Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Vitamin D and upper respiratory tract infections in young active males exposed to cold environments
1
Central Institute For Labour Protection-National Research Institute, Warsaw, Poland
2
University of North Dakota, Grand Forks, USA
3
Institute of Sport – National Research Institute, Warsaw, Poland
4
Józef Piłsudski University of Physical Education, Warsaw, Poland
5
Collegium Medicum, University of Zielona Góra, Poland
Corresponding author
Joanna Orysiak
Central Institute For Labour Protection-National Research Institute, Czerniakowska 16, 00-701, Warsaw, Poland
Central Institute For Labour Protection-National Research Institute, Czerniakowska 16, 00-701, Warsaw, Poland
Ann Agric Environ Med. 2021;28(3):446-451
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Performing indoor and outdoor work in cold environments may result in various adverse effects on human health and may lead to increased risk of respiratory infection. The aim of this study was to determine the relation of vitamin D status to secretory immunoglobulin A concentration, leucocyte counts, cytokine concentrations and incidence of upper respiratory tract infection (URTI) episodes in young active men during an autumn-winter period.
Material and methods:
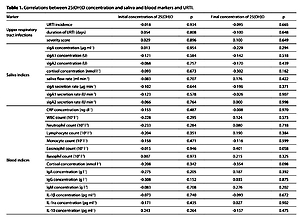
The effect of work in a cold microclimate was studied among 23 young active male ice hockey players during a 19-week study period. Blood and saliva samples were collected 7 times during the study period. Incidence of URTI was evaluated using WURSS 21. White blood cell, neutrophil, lymphocyte, monocyte, eosinophil and basophil counts, concentrations of 25(OH)D, C-reactive protein, cortisol, IL-1ra, IL-10, IL-1β and immunoglobulins A, M and G, were determined in the blood. Secretory immunoglobulin A, A1 and A2 and cortisol were analysed in saliva. Spearman’s correlations were used to evaluate relationships between initial or final 25(OH)D concentration and URTI incidence, as well as the immune and endocrine markers. Differences in URTI episodes, immune and endocrine parameters between sufficient ( ≥20 ng·ml -1) and deficient (<20 ng ·ml -1) vitamin D status groups were compared with the Mann-Whitney test.
Results:
There were no statistically significant correlations between mucosal and blood markers or URTI incidence and initial and final 25(OH)D concentrations. Immune, endocrine and URTI variables did not differ between deficient and sufficient vitamin D status groups.
Conclusions:
25(OH)D concentration has no impact on mucosal and systemic immunity, nor on URTI episodes.
Performing indoor and outdoor work in cold environments may result in various adverse effects on human health and may lead to increased risk of respiratory infection. The aim of this study was to determine the relation of vitamin D status to secretory immunoglobulin A concentration, leucocyte counts, cytokine concentrations and incidence of upper respiratory tract infection (URTI) episodes in young active men during an autumn-winter period.
Material and methods:
The effect of work in a cold microclimate was studied among 23 young active male ice hockey players during a 19-week study period. Blood and saliva samples were collected 7 times during the study period. Incidence of URTI was evaluated using WURSS 21. White blood cell, neutrophil, lymphocyte, monocyte, eosinophil and basophil counts, concentrations of 25(OH)D, C-reactive protein, cortisol, IL-1ra, IL-10, IL-1β and immunoglobulins A, M and G, were determined in the blood. Secretory immunoglobulin A, A1 and A2 and cortisol were analysed in saliva. Spearman’s correlations were used to evaluate relationships between initial or final 25(OH)D concentration and URTI incidence, as well as the immune and endocrine markers. Differences in URTI episodes, immune and endocrine parameters between sufficient ( ≥20 ng·ml -1) and deficient (<20 ng ·ml -1) vitamin D status groups were compared with the Mann-Whitney test.
Results:
There were no statistically significant correlations between mucosal and blood markers or URTI incidence and initial and final 25(OH)D concentrations. Immune, endocrine and URTI variables did not differ between deficient and sufficient vitamin D status groups.
Conclusions:
25(OH)D concentration has no impact on mucosal and systemic immunity, nor on URTI episodes.
ACKNOWLEDGEMENTS
The authors would like to thank the ice hockey players,
their parents, coaches and teachers who participated in the
study. The study was financially supported by the Ministry
of Science and Higher Education Republic of Poland (Grant
Nos. RSA2 006 52; 102.05).
REFERENCES (45)
1.
Mäkinen TM, Hassi J. Health problems in cold work. Ind Health. 2009; 47(3): 207–220.
2.
Cheung SS, Lee JK, Oksa J. Thermal stress, human performance, and physical employment standards. Appl Physiol Nutr Metab. 2016; 41(6 Suppl 2): S148–164. doi: 10.1139/apnm-2015-0518.
3.
Mohammadi D, Zare Zadeh M, Javad Zare Sakhvidi M. Short-term exposure to extreme temperature and risk of hospital admission due to cardiovascular diseases. Int J Environ Health Res. 2019. doi: 10.1080/09603123.2019.1663496.
4.
Luan G, Yin P, Wang L, et al. Association between ambient temperature and chronic obstructive pulmonary disease: a population-based study of the years of life lost. Int J Environ Health Res. 2019; 29(3): 246–254. doi: 10.1080/09603123.2018.1533533.
5.
Pecyna A, Buczaj A, Lachowski S, et al. Occupational hazards in opinions of forestry employees in Poland. Ann Agric Environ Med. 2019; 26(2): 242–248. doi: 10.26444/aaem/106246.
6.
LaVoy EC, McFarlin BK, Simpson RJ. Immune responses to exercising in a cold environment. Wilderness Environ Med. 2011; 22(4): 343–351. doi: 10.1016/j.wem.2011.08.005.
7.
Wang Y, Zhan S, Liu Y, et al. Occupational hazards tohealth of port workers, Int J Occup Saf Ergon. 2017; 23(4): 584–588. doi: 10.1080/10803548.2016.1199501.
8.
D’Amato M, Molino A, Calabrese G, et al. The impact of cold on the respiratory tract and its consequences to respiratory health. Clin Transl Allergy. 2018; 8: 20. doi: 10.1186/s13601-018-0208-9.
9.
Fargnoli M, Lombardi M, Haber N, et al. Hazard function deployment: a QFD-based tool for the assessment of working tasks – a practical study in the construction industry. Int J Occup Saf Ergon. 2020; 26(2): 348–369. doi: 10.1080/10803548.2018.
10.
Dasaraju PV, Liu C. Infections of the Respiratory System. In: Baron S, editor. Medical Microbiology. 4th ed. Galveston (TX): University of Texas Medical Branch at Galveston. 1996. Chapter 93. Available from: https://www.ncbi.nlm.nih.gov/b....
11.
Eccles R, Wilkinson JE. Exposure to cold and acute upper respiratory tract infection. Rhinology. 2015; 53(2): 99–106. doi: 10.4193/Rhin14.239.
12.
Kuchar E, Miśkiewicz K, Szenborn L, et al. Respiratory tract infections in children in primary healthcare in Poland. Adv Exp Med Biol. 2015; 835: 53–9. doi: 10.1007/5584_2014_34.
13.
Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician. 2018; 64(11): 832–840.
14.
Gombart AF, Pierre A, Maggini S. A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients. 2020; 12(1): pii: E236. doi: 10.3390/nu12010236.
15.
Smiley D. Seasonal factors in the incidence of the acute respiratory infections. Am J Hygiene. 1926; 6: 621–626.
16.
Berry DJ, Hesketh K, Power C, et al. Vitamin D status has a linear association with seasonal infections and lung function in British adults. Br J Nutr. 2011; 106: 1433–1440. doi: 10.1017/S0007114511001991.
17.
Pham H, Rahman A, Majidi A, et al. Acute Respiratory Tract Infection and 25-Hydroxyvitamin D Concentration: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2019; 16(17): pii: E3020. doi: 10.3390/ijerph16173020.
18.
Greiller CL, Martineau AR. Modulation of the immune response to respiratory viruses by vitamin D. Nutrients. 2015; 7: 4240–4270. doi: 10.3390/nu7064240.
19.
Farrokhyar F, Tabasinejad R, Dao D, et al. Prevalence of vitamin D inadequacy in athletes: a systematic-review and meta-analysis. Sports Med. 2015; 45: 365–378. doi: 10.1007/s40279-014-0267-6.
20.
Płudowski P, Ducki C, Konstantynowicz J, et al. Vitamin D status in Poland. Pol Arch Med Wewn. 2016; 126(7–8): 530–539. doi: 10.20452/pamw.3479.
21.
Walsh NP. Recommendations to maintain immune health in athletes. Eur J Sport Sci. 2018; 18(6): 820–831. doi: 10.1080/17461391.2018.1449895.
22.
Bauer P, Kraushaar L, Hölscher S, et al. Elite athletes as research model: vitamin D insufficiency associates with elevated central blood pressure in professional handball athletes. Eur J Appl Physiol. 2019; 119(10): 2265–2274. doi: 10.1007/s00421-019-04210-w.
23.
Orysiak J, Witek K, Zembron-Lacny A, et al. Mucosal immunity and upper respiratory tract infections during a 24-week competitive season in young ice hockey players. J Sports Sci. 2017; 35: 1255–1263. doi: 10.1080/02640414.2016.1218039.
24.
Jones KS, Redmond J, Fulford AJ, et al. Diurnal rhythms of vitamin D binding protein and total and free vitamin D metabolites. J Steroid Biochem Mol Biol. 2017; 172: 130–135. doi: 10.1016/j.jsbmb.2017.07.015.
25.
Barrett B, Brown RL, Mundt MP, et al. Validation of a short form Wisconsin Upper Respiratory Symptom Survey (WURSS-21). Health Qual Life Outcomes. 2009; 7: 76. doi: 10.1186/1477-7525-7-76.
26.
Hollis BW. Assessment and interpretation of circulating 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D in the clinical environment. Endocrinol Metab Clin North Am. 2010; 39: 271–286. doi: 10.1016/j.ecl.2010.02.012.
27.
IOM. Institute of Medicine. Dietary Reference Intakes for calcium and Vitamin D. Washington, DC: The National Academy Press. 2011.
28.
He CS, Handzlik M, Fraser WD, et al. Influence of vitamin D status on respiratory infection incidence and immune function during 4 months of winter training in endurance sport athletes. Exerc Immunol Rev. 2013; 19: 86–101.
29.
Grzenia A, Kazanowska D, Kazimierowska-Wasiołek M, et al. Working conditions in 2018. Statistics Poland. Statistical Office in Gdańsk, Centre for Working Conditions Statistics, Pomeranian Centre for Regional Surveys. 2019.https://stat.gov.pl/files/gfx/... aktualnosci/5476/1/13/1/warunki_pracy_w_2018.pdf (access: 2020.06.22).
30.
Dicpinigaitis PV, Eccles R, Blaiss MS, et al. Impact of cough and common cold on productivity, absenteeism, and daily life in the United States: ACHOO Survey. Curr Med Res Opin. 2015; 31(8): 1519–1525. doi: 10.1185/03007995.2015.1062355.
31.
Karczewicz E, Sikora A. 2019. Absencja chorobowa w 2018 roku. https://www.zus.pl/documents/1... (access: 2020.06.22).
32.
Hansen S, Zimmerman P, van de, Mortel T. Assessing workplace infectious illness management in Australian workplaces. Infect Dis Health. 2017; 22(1): 12–20.
33.
Gleeson M, Bishop N, Oliveira M, et al. Respiratory infection risk in athletes: association with antigen-stimulated IL-10 production and salivary IgA secretion. Scand J Med Sci Sports. 2012; 22: 410–417. doi: 10.1111/j.1600-0838.2010.01272.x.
34.
He CS, Fraser WD, Gleeson M. Influence of vitamin D metabolites on plasma cytokine concentrations in endurance sport athletes and on multiantigen stimulated cytokine production by whole blood and peripheral blood mononuclear cell cultures. ISRN Nutr. 2014; 2014: 820524. doi: 10.1155/2014/820524.
35.
Ginde AA, Mansbach JM, Camargo CAJr. Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2009; 169: 384–390. doi: 10.1001/archinternmed.2008.560.
36.
Halliday TM, Peterson NJ, Thomas JJ, et al. Vitamin D status relative to diet, lifestyle, injury, and illness in college athletes. Med Sci Sports Exerc. 2011; 43: 335–343. doi: 10.1249/MSS.0b013e3181eb9d4d.
37.
Laaksi I, Ruohola JP, Tuohimaa P, et al. An association of serum vitamin D concentrations < 40 nmol/L with acute respiratory tract infection in young Finnish men. Am J Clin Nutr. 2007; 86: 714–717.
38.
Sabetta JR, DePetrillo P, Cipriani RJ, et al. Serum 25-hydroxyvitamin D and the incidence of acute viral respiratory tract infections in healthy adults. PLoS One. 2010; 5: e11088. doi: 10.1371/journal.pone.0011088.
39.
Scullion L, Baker D, Healey P, et al. No Association between Vitamin D and Acute Respiratory Tract Infections Amongst Elite New Zealand Rugby Players and Rowers. Int J Vitam Nutr Res. 2018; 88(1–2): 8–15. doi: 10.1024/0300-9831/a000285.
40.
Jung HC, Seo MW, Lee S, et al. Vitamin D₃ Supplementation Reduces the Symptoms of Upper Respiratory Tract Infection during Winter Training in Vitamin D-Insufficient Taekwondo Athletes: A Randomized Controlled Trial. Int J Environ Res Public Health. 2018; 15(9): pii: E2003. doi: 10.3390/ijerph15092003.
41.
Martineau AR, Jolliffe DA, Greenberg L, et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health Technol Assess. 2019; 23(2): 1–44. doi: 10.3310/hta23020.
42.
Krzywanski J, Mikulski T, Krysztofiak H, et al. Seasonal Vitamin D Status in Polish Elite Athletes in Relation to Sun Exposure and Oral Supplementation. PLoS One. 2016; 11: e0164395. doi: 10.1371/journal.pone.0164395.
43.
Kmieć P, Sworczak K. Vitamin D deficiency in early autumn among predominantly non-elderly, urban adults in Northern Poland (54°N). Postepy Hig Med Dosw (Online). 2015; 69: 918–924. doi: 10.5604/17322693.1165194.
44.
Backx E, van der Avoort C, Tieland M, et al. Seasonal Variation in Vitamin D Status in Elite Athletes: A Longitudinal Study. Int J Sport Nutr Exerc Metab. 2017; 27: 6–10. doi: 10.1123/ijsnem.2016-0177.
45.
Hellard P, Avalos M, Guimaraes F, et al. Training-related risk of common illnesses in elite swimmers over a 4-yr period. Med Sci Sports Exerc. 2015; 47: 698–707.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.