Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Influence of socio-demographic characteristics on the evaluation of effectiveness of medical
simulation
1
Department of Nursing and Public Health, Institute of Health Sciences, College of Medical Sciences, Rzeszów University, Poland
2
Department of Epidemiology, Institute of Rural Health, Lublin, Poland
3
Department of Medical Informatics and Statistics with E-learning Laboratory, Medical University, Lublin, Poland
4
Monoprofile Medical Simulation Centre, Academy of Economics and Education, Lublin, Poland
5
Department of Medical Anthropology, Institute of Rural Health, Lublin, Poland
6
Institute of Rural Health, Lublin, Poland
Corresponding author
Paulina Kaczor-Szkodny
Department of Epidemiology and Biostatistics, Institute of Rural Health, ul. Jaczewskiego 2, 20-090, Lublin, Poland
Department of Epidemiology and Biostatistics, Institute of Rural Health, ul. Jaczewskiego 2, 20-090, Lublin, Poland
Ann Agric Environ Med. 2025;32(3):377-382
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Learning effectiveness is a key element in the educational process that determines how effectively students can assimilate, store, and apply the knowledge acquired. There are many approaches and theories in the research literature exploring the different aspects of this process. Factors influencing learning effectiveness include learning style, motivation, learning techniques, and learning environment. Learning effectiveness also depends on individual student characteristics, including socio-demographic characteristics. The aim of the study is to verify the influence of socio-demographic characteristics on the assessment of the effectiveness of medical simulation as a learning method, using the standardised EPQ tool.
Material and methods:
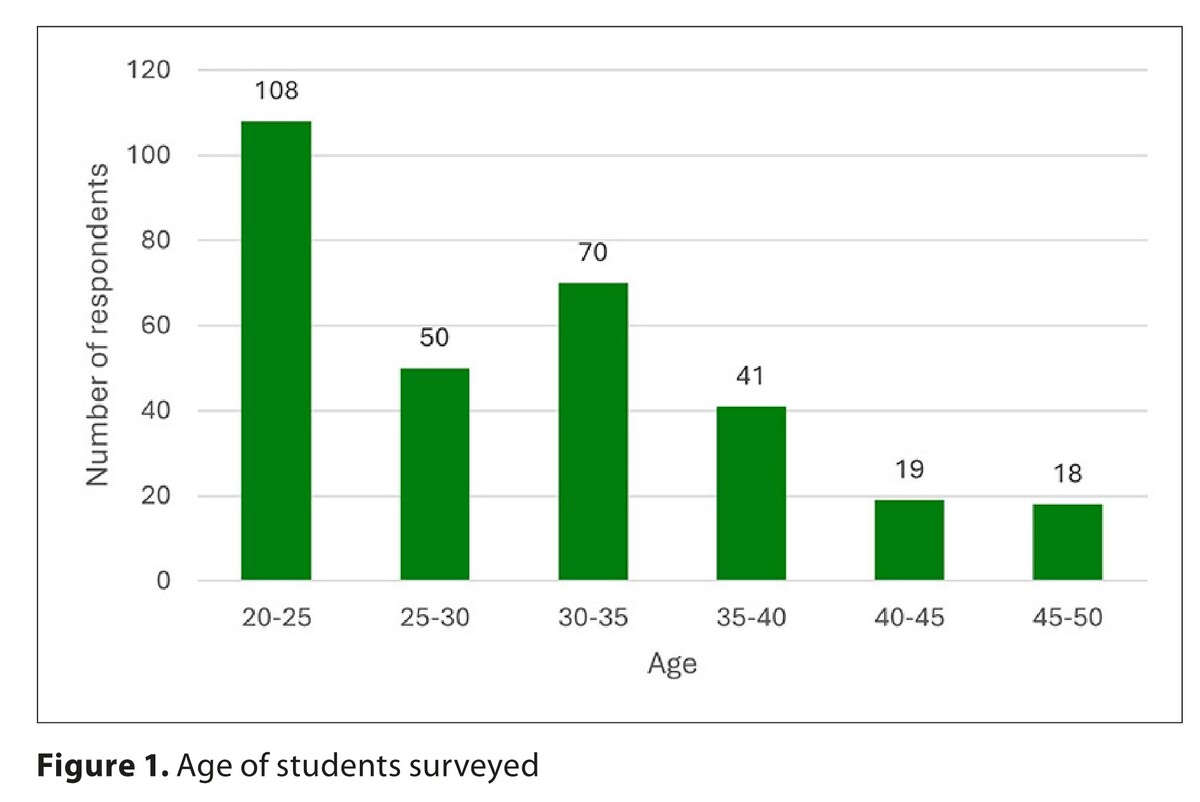
The study was conducted between 2023–2024 among 306 nursing students by means of a diagnostic survey, using the survey instrument EPQ.
Results:
The surveyed students rated the educational techniques best in terms of collaboration. Statistical analysis showed a weak negative correlation between age and the evaluation of active learning, expectations, and the overall evaluation of educational techniques. Statistically significant results were obtained in the correlation of place of residence with the evaluation of educational practices.
Conclusions:
The study showed a general relationship of the influence of selected socio-demographic characteristics on the evaluation of educational practices in medical simulation. Despite the occurrence of a relationship, the age of the subjects did not determine the outcome of the simulation effectiveness evaluation. There is a lack of detailed research in the available literature on the influence of socio-demographic variables on the evaluation of medical simulation educational practices, which allowed the identification of a research gap (white gap).
Learning effectiveness is a key element in the educational process that determines how effectively students can assimilate, store, and apply the knowledge acquired. There are many approaches and theories in the research literature exploring the different aspects of this process. Factors influencing learning effectiveness include learning style, motivation, learning techniques, and learning environment. Learning effectiveness also depends on individual student characteristics, including socio-demographic characteristics. The aim of the study is to verify the influence of socio-demographic characteristics on the assessment of the effectiveness of medical simulation as a learning method, using the standardised EPQ tool.
Material and methods:
The study was conducted between 2023–2024 among 306 nursing students by means of a diagnostic survey, using the survey instrument EPQ.
Results:
The surveyed students rated the educational techniques best in terms of collaboration. Statistical analysis showed a weak negative correlation between age and the evaluation of active learning, expectations, and the overall evaluation of educational techniques. Statistically significant results were obtained in the correlation of place of residence with the evaluation of educational practices.
Conclusions:
The study showed a general relationship of the influence of selected socio-demographic characteristics on the evaluation of educational practices in medical simulation. Despite the occurrence of a relationship, the age of the subjects did not determine the outcome of the simulation effectiveness evaluation. There is a lack of detailed research in the available literature on the influence of socio-demographic variables on the evaluation of medical simulation educational practices, which allowed the identification of a research gap (white gap).
REFERENCES (20)
1.
Wroniszewski Ł, Wacowska-Szewczyk M, Bartczak M, et al. Symulacja medyczna jako forma nauczania inwazyjnych procedur medycznych ratujących życie. In: Timler D, Bartczak M, editor. Medycyna ratunkowa i edukacja z wykorzystaniem symulacji. Część II: edukacja z wykorzystaniem symulacji. Wydawnictwo Uniwersytetu Medycznego w Łodzi; 2021:15(2).
2.
Rubio-López A, García-Carmona R, Zarandieta-Román L, et al. Analysis of stress responses in medical students during simulated pericardiocentesis training using virtual reality and 3D-printed mannequin. Sci Rep. 2025;15(1):7645. Published 2025 Mar 4. doi:10.1038/s41598-025-92221-3.
3.
Xu M, Luo Y, Zhang Y, et al. Game-based learning in medical education. Front Public Health. 2023;11:1113682. Published 2023 Mar 3. doi:10.3389/fpubh.2023.1113682.
4.
Sobierańska P, Janusz K, Janczukowicz J. Symulacja medyczna jako narzędzie edukacyjne. In: Timler D, Bartczak M, editor. Medycyna ratunkowa i edukacja z wykorzystaniem symulacji. Część II: edukacja z wykorzystaniem symulacji. Wydawnictwo Uniwersytetu Medycznego w Łodzi; 2021:15(2).
5.
Sezgin MG, Bektas H. Effectiveness of interprofessional simulation-based education programs to improve teamwork and communication for students in the healthcare profession: A systematic review and meta-analysis of randomized controlled trials. Nurse Educ Today. 2023;120:105619. doi:10.1016/j.nedt.2022.105619.
6.
Wawszczak E. Założenia symulacji medycznej w kształceniu zawodowym. In: Wiśniewski A, Chełstowska B, editor. Symulacja medyczna. Informator dla studentów kierunku pielęgniarstwo. Uniwersytet Kardynała Stefana Wyszyńskiego w Warszawie; 2023. ISBN: 9788382814255.
7.
Shuyi AT, Zikki LYT, Mei Qi A, Koh Siew Lin S. Effectiveness of interprofessional education for medical and nursing professionals and students on interprofessional educational outcomes: A systematic review. Nurse Educ Pract. 2024;74:103864. doi:10.1016/j.nepr.2023.103864.
8.
Xavier NA, Brown MR. Interprofessional education in a simulation setting. In: StatPearls [Internet]. StatPearls Publishing; 2023 May 1. PMID: 32491403.
9.
Kowalik J, Pachowicz A, Pachowicz M, Choińska K. Wymiary efektywności edukacyjnej. Humanities and Cultural Studies. 2022;3:91–107. doi:10.55225/hcs.424.
10.
Reierson IÅ, Sandvik L, Solli H, et al. Psychometric testing of the Norwegian version of the Simulation Design Scale, the Educational Practices Questionnaire and the Student Satisfaction and Self-Confidence in Learning Scale in nursing education. Int J Nurs Stud Adv. 2020;2:100012. doi:10.1016/j.ijnsa.2020.100012.
11.
Bokan I, Buljan I, Marušić M, et al. Predictors of academic progression and desire to continue education for undergraduate and graduate nursing students: Cross-sectional study and a nested follow-up study. Nurse Educ Today. 2022;111:105274. doi:10.1016/j.nedt.2022.105274.
12.
Zalewska K, Zarzycka D. Best educational techniques in high-fidelity simulation according to nursing students—adaptation and validation of the Educational Practices Questionnaire (EPQ). Int J Environ Res Public Health. 2022;19(22):14688. doi:10.3390/ijerph192214688.
13.
Farrés-Tarafa M, Roldán-Merino J, Lorenzo-Seva U, et al. Reliability and validity study of the Spanish adaptation of the “Educational Practices Questionnaire” (EPQ). PLoS One. 2020;15(9):e0239014. doi:10.1371/journal.pone.0239014. PMID: 32941464; PMCID: PMC7497994.
14.
Unver V, Basak T, Watts P, et al. The reliability and validity of three questionnaires: The Student Satisfaction and Self-Confidence in Learning Scale, Simulation Design Scale, and Educational Practices Questionnaire. Contemp Nurse. 2017;53(1):60–74. doi:10.1080/10376178.2017.1282319.
15.
Gill BK. Translation and validation of the traditional Chinese NLN educational practices questionnaire, simulation design scale and student satisfaction and self-confidence in learning. J Nurs Educ Pract. 2020;10:47.
16.
Mohamed A, Mohamed L. Perceived nursing students’ satisfaction and self-confidence towards the elements of clinical simulation design and educational practice during the outbreak of COVID-19 pandemic. Tanta Sci Nurs J. 2020;19(2):68–98.
17.
Saad Albagawi B, Grande RAN, Berdida DJE, et al. Correlations and predictors of nursing simulation among Saudi students. Nurs Forum. 2021;56(3):587–595.
18.
Al Ajmi A, Kashoub M, Al-Busaidi IS, et al. Factors influencing choice of residency program among medical intern doctors and medical students: a cross-sectional survey. BMC Med Educ. 2025;25(1):28. Published 2025 Jan 7. doi:10.1186/s12909-024-06576-8.
19.
Asturias N, Andrew S, Boardman G, Kerr D. The influence of socio-demographic factors on stress and coping strategies among undergraduate nursing students. Nurse Educ Today. 2021;99:104780. doi:10.1016/j.nedt.2021.104780.
20.
Wang Y, Ge Y, Chu M, Xu X. Factors influencing nursing undergraduates’ motivation for postgraduate entrance: a qualitative inquiry. BMC Nurs. 2024;23(1):728. Published 2024 Oct 8. doi:10.1186/s12912-024-02373-2.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.