Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Multifactorial influence of type 2 diabetes on cardiovascular risk assessed by PolSCORE, SCORE2 in the age group 40–69 years
1
Department of Physiotherapy, Medical College, University of Information Technology and Management, Rzeszów, Poland
2
Department of Nursing, Medical College, University of Information Technology and Management, Rzeszów, Poland
3
Institute of Humanities and Medicine, Academy of Zamość, Poland
4
Faculty of Health Sciences, Vincent Pol University, Lublin, Poland
Corresponding author
Marlena Krawczyk-Suszek
Department of Physiotherapy, Medical College, University of Information Technology and Management in Rzeszow, 2 Sucharskiego Str., 35 - 225, Rzeszow, Poland
Department of Physiotherapy, Medical College, University of Information Technology and Management in Rzeszow, 2 Sucharskiego Str., 35 - 225, Rzeszow, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Cardiovascular risk (CV risk) is the probability of developing cardiovascular disease or dying from it within a specified period of time. One of the main factors increasing this risk is diabetes (DM). The aim of the study was to assess the effect of type 2 diabetes (T2DM) on CV risk based on the SCORE and SCORE2 scales, taking other factors into account.
Material and methods:
The study was conducted in a group of 1,540 people aged 40–89 years (226 people with diabetes –T2DM(+)). The following scales were used to assess CV risk: Pol-SCORE and SCORE2. Inclusion criterion was the absence of cardiovascular complications such as: myocardial infarction, overt coronary artery disease, previous stroke, renal failure or complications of T2DM.
Results:
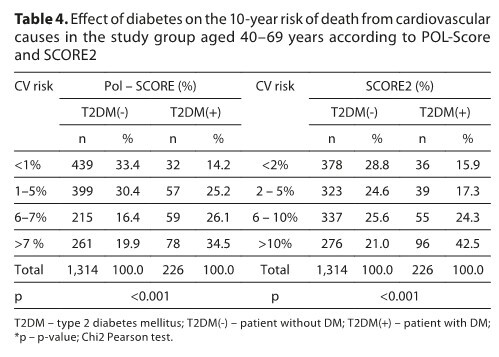
In the T2DM(+) group, high and very high CV risk was more frequently noted (Pol-SCORE: 26.1% and 34.5%; SCORE2: 24.3% and 42.5%) compared to T2DM(-). The regression model included an analysis of 10 factors determining CV risk. In estimating CV risk using the Pol-SCORE scale, 8 factors were most important (P=0.86), in the SCORE2 scale a total of 3 factors (TC – total cholesterol; LDL; TGs – triglyceride). In the T2DM(+) group, age(r=0.53) and TC(r=0.43) showed the strongest positive correlation with SCORE2, while for Pol-SCORE – age(r=0.05).
Conclusions:
In the CV risk assessment using the Pol-SCORE scale, the following were of significant importance: TC, HDL, LDL, TGs, non-HDL, systolic pressure, diastolic pressure, heart rate. In the risk assessment using the SCORE2 scale, the following were significant: total cholesterol and triglyceride. Diagnosed T2DM significantly increases CV risk.
Cardiovascular risk (CV risk) is the probability of developing cardiovascular disease or dying from it within a specified period of time. One of the main factors increasing this risk is diabetes (DM). The aim of the study was to assess the effect of type 2 diabetes (T2DM) on CV risk based on the SCORE and SCORE2 scales, taking other factors into account.
Material and methods:
The study was conducted in a group of 1,540 people aged 40–89 years (226 people with diabetes –T2DM(+)). The following scales were used to assess CV risk: Pol-SCORE and SCORE2. Inclusion criterion was the absence of cardiovascular complications such as: myocardial infarction, overt coronary artery disease, previous stroke, renal failure or complications of T2DM.
Results:
In the T2DM(+) group, high and very high CV risk was more frequently noted (Pol-SCORE: 26.1% and 34.5%; SCORE2: 24.3% and 42.5%) compared to T2DM(-). The regression model included an analysis of 10 factors determining CV risk. In estimating CV risk using the Pol-SCORE scale, 8 factors were most important (P=0.86), in the SCORE2 scale a total of 3 factors (TC – total cholesterol; LDL; TGs – triglyceride). In the T2DM(+) group, age(r=0.53) and TC(r=0.43) showed the strongest positive correlation with SCORE2, while for Pol-SCORE – age(r=0.05).
Conclusions:
In the CV risk assessment using the Pol-SCORE scale, the following were of significant importance: TC, HDL, LDL, TGs, non-HDL, systolic pressure, diastolic pressure, heart rate. In the risk assessment using the SCORE2 scale, the following were significant: total cholesterol and triglyceride. Diagnosed T2DM significantly increases CV risk.
REFERENCES (33)
1.
Araszkiewicz A, Bandurska-Stankiewicz E, Borys S, et al. 2023 Guidelines on the management of patients with diabetes – a position of Diabetes Poland. Curr Top Diabetes. 2023;3(1):1–133.
2.
Singh VP, Bali A, Singh N, Jaggi AS. Advanced Glycation End Products and Diabetic Complications. Korean J Physiol Pharmacol. 2014;18(1):1.
3.
Sigala EG, Panagiotakos DB. Assessment of Lifetime Risk for Cardiovascular Disease: Time to Move Forward. Curr Cardiol Rev. 2024;20(6):e030724231561.
4.
Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019. J Am Coll Cardiol. 2020;76(25):2982–3021.
5.
Sun J, Qiao Y, Zhao M, et al. Global, regional, and national burden of cardiovascular diseases in youths and young adults aged 15–39 years in 204 countries/territories, 1990–2019: a systematic analysis of Global Burden of Disease Study 2019. BMC Med. 2023;21(1):222.
6.
Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–337.
7.
Xu G, Xu Y, Zheng T, Liu T. Type 2 diabetes and inflammatory bowel disease: a bidirectional two-sample Mendelian randomization study. Sci Rep. 2024;14(1):5149.
8.
Zdrojewski T, Jankowski P, Bandosz P, et al. A new version of cardiovascular risk assessment system and risk charts calibrated for Polish population. Kardiol Pol. 2015;73(10):958–61.
9.
Hageman S, Pennells L, Ojeda F, et al. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021;42(25):2439–54.
10.
Stępień-Wałek A, Gorczyca-Michta I, Tomasik E, et al. Concomitant diseases and selected cardiovascular complications in hospitalised patients with hypertensiion and diabetes. Folia Cardiologica. 2014;9(1):10–16.
11.
WMA Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (access: 2025.03.28).
12.
Broncel M. The new ESC guidelines for the prevention of cardiovascular diseases – what changes do they bring to medical practice? Med Faktów. 2022;15(1):8–17.
13.
Postuła M, Jarosz-Popek J. Skala SCORE2 – nowe narzędzie w kardiologii prewencyjnej. Med Dypl. 2022;32(3):2–7.
14.
WHO. The top 10 causes of death. www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (access:2025.03.28).
15.
GUS. Zachorowalność i umieralność na choroby układu krążenia a sytuacja demograficzna Polski. https://bip.stat.gov.pl/organi... (access: 2025.03.29).
16.
Galiuto L, Locorotondo G. Cardiovascular Aging. In: Fioranelli M, editor. Integrative Cardiology. Springer International Publishing, Cham; 2017. p. 109–20.
17.
Krawczyk-Suszek M, Gaweł A, Kleinrok A. Correlation of ageing with Health related-quality of life of patients in 13 groups of disease in Poland. Sci Rep. 2024;14(1):26404.
18.
Krawczyk-Suszek M, Gaweł A, Kleinrok A. Ranking of diseases affecting the health-related quality of life of patients in Poland – a cross-sectional study. Archives of Medical Science. 2024;20(5):1567–1578.
19.
Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation. 2019;139(10):e56-e528.
20.
Keto J, Ventola H, Jokelainen J, et al. Cardiovascular disease risk factors in relation to smoking behaviour and history: a population-based cohort study. Open Heart. 2016;3(2):e000358.
21.
Glovaci D, Fan W, Wong ND. Epidemiology of Diabetes Mellitus and Cardiovascular Disease. Curr Cardiol Rep. 2019;21(4):21.
22.
Cebrián-Cuenca AM, Mata-Cases M, Franch-Nadal J, et al. Half of patients with type 2 diabetes mellitus are at very high cardiovascular risk according to the ESC/EASD: data from a large Mediterranean population. Eur J Prev Cardiol. 2022;28(18):e32–4.
23.
Pintaudi B, Scatena A, Piscitelli G, et al. Clinical profiles and quality of care of subjects with type 2 diabetes according to their cardiovascular risk: an observational, retrospective study. Cardiovasc Diabetol. 2021;20(1):59.
24.
Rydén L, Ferrannini G, Standl E. Risk prediction in patients with diabetes: is SCORE 2D the perfect solution? Eur Heart J. 2023;44(28):2557–9.
25.
Pennells L, Kaptoge S, Østergaard HB, et al. SCORE2-Diabetes: 10-year cardiovascular risk estimation in type 2 diabetes in Europe. Eur Heart J. 2023;44(28):2544–56.
26.
Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41(2):255–323.
27.
Wahid A, Manek N, Nichols M, et al. Quantifying the Association Between Physical Activity and Cardiovascular Disease and Diabetes: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2016;5(9): e002495.
28.
Cleven L, Krell-Roesch J, Nigg CR, Woll A. The association between physical activity with incident obesity, coronary heart disease, diabetes and hypertension in adults: a systematic review of longitudinal studies published after 2012. BMC Public Health. 2020;20(1):726.
29.
Choi JW, Han E, Kim TH. Association of smoking cessation after new-onset type 2 diabetes with overall and cause-specific mortality among Korean men: a nationwide population-based cohort study. BMJ Open Diabetes Res Care. 2020;8(1):e001249.
30.
Critchley JA, Capewell S. Mortality Risk Reduction Associated With Smoking Cessation in Patients With Coronary Heart Disease. JAMA. 2003;290(1):86.
31.
Global Effect of Modifiable Risk Factors on Cardiovascular Disease and Mortality. New England J Med. 2023;389(14):1273–85.
32.
Luca SA, Bungau RM, Lazar S, et al. To What Extent Does Cardiovascular Risk Classification of Patients with Type 2 Diabetes Differ between European Guidelines from 2023, 2021, and 2019? A Cross-Sectional Study. Medicina (B Aires). 2024;60(2):334.
33.
Liu R, Li L, Shao C, et al. The Impact of Diabetes on Vascular Disease: Progress from the Perspective of Epidemics and Treatments. J Diabetes Res. 2022;2022:1–17.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.