Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Comparing results of three measurement techniques used to determine the size of oropharyngeal airway in adults
1
Department of Emergency Medicine and Disaster Medicine, Medical University of Lodz, Poland
Corresponding author
Ann Agric Environ Med. 2023;30(4):715-720
KEYWORDS
airway managementventilationairway obstructionrespiratory therapyemergency medicineoropharyngealairwaymedical device
TOPICS
ABSTRACT
Introduction and objective:
The oropharyngeal airway, also known as the Guedel airway, is a crucial medical device used for over a century as a basic way to maintain a patient’s airway open and secure. Although it is easy to use, this can be misleading as incorrect sizing can lead to injuries, bleeding, laryngospasm, and potentially fatal complications. This study aims to compare three techniques for selecting the appropriate oropharyngeal airway size using craniofacial anatomical landmarks.
Material and methods:
Three facial distances were measured, each one according to the techniques described in the scientific sources. For greater reliability of the test, measurements were made sequentially with two different methods.
Results:
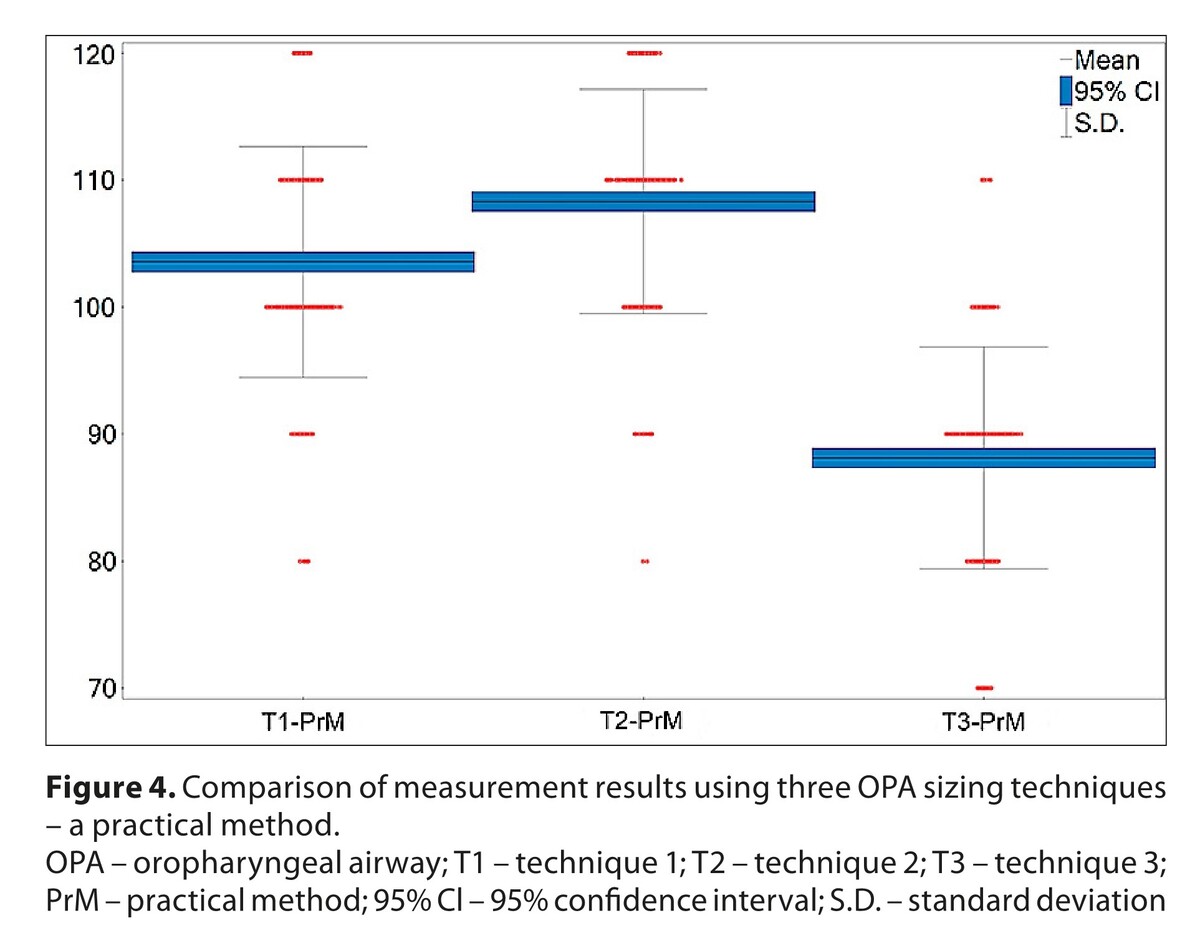
The study included over 500 participants. Depending on the measurement technique used, different results of average lengths and thus approximate sizes of oropharyngeal airway were obtained. This indicated that depending on which technique is used for measuring purposes, differences in the size of the oropharyngeal airway can be up to 2–3 cm, with a high degree of statistical significance.
Conclusions:
Using different craniofacial anatomical landmarks to select the size of the oropharyngeal airway can yield significantly varied results for the same adult patient, thus posing a potentially fatal threat. To ensure effective and safe airway management, proper ventilation and oxygenation, it is recommended to follow the ISA (Initial Size Approximation) approach when choosing the oropharyngeal airway size in medical education, training, and clinical settings. Further research is needed to explore this matter, also in different populations
The oropharyngeal airway, also known as the Guedel airway, is a crucial medical device used for over a century as a basic way to maintain a patient’s airway open and secure. Although it is easy to use, this can be misleading as incorrect sizing can lead to injuries, bleeding, laryngospasm, and potentially fatal complications. This study aims to compare three techniques for selecting the appropriate oropharyngeal airway size using craniofacial anatomical landmarks.
Material and methods:
Three facial distances were measured, each one according to the techniques described in the scientific sources. For greater reliability of the test, measurements were made sequentially with two different methods.
Results:
The study included over 500 participants. Depending on the measurement technique used, different results of average lengths and thus approximate sizes of oropharyngeal airway were obtained. This indicated that depending on which technique is used for measuring purposes, differences in the size of the oropharyngeal airway can be up to 2–3 cm, with a high degree of statistical significance.
Conclusions:
Using different craniofacial anatomical landmarks to select the size of the oropharyngeal airway can yield significantly varied results for the same adult patient, thus posing a potentially fatal threat. To ensure effective and safe airway management, proper ventilation and oxygenation, it is recommended to follow the ISA (Initial Size Approximation) approach when choosing the oropharyngeal airway size in medical education, training, and clinical settings. Further research is needed to explore this matter, also in different populations
REFERENCES (29)
1.
Hewitt FW. An artificial “air-way” for use during anaesthetisation. The Lancet. 1908;171(4407):490–491. https://doi.org/10.1016/S0140-....
2.
Haridas RP. The Hewitt airway – the first known artificial oral ‘air-way’ 101 years since its description. Anaesthesia. 2009;64(4):435–438. https://doi.org/10.1111/j.1365....
3.
Guedel AE. A nontraumatic pharyngeal airway. JAMA. 1933;100(23):1862–1862. https://doi.org/10.1001/jama.1....
4.
Baskett TF. Arthur Guedel and the oropharyngeal airway. Resuscitation. 2004;63(1):3–5. https://doi.org/10.1016/j.resu....
5.
Kim HJ, Kim SH, Min JY, Park WK. Determination of the appropriate oropharyngeal airway size in adults: Assessment using ventilation and an endoscopic view. Am J Emerg Med. 2017;35(10):1430–1434. https://doi.org/10.1016/j.ajem....
6.
González RR, García JT, Lomas A. Importance of size of the Guedel in the patency of the airway during MRI in children. Science Postprint. 2013;1(1):6–6. https://doi.org/10.14340/spp.2....
7.
Castro D, Freeman LA. Oropharyngeal Airway. In: StatPearls. Treasure Island (FL) StatPearls Publishing; 2022.
8.
Regulation of the Minister of Health of 19 March 2007 on the qualified first aid course. Journal of Laws of 2007; No. 60, item 408 as amended.
9.
Marsh AM, Nunn JF, Taylor SJ, et al. Airway obstruction associated with the use of the Guedel airway. Br J Anaesth. 1991;67(5):517–523. https://doi.org/ https://doi.org/10.1093/bja/67....
10.
Kumar N, Gupta BK, Dubey PK, et al. Palatal pressure necrosis due to inappropriate size of Guedel’s airway?. Indian J Anaesth. 2016;60(2):150–150. https://doi.org/10.4103/0019-5....
11.
Bhardwaj A, Bhagat H. Necrosis of lower lip due to Guedel’s airway in a case of head injury. JNACC. 2014;1(3):219–220. https://doi.org/10.4103/2348-0....
12.
Gusti V, Vaghadia H. Hybrid nasopharyngeal and oropharyngeal airway for improving upper airway and capnography in sedated patients. Can J Emerg Med. 2021;23(3):416–417. https://doi.org/10.1007/s43678....
13.
Elmer JE, Walls RM, Page RL. ACLS: Advanced Cardiac Life Support Provider Manual. 2020 ed. American Heart Association; 2020.
14.
Lott C, Carmona F. ALS: Advanced Life Support Course Manual, European Resuscitation Council Guidelines. 2021 ed. Resuscitation Council; 2021.
15.
Alson RL, Han K, Campell JE. ITLS: International Trauma Life Support for Emergency Care Providers. 9th ed. Pearson North America; 2019.
16.
National Association of Emergency Medical Technicians. PHTLS: Prehospital Trauma Life Support. 9th ed. Jones & Bartlett Learning; 2018.
17.
Kim HJ, Kim SH, Min NH, et al. Determination of the appropriate sizes of oropharyngeal airways in adults: correlation with external facial measurements: A randomised crossover study. Eur J Anaesthesiol. 2016;33(12):936–942. https://doi.org/10.1097/EJA.00....
18.
Ho AK. Should Oropharyngeal Airways Be Included With Public Automated External Defibrillators?. Circulation. 2018;138(16):1620–1622. https://doi.org/10.1161/CIRCUL....
19.
Nemeth M, Ernst M, Asendorf T, et al. Guedel oropharyngeal airway: The validation of facial landmark-distances to estimate sizing in children – Visualisation by magnetic resonance imaging (GUEDEL-I):A prospective observational study. Resuscitation. 2023;184:109702. https://doi.org/10.1016/j.resu....
20.
Jain S, Nazir N, Khan RM, et al. A prospective randomized control study comparing classic laryngeal mask airway with Guedel’s airway for tracheal tube exchange and smooth extubation. Anesth Essays Res. 2016;10(3):552–556. https://doi.org/10.4103/0259-1....
21.
Soar J, Böttiger BW, Carli P, et al. European Resuscitation Council Guidelines 2021: Adult advanced life support [published correction appears in Resuscitation. 2021;167:105–106]. Resuscitation. 2021;161(1):115–151. https://doi.org/10.1016/j.resu....
22.
Panchal AR, Bartos JA, Cabanas JG, et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16_suppl_2):366–468. https://doi.org/10.1161/CIR.00....
23.
Greif R, Lockey A, Breckwoldt J. et al. European Resuscitation Council Guidelines 2021: Education for resuscitation. Resuscitation. 2021;161(1):388–407. https://doi.org/10.1016/j.resu....
24.
Greif R, Bhanji F, Bigham BL, et al. Education, Implementation, and Teams: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation. 2020;156(1):188–239. https://doi.org/10.1016/j.resu....
25.
Eberhard KE, Linderoth G, Gregers MCT, et al. Impact of dispatcher-assisted cardiopulmonary resuscitation on neurologically intact survival in out-of-hospital cardiac arrest: a systematic review. Scand J Trauma Resusc Emerg Med. 2021;29(1):70–70. https://doi.org/10.1186/s13049....
26.
Gräsner JT, Herlitz J, Tjelmeland IBM, et al. European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe. Resuscitation. 2021;161(1):61–79. https://doi.org/10.1016/j.resu....
27.
González-Salvado V, Rodríguez-Ruiz E, Abelairas-Gómez C, et al. Training adult laypeople in basic life support. A systematic review. Rev Esp Cardiol. 2020;73(1):53–68. https://doi.org/10.1016/j.rec.....
28.
Shibahashi K, Sugiyama K, Kuwahara Y, et al. Private residence as a location of cardiac arrest may have a deleterious effect on the outcomes of out-of-hospital cardiac arrest in patients with an initial non-shockable cardiac rhythm: A multicentre retrospective cohort study. Resuscitation. 2020;150:80–89. https://doi.org/10.1016/j.resu....
29.
Bylow H, Rawshani A, Claesson A, et al. Characteristics and outcome after out-of-hospital cardiac arrest with the emphasis on workplaces: an observational study from the Swedish Registry of Cardiopulmonary Resuscitation. Resusc Plus. 2021;5:100090. https://doi.org/10.1016/j.resp....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.