various hazardous bioaerosols. Part I. Occurrence, epidemiology and presumed origin of the pandemic. Ann Agric Environ Med. 2020; 27(4): 491–504. doi: 10.26444/aaem/130871
REFERENCES (99)
1.
Domingo P, Mur I, Pomar V, Corominas H, Casademont J, de Benito N. The four horsemen of a viral Apocalypse: The pathogenesis of SARS-CoV-2 infection (COVID-19). EBioMedicine 2020; 58: 102887.
2.
Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, et al. Coronavirus disease 2019–COVID-19. Clin Microbiol Rev. 2020; 33: e00028-20.
3.
Zhang R, Li Y, Zhang AL, Wang Y, Molina MJ. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc Natl Acad Sci USA 2020; 117: 14857–14863. doi: 10.1073/pnas.2009637117.
4.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506.
5.
Sierpiński R, Pinkas J, Jankowski M, Juszczyk G, Topór-Mądry R, Szumowski Ł. Occupational risks for SARS-CoV-2 infection: The Polish experience. Int J Occup Med Environ Health. 2020; 33(6): 1–9.
6.
Hosoki K, Chakraborty A, Sur S. Molecular mechanisms and epidemiology of COVID-19 from an allergist’s perspective. J Allergy Clin Immunol. 2020; 146: 285–299.
7.
Liu S, Zhi Y, Ying S. COVID-19 and asthma: reflection during the pandemic. Clin Rev Allergy Immunol. 2020; 59: 78–88.
8.
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020; 94: 91–95.
9.
24th Collegium Ramazzini statement: Prevention of work-related infection in the COVID-19 pandemic. Int J Occup Med Environ Health 2020; 33(4): 535–557.
10.
Lacey J, Dutkiewicz J. Bioaerosols and occupational lung disease. J Aerosol Sci. 1994; 25: 1371–1404.
11.
Dutkiewicz J, Cisak E, Sroka J, Wójcik-Fatla A, Zając V. Biological agents as occupational hazards – selected issues. Ann Agric Environ Med. 2011; 18: 286–293.
12.
Mackiewicz B, Skórska C, Dutkiewicz J. Relationship between concentrations of microbiological agents in the air of agricultural settings and occurrence of work-related symptoms in exposed persons. Ann Agric Environ Med. 2015; 22: 473–477.
13.
Dutkiewicz J. Biological agents of occupational hazard in agriculture and forestry. Ubezpieczenia w Rolnictwie, Materiały i Studia, Kwartalnik. 2017; 63: 7–37 (in Polish).
14.
Górny RL, Dutkiewicz J. Evaluation of microorganisms and endotoxin levels of indoor air in living rooms occupied by cigarette smokers and non-smokers in Sosnowiec, Upper Silesia, Poland. Aerobiologia. 1998; 14: 235–239.
15.
Dutkiewicz J, Tucker J, Burrell R, Olenchock SA, Schwegler-Berry D, Keller III GE, et al. Ultrastructure of the endotoxin produced by Gram-negative bacteria associated with organic dusts. System Appl Microbiol. 1992; 15: 474–485.
16.
Dutkiewicz J, Krysińska-Traczyk E, Skórska C, Sitkowska J, Prażmo Z., Urbanowicz B. Exposure of agricultural workers to airborne microorganisms and endotoxin during handling of various vegetable products. Aerobiologia. 2000; 16: 193–198.
17.
Burrell R. Immunotoxic reactions in the agricultural environment. Ann Agric Environ Med. 1995; 2: 11–20.
18.
Samson RA, Flannigan B, Flannigan ME. et al. Health Implications of Fungi in Indoor Environments. Elsevier, Amsterdam 1994.
19.
Górny RL, Reponen T, Willeke K, Schmechel D, Robin D, Robin E, Boissier M, et al. Fungal fragments as indoor air contaminants. Appl Environ Microbiol. 2002; 68: 3522–3531.
20.
Dutkiewicz J. Biological agents. In: Koradecka D (Ed). Handbook of Occupational Safety and Health, pp. 385–400. CRC Press, Taylor & Francis Group, Boca Raton 2010.
22.
Lopata AL, O’Hehir RE, Lehrer SB. Shellfish allergy. Clin Exp Allergy. 2010; 40(6): 850–858.
23.
Jeebhay MF, Robins TG, Lehrer SB, Lopata AL. Occupational seafood allergy: a review. Occup Environ Med. 2001; 58: 553–562.
24.
Griffin P, Crook B, Lacey J, Topping MD. Airborne scampi allergen and scampi peelers asthma. In: Griffiths WD (Ed): Aerosols: their Generation, Behaviour and Application. Aerosol Society Second Conference, pp. 347–352. The Aerosol Society, London 1988.
25.
Dutkiewicz J (Ed). Biological Hazards in Agriculture. Institute of Rural Heath, Lublin 1998 (in Polish).
26.
Bengoechea JA, Bamford CGG. SARS-CoV-2, bacterial co-infections, and AMR: the deadly trio in COVID-19? EMBO Mol Med. 2020; 12: e12560.
27.
Mapp C, Boschetto P, Miotto D, De Rosa E, Fabbri LM. Mechanisms of occupational asthma. Ann Allergy Asthma Immunol. 1999; 83: 645–664.
28.
Wild LG, Lopez M. Occupational asthma caused by high-molecular-weight substances. Immunol Allergy Clin North Am. 2003; 23: 235–250.
29.
Morais-Almeida M, Pité H, Aguiar R, Ansotegui I, Bousquet J. Asthma and the coronavirus disease 2019 pandemic: a literature review. Int Arch Allergy Immunol 2020; 181: 680–688.
30.
Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19). 2020. Available at: https://edubirdie.com/blog/peo.... Accessed October 1, 2020.
31.
Abrams EM, Jong GW, Connie L. Yang CL. Asthma and COVID-19. CMAJ 2020; 192:E551. doi: 10.1503/cmaj.200617.
32.
Jackson DJ, Busse WW, Bacharier LB, Kattan M, O’Connor GT, Wood RA, et al. Association of respiratory allergy, asthma and expression of the SARS-CoV-2 receptor. J Allergy Clin Immunol. 2020; 146(1): 203–206.e3. doi: 10.1016/j.jaci.2020.04.009.
33.
Lovinsky-Desir S, Deshpande DR, De A, Murray L, Stingone JA, Chan A, et al. Asthma among hospitalized patients with COVID-19 and related outcomes. J Allergy Clin Immunol. 2020; 6: S0091-6749(20)31100-3. doi: 10.1016/j.jaci.2020.07.026.
34.
Chhiba KD, Patel GB, Vu THT, Chen MM, Guo A, Kudlaty E. Prevalence and characterization of asthma in hospitalized and nonhospitalized patients with COVID-19. J Allergy Clin Immunol. 2020; 146: 307–314.
36.
Wang JY, Pawankar R, Tsai HJ, Wu SL, Kuo WS. COVID-19 and asthma, the good or the bad? Allergy 2020; 3: 10.1111/all.14480. doi: 10.1111/a l l.14 480.
37.
Peters MC, Sajuthi S, Deford P, Christenson S, Rios CL, Michael T. Montgomery MT, et al. COVID-19–related genes in sputum cells in asthma. Relationship to demographic features and corticosteroids. Am J Respir Crit Care Med. 2020; 202(1): 83–90.3.
38.
Sajuthi SP, DeFord P, Jackson ND, Montgomery MT, Everman JL, Rios CL, et al. Type 2 and interferon inflammation strongly regulate SARS-CoV-2 related gene expression in the airway epithelium. bioRxiv. 2020; 2020.04.09.034454. doi: 10.1101/2020.04.09.0344543.
39.
Radzikowska U, Ding M, Tan G, Zhakparov D, Peng Y, Wawrzyniak P, et al. Distribution of ACE2, CD147, CD26 and other SARS-CoV-2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID-19 risk factors. A l lerg y 2020. doi: 10.1111/A LL .14 429.
40.
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020; 584(7821): 430–436. doi: 10.1038/s41586-020-2521-4.
41.
Wark PAB, Ramsahai JM, Pathinayake P, Malik B, Bartlett NW. Respiratory viruses and asthma. Semin Respir Crit Care Med. 2018; 39(1): 45–55.
42.
Nogueira R, Melo N, Novais e Bastos H, Martins N, Delgado L, Morais A, Mota PC. Hypersensitivity pneumonitis: Antigen diversity and disease implications. Pulmonology. 2019, 25(2): 97–108.
43.
Selman M, Pardo A, King TE Jr. Hypersensitivity pneumonitis: insights in diagnosis and pathobiology. Am J Respir Crit Care Med. 2012; 186(4): 314 –324.
44.
Malmberg P, Rask-Andersen A, Höglund S, Kolmodin-Hedman B, Read Guernsey J. Incidence of organic dust toxic syndrome and allergic alveolitis in Swedish farmers. Int Arch Allergy Appl Immunol. 1988; 87(1): 47–54.
45.
Quirce S, Vandenplas O, Campo P, Cruz MJ, de Blay F, Koschel D, et al. Occupational hypersensitivity pneumonitis: an EAACI position paper. Allergy. 2016; 71(6): 765–779.
46.
Milanowski J, Dutkiewicz J, Potoczna H, Kuś L, Urbanowicz B. Allergic alveolitis among agricultural workers in eastern Poland: A study of twenty cases. Ann Agric Environ Med. 1998; 5: 31–43.
47.
Lemieszek M, Chilosi M, Golec M, Skórska C, Huaux F, Yakoub Y, et al. Mouse model of hypersensitivity pneumonitis after inhalation exposure to different microbial antigens associated with organic dusts. Ann Agric Environ Med. 2011; 18: 159–168.
48.
Lemieszek MK, Chilosi M, Golec M, Skórska C, Dinnyes A, Mashayekhi K, et al. Age influence on hypersensitivity pneumonitis induced in mice by exposure to Pantoea agglomerans. Inhal Toxicol. 2013, 25: 640–650.
49.
Dutkiewicz J, Mackiewicz B, Lemieszek MK, Golec M, Skórska C, Góra-Florek A, Milanowski J. Pantoea agglomerans: a mysterious bacterium of evil and good. Part. II. – Deleterious effects: Dust-borne endotoxins and allergens – focus on grain dust, other agricultural dusts and wood dust. Ann Agric Environ Med. 2016; 23: 6–29.
50.
Mackiewicz B, Dutkiewicz J, Siwiec J, Kucharczyk T, Siek E, Wójcik-Fatla A, et al. Acute hypersensitivity pneumonitis in woodworkers caused by inhalation of birch dust contaminated with Pantoea agglomerans and Microbacterium barkeri. Ann Agric Environ Med. 2019; 26(4): 644–655.
51.
Sanchez-Gonzalez MA, Moskowitz D, Issuree PD, Yatzkan G, Rizvi SA, Day K. A pathophysiological perspective on COVID-19’s lethal complication: from viremia to hypersensitivity pneumonitis-like immune dysregulation. Infect Chemother. 2020; 52(3): e31.
52.
Dakhama A, Hegele RG, Laflamme G, Israël-Assayag E, Cormier Y. Common respiratory viruses in lower airways of patients with acute hypersensitivity pneumonitis. Am J Respir Crit Care Med. 1999; 159: 1316 –1322.
53.
Cormier Y, Israël-Assayag E, Fournier M, Tremblay GM. Modulation of experimental hypersensitivity pneumonitis by Sendai virus. J Lab Clin Med. 1993; 121(5): 683–688.
54.
Cormier Y, Tremblay GM, Fournier M, Israël-Assayag E. Long-term viral enhancement of lung response to Saccharopolyspora rectivirgula. Am J Respir Crit Care Med. 1994; 149: 490–494.
55.
Cormier Y, Israël-Assayag E. The role of viruses in the pathogenesis of hypersensitivity pneumonitis. Curr Opin Pulm Med. 2000; 6(5): 420–423.
56.
Gudmundsson G, Monick MM, Hunninghake GW. Viral infection modulates expression of hypersensitivity pneumonitis. J Immunol. 1999; 162: 7397–7401.
57.
Kuś L. Allergic alveolitis after exposure to antigens occurring in grain dust in the light of own clinical and experimental investigations. Dissertation for the degree of Dr habil. Medical University, Lublin 1980 (in Polish).
58.
Lemieszek MK, Rzeski W, Golec M, Mackiewicz B, Zwoliński J, Dutkiewicz J, Milanowski J. Pantoea agglomerans chronic exposure induces epithelial-mesenchymal transition in human lung epithelial cells and mice lungs. Ecotoxicol Environ Saf. 2020: 194: 110416.
59.
Ochsner SA, McKenna NJ. A transcriptional regulatory atlas of coronavirus infection of human cells. BioRxiv Preprint. doi: https://doi.org/10.1101/2020.0.... Version posted April 27, 2020.
60.
Stewart CA, Gay CM, Ramkumar K, Cargill KR, Cardnell RJ, Nilsson MB, et al. SARS-CoV-2 infection induces EMT-like molecular changes, including ZEB1-mediated repression of the viral receptor ACE2, in lung cancer models. BioRxiv Preprint. doi: 10.1101/2020.05.28.1222912020 Version posted May 29, 2020.
61.
Song YG, Shin HS. COVID-19, a clinical syndrome manifesting as hypersensitivity pneumonitis. Infect Chemother. 2020; 52(1): 110–112.
62.
Von Essen S, Robbins RA, Thompson AB, Rennard SI. Organic dust toxic syndrome: an acute febrile reaction to organic dust exposure distinct from hypersensitivity pneumonitis. J Toxicol Clin Toxicol. 1990; 28(4): 389–420.
63.
Petruk G, Puthia M, Petrlova J, Strömdahl A-C, Kjellström S, Schmidtchen A. SARS-CoV-2 Spike protein binds to bacterial lipopolysaccharide and boosts proinflammatory activity. bioRxiv DOI: https://doi.org/10.1101/2020.0....
64.
Nain N, Hinder F, Gong JH, Schmidt A, Bender A, Sprenger H, Gemsa D. Tumor necrosis factor-alpha production of influenza A virus-infected macrophages and potentiating effect of lipopolysaccharides. J Immunol. 1990: 145(6): 1921–1928.
65.
Dutkiewicz J, Skórska C, Burrell R, Szuster-Ciesielska A, Sitkowska J. Immunostimulative effects of repeated inhalation exposure to microvesicle-bound endotoxin of Pantoea agglomerans. Ann Agric Environ Med. 2005; 12: 289–294.
66.
Mueller M, Lindner B, Kusumoto S, Fukase K, Schromm AB, Seydel U. Aggregates are the biologically active units of endotoxin. J Biol Chem 2004; 279(25): 26307–26313.
67.
Yang J, Kim Y-K, Kang TS, Jee Y-K, Kim Y-Y. Importance of indoor dust biological ultrafine particles in the pathogenesis of chronic inflammatory lung diseases. Environ Health Toxicol. 2017; 32: e2017021.
68.
Yang J, Kim EK, Park HJ, McDowell A, Kim Y-K. The impact of bacteria-derived ultrafine dust particles on pulmonary diseases. Exp Molec Med 2020; 52: 338–347.
69.
Kim YY, Joh JS, Lee JY. Importance of microbial extracellular vesicle in the pathogenesis of asthma and chronic obstructive pulmonary disease and its diagnostic potential. Asia Pac Allergy. 2020; 10(3): e25.
70.
Rylander R. Bacterial toxins and etiology of byssionosis. Chest 1981; Suppl. 79: 34S-38S.
71.
Rylander R. The role of endotoxin for reactions after exposure to cotton dust. Am J Ind Med. 1987; 12: 687–697.
72.
Menon B, Mrigpuri P, Tiwari M, Raj P. Diffuse lung disease caused by cotton dust exposure. J Lung Pulm Respir Res. 2018; 5(6): 176‒178.
73.
Gangan SP. ‘Textile workers’ lung diseases make them vulnerable to Covid’. Hindustan Times, Mumbai, Jul 09, 2020.
74.
Sorenson WG. Mycotoxins. Toxic metabolites of fungi. In: Murphy JW, et al. (Eds): Fungal Infection and Immune Response, pp. 469–491. New York, Plenum Press 1993.
75.
Górny R. L. (Ed). Water Damage to Buildings and Their Microbiological Corrosion. Causes, Risks, Prevention and Remediation. Central Institute for Labour Protection, Warsaw 2010.
76.
Rylander R, Persson K, Goto H, Yuasa K, Tanaka S. Airborne ?-1,3-glucan may be related to symptoms in sick buildings. Indoor Environ. 1992; 1: 263–267.
77.
Hosseini MR, Reza Fouladi-Fard R, Aali R. COVID-19 pandemic and sick building syndrome. Indoor Built Environ. 2020; 0(0): 1–3. doi: 10.1177/1420326X20935644.
79.
Eisen D. Employee presenteeism and occupational acquisition of COVID-19. Med J Aust. 2020; 13(3): 140–140.
80.
Ministry of Health, Poland. Official data on COVID-19 among health care workers in Poland between 4.03.2020–2.11.2020. Announced: 3.11.2020. https:\www.medonet.pl (in Polish).
81.
Morawska L, Tang JW, Bahnfleth W, Bluyssend PM, Boerstrae A, Buonanno G, et al. How can airborne transmission of COVID-19 indoors be minimised? Environ Internat. 2020; 142: 105832.
82.
National Center for Farmworkers Health, Inc. COVID-19 in Rural America: Impact on Farms & Agricultural Workers. Farmworker Health Factsheet, October 1, 2020.
83.
Tuirán R., Roberts N. Farmworkers are among those at highest risk for COVID-19, studies show. PBS, Frontline July 21, 2020. https://www.pbs.org/wgbh/front....
84.
Zhong Z-F, Huang J, Yang X, Peng J-L, Zhang X-Y, Hu Y, et al. Epidemiological and clinical characteristics of COVID-19 patients in Hengyang, Hunan Province, China. World J Clin Cases. 2020; 8(12): 2554–2565.
85.
Oreshkova N, Molenaar RJ, Vreman S, Harders F, Oude Munnink BB, Hakze-van der Honing RW, et al. SARS-CoV-2 infection in farmed minks, the Netherlands, April and May 2020. Euro Surveill.2020; 25(23): pii=2001005. https://doi.org/10.2807/1560–7....
86.
Enserink M. Coronavirus rips through Dutch mink farms, triggering culls. Public concerns rise as two workers catch the disease. Science 2020; 368(6496): 1169. doi: 10.1126/science.368.6496.1169.
87.
Anonymous. Netherlands terminates mink farming following COVID-19 outbreaks. CGTN, 03-Jul-2020 (press note).
88.
Barsoe T, Heinrich M (Reuters Staff ). Denmark to cull up to one million mink due to risk of coronavirus contagion. Reuters, Environment, October 2, 2020 (press note).
89.
Dyal JW, Grant MP, Broadwater K, Bjork A, Waltenburg MA, Gibbins JD, et al. COVID-19 among workers in meat and poultry processing facilities — 19 States, April 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(18 557): 557–561.
90.
Middleton J, Reintjes R, Lopes H. Meat plants—a new front line in the COVID-19 pandemic. These businesses failed in their duty to workers and the wider public health. BMJ 2020; 370: m2716. doi: 10.1136/bmj.m2716.
91.
Halliday J. Over 450 cases of COVID-19 reported at food factories in England and Wales. Guardian 2020, Jun 25 (press note), https://www.theguardian.com/uk....
92.
Anonymous. A Wuhan shrimp seller identified as coronavirus ‘patient zero’. The Economic Times, Word News, March 30, 2020 (press note).
93.
Bertelsen R, Svanes Ø, Hollund BE, Madsen AM, Sigsgaard T, Aasen T, Svanes C. Organic dust toxic syndrome caused by occupational exposure to shrimpshell powder. Eur Respir J. 2015; 46: PA4098. doi: 10.1183/13993003.congress-2015.PA4098.
94.
Craze M. Ecuador shrimp capital is coronavirus epicenter. Undercurrent News – seafood business news from beneath the surface, April 20, 2020 (press note). https://www.undercurrentnews.c....
95.
Walsh M, Simin W. The mystery link between China’s Covid-19 outbreaks and seafood. CX Daily Briefing, Caixin, Jul 28, 2020 (press note).
96.
Anonymous, COVID-19 outbreaks in Wuhan, Beijing and Dalian share certain similarities. CGTN, Health 30-Jul-2020 (press note).
97.
Nishiura H, Linton NM, Akhmetzhanov AR. Initial cluster of novel coronavirus (2019-nCoV) infections in Wuhan, China is consistent with substantial human-to-human transmission. J Clin Med. 2020; 9: 488. doi: 10.3390/jcm9020488.
98.
Cowley JA. Nidoviruses of Fish and Crustaceans. In: Aquaculture Virology. Elsevier Inc. 2016, 443–472. http://dx.doi.org/10.1016/B978....
99.
Ziebuhr J, Bayer S, Cowley JA, Gorbalenya AE. The 3C-like proteinase of an invertebrate Nidovirus links Coronavirus and Potyvirus homologs. J Virol. 2003; 77(2): 1415–1426.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.