Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Malnutrition as the cause of growth retardation among children in developed countries
1
Department of Paediatric Diabetes, Auxology and Obesity, Poznan University of Medical Sciences, Poznań, Poland
Corresponding author
Joanna Budzulak
Department of Pediatric Diabetes, Auxology and Obesity, Poznan University of Medical Sciences, Szpitalna 27/33, 60-572, Poznań, Poland
Department of Pediatric Diabetes, Auxology and Obesity, Poznan University of Medical Sciences, Szpitalna 27/33, 60-572, Poznań, Poland
Ann Agric Environ Med. 2022;29(3):336-341
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
According to the World Health Organization (WHO), malnutrition is a term that covers three broad groups of conditions: undernutrition, micronutrient-related malnutrition, and overweight with obesity, and diet-related non-communicable diseases. Undernutrition is the leading cause of growth failure worldwide, mainly in third-world countries where stunting is a significant public health problem arising from food poverty. In developed countries, malnutrition resulting in growth failure might often be misdiagnosed in paediatric practice. The aim of this study was to review the current state of knowledge regarding nutritional causes of growth retardation among children in developed countries.
Materials and method.:
The review was based on data obtained from articles published in the PubMed database (https://pubmed.ncbi.nlm.nih.gov/) between 2004–2021. The expert reports of the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF), were also included.
Brief description of the state of knowledge:
Nutritional growth retardation (NGR) is challenging to diagnose, as it may result from mild food restrictions without apparent abnormalities in biochemical parameters of nutritional status. Reduced insulin-like growth factor type 1 (IGF-1) may suggest NGR, but it also occurs in endocrine disorders such as growth hormone deficiency.
Conclusion:
NGR is a phenomenon that can occur in underweight children and those with normal or excessive body weight. As no effective diagnostic biochemical test is available, it seems that paediatric patients with growth failure should undergo dietary analysis preceding further advanced endocrine and biochemical diagnostic procedures.
According to the World Health Organization (WHO), malnutrition is a term that covers three broad groups of conditions: undernutrition, micronutrient-related malnutrition, and overweight with obesity, and diet-related non-communicable diseases. Undernutrition is the leading cause of growth failure worldwide, mainly in third-world countries where stunting is a significant public health problem arising from food poverty. In developed countries, malnutrition resulting in growth failure might often be misdiagnosed in paediatric practice. The aim of this study was to review the current state of knowledge regarding nutritional causes of growth retardation among children in developed countries.
Materials and method.:
The review was based on data obtained from articles published in the PubMed database (https://pubmed.ncbi.nlm.nih.gov/) between 2004–2021. The expert reports of the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF), were also included.
Brief description of the state of knowledge:
Nutritional growth retardation (NGR) is challenging to diagnose, as it may result from mild food restrictions without apparent abnormalities in biochemical parameters of nutritional status. Reduced insulin-like growth factor type 1 (IGF-1) may suggest NGR, but it also occurs in endocrine disorders such as growth hormone deficiency.
Conclusion:
NGR is a phenomenon that can occur in underweight children and those with normal or excessive body weight. As no effective diagnostic biochemical test is available, it seems that paediatric patients with growth failure should undergo dietary analysis preceding further advanced endocrine and biochemical diagnostic procedures.
REFERENCES (46)
1.
World Health Organization (WHO). Malnutrition. https://www.who.int/news-room/... (access: 2022.02.22).
2.
Abera L, Dejene T, Laelago T. Prevalence of malnutrition and associated factors in children aged 6–59 months among rural dwellers of damot gale district, south Ethiopia: community based cross sectional study. Int J Equity Health. 2017;16(1):111. https://doi.org/10.1186/s12939....
3.
de Onis M, Branca F. Childhood stunting: a global perspective. Matern Child Nutr. 2016; 12(S1): 12–26. https://doi.org/10.1111/mcn.12....
4.
United Nations Children’s Fund (UNICEF), World Health Organization, International Bank for Reconstruction and Development/The World Bank. Levels and trends in child malnutrition: Key Findings of the 2020 Edition of the Joint Child Malnutrition Estimates. Geneva: World Health Organization; 2020. https://www.unicef.org/reports... (access: 2022.02.22).
5.
Farhadi S, Ovchinnikov RS. The relationship between nutrition and infectious diseases: A review. Biomed Biotechnol Res J. 2018; 2(3): 168–172. https://doi.org/10.4103/bbrj.b....
6.
Prendergast AJ, Humphrey JH. The stunting syndrome in developing countries. Paediatr Int Child Health. 2014; 34(4): 250–265. https://doi.org/10.1179/204690....
7.
De Lucia Rolfe E, de França GVA, Vianna CA, et al. Associations of stunting in early childhood with cardiometabolic risk factors in adulthood. PLoS One. 2018; 13(4): e0192196. https://doi.org/10.1371/journa....
8.
Homan GJ. Failure to Thrive: A Practical Guide. Am Fam Physician. 2016; 94(4): 295–299.
9.
Hawkes CP, Grimberg A. Insulin-Like Growth Factor-1 is a Marker for the Nutritional State. Pediatr Endocrinol Rev. 2015; 13(2): 499–511.
10.
Gat-Yablonski G, Phillip M. Nutritionally-induced catch-up growth. Nutrients. 2015; 7(1): 517–551. https://doi.org/10.3390/nu7010....
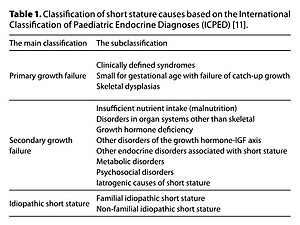
11.
International Classification of Pediatric Endocrine Diagnoses (ICPED), 2015, ICPED code 1. http://www.icped.org (access: 2022.02.22).
12.
Zadik Z, Sinai T, Zung A, et al. Effect of nutrition on growth in short stature before and during growth-hormone therapy. Pediatrics. 2005; 116(1): 68–72. https://doi.org/10.1542/peds.2....
13.
Fazeli PK, Klibanski A. Determinants of GH resistance in malnutrition. J Endocrinol. 2014; 220(3): R57-R65. https://doi.org/10.1530/JOE-13....
14.
Lezo A, Baldini L, Asteggiano M. Failure to Thrive in the Outpatient Clinic: A New Insight. Nutrients. 2020; 12(8): 2202. https://doi.org/10.3390/nu1208....
15.
Thomas JJ, Lawson EA, Micali N, et al. Avoidant/Restrictive Food Intake Disorder: a Three-Dimensional Model of Neurobiology with Implications for Etiology and Treatment. Curr Psychiatry Rep. 2017; 19(8): 54. https://doi.org/10.1007/s11920....
16.
Robbins KA, Wood RA, Keet CA. Persistent cow’s milk allergy is associated with decreased childhood growth: A longitudinal study. J Allergy Clin Immunol. 2020; 145(2): 713–716.e4. https://doi.org/10.1016/j.jaci....
17.
Morency ME, Birken CS, Lebovic G, et al. Association between noncow milk beverage consumption and childhood height. Am J Clin Nutr. 2017; 106(2): 597–602. https://doi.org/10.3945/ajcn.1....
18.
Dittfeld A, Gwizdek K, Parol D, et al. Dieta bezglutenowa – charakterystyka grup docelowych. Postep Hig Med Dosw. 2018; 72: 227–239.
19.
Soliman A, De Sanctis V, Elalaily R. Nutrition and pubertal development. Indian J Endocrinol Metab. 2014; 18(Suppl 1): S39–S47. http://www.doi.org/10.4103/223....
20.
Lifshitz F. Nutrition and growth. J Clin Res Pediatr Endocrinol. 2009; 1(4): 157–163. https://doi.org/10.4274/jcrpe.....
21.
Kim YJ. Nutritional concerns in pediatric inflammatory bowel disease. Korean J Pediatr. 2016; 59(6): 247–251. https://doi:10.3345/kjp.2016.5....
22.
Iorember FM. Malnutrition in Chronic Kidney Disease. Front Pediatr. 2018; 6: 161. https://doi:10.3389/fped.2018.....
23.
Semba RD, Shardell M, Sakr Ashour FA, et al. Child Stunting is Associated with Low Circulating Essential Amino Acids. EBioMedicine. 2016; 6: 246–252. https://doi.org/10.1016/j.ebio....
24.
van Vught AJ, Dagnelie PC, Arts IC, et al. Dietary arginine and linear growth: the Copenhagen School Child Intervention Study. Br J Nutr. 2013; 109(6): 1031–1039. https://doi.org/10.1017/S00071....
25.
Hamner HC, Perrine CG, Scanlon KS. Usual Intake of Key Minerals among Children in the Second Year of Life, NHANES 2003–2012. Nutrients. 2016; 8(8): 468. https://doi.org/10.3390/nu8080....
26.
Robbins KA, Wood RA, Keet CA. Milk allergy is associated with decreased growth in US children. J Allergy Clin Immunol. 2014; 134(6): 1466–1468.e6. https://doi.org/10.1016/j.jaci....
27.
Esposito S, Leonardi A, Lanciotti L, et al. Vitamin D and growth hormone in children: a review of the current scientific knowledge. J Transl Med. 2019; 17(1): 87. https://doi.org/10.1186/s12967....
28.
Cole CR, Lifshitz F. Zinc nutrition and growth retardation. Pediatr Endocrinol Rev. 2008; 5(4): 889–896.
29.
Mennella JA, Bobowski NK. The sweetness and bitterness of childhood: Insights from basic research on taste preferences. Physiol Behav. 2015; 152(Pt B): 502–507. https://doi.org/10.1016/j.phys....
30.
Mennella JA, Bobowski NK, Reed DR. The development of sweet taste: From biology to hedonics. Rev Endocr Metab Disord. 2016; 17(2): 171–178. https://doi.org/10.1007/s11154....
31.
Bennett LJ, Totosy de Zepetnek JO, Brett NR, et al. Effect of Commercially Available Sugar-Sweetened Beverages on Subjective Appetite and Short-Term Food Intake in Girls. Nutrients. 2018; 10(4): 394. https://doi.org/10.3390/nu1004....
32.
Bowman SA, Clemens JC, Friday JE, et.al. Added Sugars in American Children’s Diet: What We Eat in America, NHANES 2015–2016. Food Surveys Research Group. Dietary Data Brief No. 26. December 2019. http://www.doi.org/10.13140/RG....
33.
Khan TA, Sievenpiper JL. Controversies about sugars: results from systematic reviews and meta-analyses on obesity, cardiometabolic disease and diabetes. Eur J Nutr. 2016; 55(Suppl 2): 25–43. https://doi.org/10.1007/s00394....
34.
van de Gaar VM, van Grieken A, Jansen W, et al. BMC Public Health. Children’s sugar-sweetened beverages consumption: associations with family and home-related factors, differences within ethnic groups explored. BMC Public Health. 2017; 17(1): 195. https://doi.org/10.1186/s12889....
35.
Marcovecchio ML, Chiarelli F. Obesity and growth during childhood and puberty. World Rev Nutr Diet. 2013; 106: 135–141. https://doi.org/10.1159/000342....
36.
Ballerini MG, Ropelato MG, Domené HM, et al. Differential impact of simple childhood obesity on the components of the growth hormone-insulin-like growth factor (IGF)-IGF binding proteins axis. J Pediatr Endocrinol Metab. 2004; 17(5): 749–755. https://doi.org/10.1515/jpem.2....
37.
Chung S. Growth and Puberty in Obese Children and Implications of Body Composition. J Obes Metab Syndr. 2017; 26(4): 243–250. https://doi.org/10.7570/jomes.....
38.
Pinhas-Hamiel O, Benary D, Mazor-Aronovich K, et al. Advanced bone age and hyperinsulinemia in overweight and obese children. Endocr Pract. 2014; 20(1): 62–67. https://doi.org/10.4158/EP1319....
39.
Beghini M, Brandt S, Körber I, et al. Serum IGF1 and linear growth in children with congenital leptin deficiency before and after leptin substitution. Int J Obes (Lond). 2021; 45(7): 1448–1456. https://doi.org/10.1038/s41366....
40.
World Health Organization (WHO). The double burden of malnutrition. Policy brief. Geneva: World Health Organization; 2017. https://www.who.int/publicatio... (access:2022.02.22).
41.
Keino S, Plasqui G, Ettyang G, et al. Determinants of stunting and overweight among young children and adolescents in sub-Saharan Africa. Food Nutr Bull. 2014; 35(2): 167–178. https://doi.org/10.1177%2F1564....
42.
Kroker-Lobos MF, Pedroza-Tobías A, Pedraza LS, et al. The double burden of undernutrition and excess body weight in Mexico. Am J Clin Nutr. 2014; 100(6): 1652S–1658S. https://doi.org/10.3945/ajcn.1....
43.
Singh Malik V, Dayal D, Khaiwal R, et al. Low serum copper and zinc concentrations in North Indian children with overweight and obesity. Pediatric Endocrinology Diabetes and Metabolism. 2020; 26(2): 79–83. https://doi.org/10.5114/pedm.2....
44.
Smyczyńska J, Hilczer M, Lewinski A, et al. Effectiveness, economical and safety aspects of growth hormone (GH) therapy in growth promoting doses in patients with isolated GH deficiency after the attainment of near-final height. Is there a need to modify the criteria of therapy withdrawal? Pediatric Endocrinology Diabetes and Metabolism. 2021; 27(4): 258–265. https://doi:10.5114/pedm.2021.....
45.
Lohiya N, Krishna Prasad H, Narayanasamy K, et al. Factors influencing growth in children with growth hormone deficiency – a case-control study. Pediatric Endocrinology Diabetes and Metabolism. 2021; 27(1): 19–25. https://doi:10.5114/pedm.2020.....
46.
SEZER OB, BULUŞ D. Short stature, insufficient annual height growth and back bone age: Nutritional growth retardation or growth hormone deficiency? Journal Of Contemporary Medicine 2016; 6(4): 277–282. https://doi.org/10.16899/ctd.3....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.