Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Working environment of health care professionals – focus on occupational stress
1
Faculty of Health Sciences, Klaipeda University, Klaipeda, Lithuania
2
University Hospital, Klaipeda, Lithuania
3
Faculty of Marine Technology and Natural Sciences, Klaipeda University, Klaipeda, Lithuania
4
Department of Public Health, Medical University of Bialystok, Bialystok, Poland
Corresponding author
Ann Agric Environ Med. 2023;30(4):721-728
KEYWORDS
occupational stresshealthcare workersworking environmentstress managementhealthcare professionalsstress prevention
TOPICS
ABSTRACT
Introduction and objective:
Healthcare professionals most often encounter occupational stress. The aim of the study was to investigate the working environment of health care professionals with the focus on expression of occupational stress, and oversee the possibilities of stress management and prevention.
Material and methods:
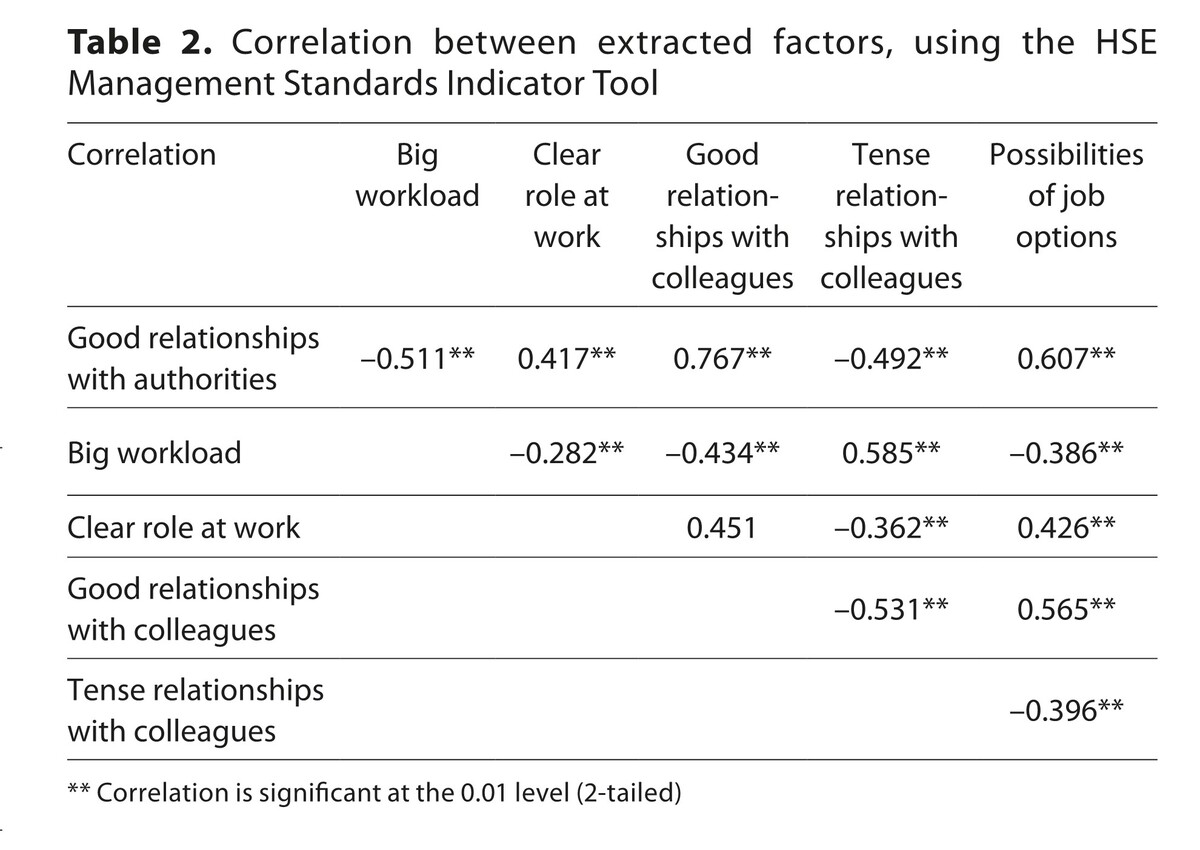
326 representatives from five different healthcare institutions were surveyed in Siauliai city, Lithuania. The validated questionnaires HSE Management Standards Indicator Tool and the SF-36 questionnaire were used.
Results:
The study revealed that the most important organizational factors were lack of communication, inappropriate relations with authorities and colleagues, big workload and long working hours, quick decision-making, and manifestations of mobbing. Financial support was reported as one of the main motivators in stress management. The most frequent individual factors were emotional relations with patients and their relatives. The healthcare professionals who experienced stress at work more often felt aches that disturbed their work routine, and their health interfered more their ordinary social activities. The main stress prevention measures are involvement of employees in decision-making, annual interviews with authorities, education, assurance of a safe work environment, and elimination of manifestations of mobbing.
Conclusions:
More attention must be paid to occupational stress management. It appeared that there is a lack of knowledge by institutions about the models of occupational stress management and internal stress management policy of organization. Therefore, this stimulates the search for measures that could help to change the situation.
Healthcare professionals most often encounter occupational stress. The aim of the study was to investigate the working environment of health care professionals with the focus on expression of occupational stress, and oversee the possibilities of stress management and prevention.
Material and methods:
326 representatives from five different healthcare institutions were surveyed in Siauliai city, Lithuania. The validated questionnaires HSE Management Standards Indicator Tool and the SF-36 questionnaire were used.
Results:
The study revealed that the most important organizational factors were lack of communication, inappropriate relations with authorities and colleagues, big workload and long working hours, quick decision-making, and manifestations of mobbing. Financial support was reported as one of the main motivators in stress management. The most frequent individual factors were emotional relations with patients and their relatives. The healthcare professionals who experienced stress at work more often felt aches that disturbed their work routine, and their health interfered more their ordinary social activities. The main stress prevention measures are involvement of employees in decision-making, annual interviews with authorities, education, assurance of a safe work environment, and elimination of manifestations of mobbing.
Conclusions:
More attention must be paid to occupational stress management. It appeared that there is a lack of knowledge by institutions about the models of occupational stress management and internal stress management policy of organization. Therefore, this stimulates the search for measures that could help to change the situation.
REFERENCES (49)
1.
Ma Y, Faraz NA, Ahmed F, et al. Curbing nurses’ burnout during COVID-19: The roles of servant leadership and psychological safety. J Nurs Manag. 2021;29(8):2383–2391. doi:10.1111/jonm.
2.
Wang H, Liu Y, Hu K, et al. Healthcare workers’ stress when caring for COVID-19 patients: An altruistic perspective. Nurs Ethics. 2020;27(7):1490–1500. doi:10.1177/0969733020934146.
3.
Makara-Studzińska M, Wontorczyk A, Izydorczyk B. Stress and occupational burnout in a population of Polish doctors – Organizational-professional and non-professional-social predictors. Ann Agric Environ Med. 2020;27(3):456–468. doi:10.26444/aaem/110846.
4.
Havermans BM, Brouwers EPM, Hoek RJA, Anema JR, van der Beek AJ, Boot CRL. Work stress prevention needs of employees and supervisors. BMC Public Health. 2018;18(1):642. doi:10.1186/s12889-018-5535-1.
5.
Goncalves A, Fontes, L, Simaes C, et al. Stress and burnout in health professionals. Occup Environ Saf Health. 2019;202,563–571.
6.
Kwiecień-Jaguś K, Mędrzycka-Dąbrowska W, Chamienia A, et al. Stress factors vs. job satisfaction among nursing staff in the Pomeranian Province (Poland) and the Vilnius Region (Lithuania). Ann Agric Environ Med. 2018;25(4):616–624. doi:10.26444/aaem/75801.
7.
Burton A, Burgess C, Dean S, Koutsopoulou GZ, et al. How Effective are Mindfulness-Based Interventions for Reducing Stress Among Healthcare Professionals? A Systematic Review and Meta-Analysis. Stress Health. 2017;33(1):3–13. doi:10.1002/smi.2673.
8.
Li Y, Scherer N, Felix L, et al. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS One. 2021;16(3):e0246454. doi:10.1371/journal.pone.0246454.
9.
Bruschini M, Carli A, Burla F. Burnout and work-related stress in Italian rehabilitation professionals: A comparison of physiotherapists, speech therapists and occupational therapists. Work. 2018;59(1):121–129. doi:10.3233/WOR-172657.
10.
Hodkinson A, Zhou A, Johnson J, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. 2022;378:e070442. doi:10.1136/bmj-2022-070442.
11.
Sarafis P, Rousaki E, Tsounis A, et al. The impact of occupational stress on nurses’ caring behaviors and their health related quality of life. BMC Nurs. 2016;15:56. doi:10.1186/s12912-016-0178-y.
12.
Moreno Fortes A, Tian L, Huebner ES. Occupational Stress and Employees Complete Mental Health: A Cross-Cultural Empirical Study. Int J Environ Res Public Health. 2020;17(10):3629. doi:10.3390/ijerph17103629.
13.
Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi:10.1016/j.bbi.2020.05.026. Erratum in: Brain Behav Immun. 2021;92:247.
14.
Caruso R, Toffanin T, Folesani F, et al. Violence Against Physicians in the Workplace: Trends, Causes, Consequences, and Strategies for Intervention. Curr Psychiatry Rep. 2022;24(12):911–924. doi:10.1007/s11920-022-01398-1.
15.
Mento C, Silvestri MC, Bruno A, et al. Workplace violence against healthcare professionals: A systematic review. Aggression and violent behaviour. 2020;51,101381. doi:10.1016/j.avb.2020.101381.
16.
Hawton K, Agerbo E, Simkin S, et al. Risk of suicide in medical and related occupational groups: a national study based on Danish case population-based registers. J Affect Disord. 2011;134(1–3):320–6. doi:10.1016/j.jad.2011.05.044.
17.
Joseph B, Joseph M. The health of the healthcare workers. Indian J Occup Environ Med. 2016;20(2):71–72. doi:10.4103/0019-5278.197518.
18.
Cocchiara RA, Peruzzo M, Mannocci A, et al. The Use of Yoga to Manage Stress and Burnout in Healthcare Workers: A Systematic Review. J Clin Med. 2019;8(3):284. doi:10.3390/jcm8030284.
19.
Mayo AT, Woolley AW. Teamwork in Health Care: Maximizing Collective Intelligence via Inclusive Collaboration and Open Communication. AMA J Ethics. 2016;18(9):933–40. doi:10.1001/journalofethics.2016.18.9.stas2-1609.
20.
Ungar P, Schindler AK, Polujanski S, et al. Online programs to strengthen the mental health of medical students: A systematic review of the literature. Med Educ Online. 2022;27(1):2082909. doi:10.1080/10872981.2022.2082909.
21.
Ng R, Chahine S, Lanting B, et al. Unpacking the Literature on Stress and Resiliency: A Narrative Review Focused on Learners in the Operating Room. J Surg Educ. 2019;76(2):343–353. doi:10.1016/j.jsurg.2018.07.025.
22.
Lu DW, Zhan T, Bilimoria KY, et al. Workplace mistreatment, career choice regret, and burnout in emergency medicine residency training in the United States. Ann Emerg Med. 2023;81(6):706–714. doi:10.1016/j.annemergmed.2022.10.015.
23.
Barten DG, Klokman VW, Cleef S, et al. When disasters strike the emergency department: a case series and narrative review. Int J Emerg Med. 2021;14(1):49. doi:10.1186/s12245-021-00372-7.
24.
Vizheh M, Qorbani M, Arzaghi SM, et al. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J Diabetes Metab Disord. 2020;19(2):1967–1978. doi:10.1007/s40200-020-00643-9.
25.
Umbetkulova S, Kanderzhanova A, Foster F, et al. Mental Health Changes in Healthcare Workers DURING COVID-19 Pandemic: A Systematic REVIEW of Longitudinal Studies. Eval Health Prof. 2023:1632787231165076. doi:10.1177/01632787231165076.
26.
Stodolska A, Wójcik G, Barańska I, et al. Prevalence of burnout among healthcare professionals during the COVID-19 pandemic and associated factors – a scoping review. Int J Occup Med Environ Health. 2023;36(1):21–58. doi:10.13075/ijomeh.1896.02007.
27.
Lai J, Ma S, Wang Y, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi:10.1001/jamanetworkopen.2020.3976.
28.
Nienhaus A, Kesavachandran C, Wendeler D, et al. Infectious diseases in healthcare workers – an analysis of the standardised data set of a German compensation board. J Occup Med Toxicol. 2012;7(1):8. doi:10.1186/1745-6673-7-8.
29.
Pataka A, Kotoulas S, Tzinas A, et al. Sleep Disorders and Mental Stress of Healthcare Workers during the Two First Waves of COVID-19 Pandemic: Separate Analysis for Primary Care. Healthcare (Basel). 2022;10(8):1395. doi:10.3390/healthcare10081395.
30.
Hämmig O. Work- and stress-related musculoskeletal and sleep disorders among health professionals: a cross-sectional study in a hospital setting in Switzerland. BMC Musculoskelet Disord. 2020;21(1):319. doi:10.1186/s12891-020-03327-w.
31.
Ezenwaji IO, Eseadi C, Okide CC, et al. Work-related stress, burnout, and related sociodemographic factors among nurses: Implications for administrators, research, and policy. Medicine (Baltimore). 2019;98(3):e13889. doi:10.1097/MD.0000000000013889.
32.
Coplan B, McCall TC, Smith N, et al. Burnout, job satisfaction, and stress levels of PAs. JAAPA. 2018;31(9):42–46. doi:10.1097/01.JAA.0000544305.38577.84.
33.
Baird KM, Tung A, Yu Y. Employee organizational commitment and hospital performance. Health Care Manage Rev. 2019;44(3):206–215. doi:10.1097/HMR.0000000000000181.
34.
Teoh KRH, Hassard J, Cox T. Individual and organizational psychosocial predictors of hospital doctors’ work-related well-being: A multilevel and moderation perspective. Health Care Manage Rev. 2020;45(2):162–172. doi:10.1097/HMR.0000000000000207.
35.
Berberoglu A. Impact of organizational climate on organizational commitment and perceived organizational performance: empirical evidence from public hospitals. BMC Health Serv Res. 2018;18(1):399. doi:10.1186/s12913-018-3149-z.
36.
Kuodyte V, Pajarskiene B. Psychometric properties of the Lithuanian version of the HSE Stress Indicator Tool. Public Health. 2017;4(79):66–73.
37.
Zhang Y, Qu B, Lun SS, et al. The 36-item short form health survey: reliability and validity in Chinese medical students. Int J Med Sci. 2012;9(7):521–6. doi:10.7150/ijms.4503.
38.
Copanitsanou P, Fotos N, Brokalaki H. Effects of work environment on patient and nurse outcomes. Br J Nurs. 2017;26(3):172–176. doi:10.12968/bjon.2017.26.3.172.
39.
Zheng R, Lee SF, Bloomer MJ. How nurses cope with patient death: A systematic review and qualitative meta-synthesis. J Clin Nurs. 2018;27(1–2):e39-e49. doi:10.1111/jocn.13975.
40.
Wang C, Huang L, Li J, et al. Relationship between psychosocial working conditions, stress perception, and needle-stick injury among healthcare workers in Shanghai. BMC Public Health. 2019;19(1):874. doi:10.1186/s12889-019-7181-7.
41.
Andela M, Truchot D, Van der Doef M. Job stressors and burnout in hospitals: The mediating role of emotional dissonance. Int J Stress Management. 2016;23(3):298–317. doi:10.1037/str0000013.
42.
Montgomery A, Panagopoulou E, Esmail A, et al. Burnout in healthcare: the case for organisational change. BMJ. 2019;366:l4774. doi:10.1136/bmj.l4774.
43.
Olvera Alvarez HA, Provencio-Vasquez E, Slavich GM, et al. Stress and Health in Nursing Students: The Nurse Engagement and Wellness Study. Nurs Res. 2019;68(6):453–463. doi:10.1097/NNR.0000000000000383.
44.
Cordioli DFC, Cordioli Junior JR, Gazetta CE, et al. Occupational stress and engagement in primary health care workers. Rev Bras Enferm. 2019;72(6):1580–1587. doi:10.1590/0034-7167-2018-0681.
45.
Stoewen DL. Wellness at work: Building healthy workplaces. Can Vet J. 2016;57(11):1188–1190.
46.
Karasek RA. Jr. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979:285–308.
47.
Siegrist J, Starke S, Chandola T, et al. The measurement of effort-reward imbalance at work: European comparisons. Soc Sci Med. 2004;58:1483–1499. doi:10.1016/S0277-9536(03)00351-4.
48.
Notelaers G, Törnroos M, Salin D. Effort-Reward Imbalance: A Risk Factor for Exposure to Workplace Bullying. Front Psychol. 2019;10:386. doi:10.3389/fpsyg.2019.00386.
49.
Eslami Akbar R, Elahi N, Mohammadi E, et al. What Strategies Do the Nurses Apply to Cope With Job Stress?: A Qualitative Study. Glob J Health Sci. 2015;8(6):55–64. doi:10.5539/gjhs.v8n6p55.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.