Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Impact of isolation on the biopsychosocial functioning of older people with COVID-19
1
Department of Internal Nursing, Faculty of Health Sciences, Medical University, Wrocław, Poland
2
Institute of Environmental Protection – National Research Institute, Warsaw, Poland
3
Faculty of Pedagogy and Psychology, Jan Kochanowski University, Kielce, Poland
4
Office of the Patient Ombudsman, Poland
5
Collegium Medicum, Jan Kochanowski University, Kielce, Poland
6
Institute of Outcomes Research, Maria Sklodowska-Curie Medical Academy, Poland
7
Institute of Rural Health, Lublin, Poland
Corresponding author
Magdalena Florek-Łuszczki
Instytut Medycyny Wsi w Lublinie, ul. Jaczewskiego 2, 20-090, Lublin, Poland
Instytut Medycyny Wsi w Lublinie, ul. Jaczewskiego 2, 20-090, Lublin, Poland
Ann Agric Environ Med. 2022;29(4):560-567
KEYWORDS
TOPICS
ABSTRACT
Introduction:
COVID-19 is a highly contagious coronavirus disease that has had a significant impact on the functioning of society. On 11 March 2020, due to the rapid spread of the virus, the WHO declared a global pandemic. By the end of 2021, 5 variants of SARS-CoV-2 had been identified since the beginning of the pandemic. The course of the disease varied depending on the age of the patients and the presence of possible comorbidities. Most patients were asymptomatic or sparsely symptomatic of the infection; however, in about 6% of cases, the course of the disease was critical. Typical symptoms of COVID-19 include: fever, muscle pain and headache, lack of smell and taste, cough, dyspnea, diarrhoea and nausea. According to epidemic guidelines, infected patients were subjected to isolation, which harmed their mental state, especially the elderly.
Objective:
The aim of the study was to assess the impact of isolation on the biopsychosocial functioning of elderly patients with COVID-19.
Material and methods:
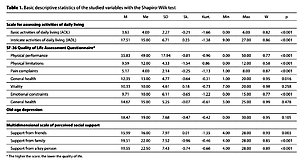
The study was conducted among 360 elderly patients in hospital wards operating as a unit in a hospital complex dedicated to patients infected with the SARS-CoV-2 virus. Data were collected using standardized questionnaires: ADL Scale, IADL, GDS, SF-36 Quality of Life Scale, Multidimensional Scale of Perceived Social Support, and supplementary questions about, among others, the oxygen therapy provided, length of stay in the unit, and the support received from relatives.
Results:
Almost half (48%) of the subjects received oxygen therapy, and 36% had a length of disease of 7–14 days. A correlation was observed between the quality of life and the above-mentioned factors. Correlations of quality of life indicators with the length of illness were moderate (except for the level of pain) and positive, meaning that the longer the patients were ill, the lower their quality of life. Correlations of disease severity were moderate for pain, vitality, and emotional limitations, while vital for physical functioning and limitations and general and mental health. The intensity of oxygen therapy was moderately correlated with physical and emotional limitations and general health and strongly correlated with physical functioning, vitality and mental health. Correlations between functional status and mental status of elderly patients were also studied. Analysis of variance showed that the constructed model was an excellent fit to the data, F = 37.14; p < 0.001, explaining 42% of the variance in the dependent variable (R2= 0.42). As many as 80% of the respondents felt that isolation harmed their well-being. Examining the impact of quality of life on their well-being showed that most of the associations tested were statistically significant, and all were positive. Associations of moderate strength were shown for physical functioning, physical limitations and general health, while strong associations were shown for vitality, emotional limitations and mental health. Pain complaints were associated with changes in well-being at the level of statistical trend (p = 0.055). This means that the lower the patients’ quality of life, especially in terms of vitality and mental health, the more significant the impact of isolation on their well-being. The study also investigated the effect of social support on mental state. The model proved to be an excellent fit to the data, F = 5.91, p = 0.002, and explained 23% of the variance in the dependent variable (Adjusted R² = 0.23). At the same time, support from friends turned out to be the only significant predictor (Beta = 0.53), and this means that the more support the subjects received from them, the lower the level of depression they manifested.
Conclusions:
1) The better the functional state of a senior and the support received from relatives, the lower the severity of depression. 2) The lower the quality of a senior’s life, especially in terms of mental state, the greater the negative impact on his/her well-being in isolation. 3) The low quality of life of a senior increased the likelihood of depression. 4) The quality of life of older Covid-19 patients was higher in those without chronic disease. 5) The quality-of-life level was lower in patients with a more severe course of COVID-19, and longer duration of disease and oxygen therapy.
COVID-19 is a highly contagious coronavirus disease that has had a significant impact on the functioning of society. On 11 March 2020, due to the rapid spread of the virus, the WHO declared a global pandemic. By the end of 2021, 5 variants of SARS-CoV-2 had been identified since the beginning of the pandemic. The course of the disease varied depending on the age of the patients and the presence of possible comorbidities. Most patients were asymptomatic or sparsely symptomatic of the infection; however, in about 6% of cases, the course of the disease was critical. Typical symptoms of COVID-19 include: fever, muscle pain and headache, lack of smell and taste, cough, dyspnea, diarrhoea and nausea. According to epidemic guidelines, infected patients were subjected to isolation, which harmed their mental state, especially the elderly.
Objective:
The aim of the study was to assess the impact of isolation on the biopsychosocial functioning of elderly patients with COVID-19.
Material and methods:
The study was conducted among 360 elderly patients in hospital wards operating as a unit in a hospital complex dedicated to patients infected with the SARS-CoV-2 virus. Data were collected using standardized questionnaires: ADL Scale, IADL, GDS, SF-36 Quality of Life Scale, Multidimensional Scale of Perceived Social Support, and supplementary questions about, among others, the oxygen therapy provided, length of stay in the unit, and the support received from relatives.
Results:
Almost half (48%) of the subjects received oxygen therapy, and 36% had a length of disease of 7–14 days. A correlation was observed between the quality of life and the above-mentioned factors. Correlations of quality of life indicators with the length of illness were moderate (except for the level of pain) and positive, meaning that the longer the patients were ill, the lower their quality of life. Correlations of disease severity were moderate for pain, vitality, and emotional limitations, while vital for physical functioning and limitations and general and mental health. The intensity of oxygen therapy was moderately correlated with physical and emotional limitations and general health and strongly correlated with physical functioning, vitality and mental health. Correlations between functional status and mental status of elderly patients were also studied. Analysis of variance showed that the constructed model was an excellent fit to the data, F = 37.14; p < 0.001, explaining 42% of the variance in the dependent variable (R2= 0.42). As many as 80% of the respondents felt that isolation harmed their well-being. Examining the impact of quality of life on their well-being showed that most of the associations tested were statistically significant, and all were positive. Associations of moderate strength were shown for physical functioning, physical limitations and general health, while strong associations were shown for vitality, emotional limitations and mental health. Pain complaints were associated with changes in well-being at the level of statistical trend (p = 0.055). This means that the lower the patients’ quality of life, especially in terms of vitality and mental health, the more significant the impact of isolation on their well-being. The study also investigated the effect of social support on mental state. The model proved to be an excellent fit to the data, F = 5.91, p = 0.002, and explained 23% of the variance in the dependent variable (Adjusted R² = 0.23). At the same time, support from friends turned out to be the only significant predictor (Beta = 0.53), and this means that the more support the subjects received from them, the lower the level of depression they manifested.
Conclusions:
1) The better the functional state of a senior and the support received from relatives, the lower the severity of depression. 2) The lower the quality of a senior’s life, especially in terms of mental state, the greater the negative impact on his/her well-being in isolation. 3) The low quality of life of a senior increased the likelihood of depression. 4) The quality of life of older Covid-19 patients was higher in those without chronic disease. 5) The quality-of-life level was lower in patients with a more severe course of COVID-19, and longer duration of disease and oxygen therapy.
FUNDING
The study was financed from the Research Fund of the Jan
Kochanowski University in Kielce, which is intended to
support the continuity and development of the university’s
scientific research.
REFERENCES (50)
1.
Dzieciatkowski T, Szarpak L, Filipiak KJ, Jaguszewski M, Ladny JR, Smereka J. COVID-19 challenge for modern medicine. Cardiol J. 2020; 27(2): 175–183. https://doi.org/10.5603/CJ.a20....
2.
Kulak K, Wieczorek K, Krupski A, Fajfer Z. SARS-CoV-2 as a real threat for healthcare workers. Disaster Emerg Med J. 2020; 5(2): 110–111. https://doi.org/10.5603/DEMJ.a....
3.
Smereka J, Szarpak L. COVID 19 a challenge for emergency medicine and every health care professional. Am J Emerg Med. 2020; 38(10): 2232–2233. https://doi.org/10.1016/j.ajem....
4.
Smereka J, Szarpak L, Filipiak KJ. Modern medicine in COVID-19 era. Disaster Emerg Med J. 2020; 5(2): 103–105. https://doi.org/10.5603/DEMJ.a....
5.
Kulig-Kulesza MD, Sobieraj A, Wojtyczka D, Graca M, Saran A, Kluczewska E. Assessment of the level of COVID-19 anxiety perceived by Internet users and factors affecting its increase at the first stage of the pandemic in Poland. Med Og Nauk Zdr. 2022: 28(2): 142–148. https://doi.org/10.26444/monz/....
6.
Chmielewski JP, Raczek M, Puścion M, Chmielowiec B. Pawlas N, Łuszczki JJ. COVID-19 caused by the SARS-CoV-2 virus as an occupational disease of medical professionals. Med Og Nauk Zdr. 2021; 27(3): 235–243. https://doi.org/10.26444/monz/....
7.
Cascella M, Rajnik M, Aleem A, et al. Features, Evaluation, and Treatment of Coronavirus (COVID-19). In: StatPearls [Internet]. Treasure Island (F.L.): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/b... (Updated: 2022.05.04).
8.
Wróblewska I, Wróblewska Z, Grudzień R, Dziechciarz M, Czabak-Garbacz R, Choina P, Chmielewski J. Post-vaccination reactions occurring in patients vaccinated against SARS-COV-2. Med Og Nauk Zdr. 2021; 27(4): 421–427. https://doi.org/10.26444/monz/....
9.
Li T, Qiu X, Gong X, Zhan R, Zheng X. The cross-sectional survey on COVID-19 vaccine hesitancy and it predictors among Chinese parents of 3–17 years aged children in Shenzhen City. Ann Agric Environ Med. 2022; 29(1): 120–125. https://doi.org/10.26444/aaem/....
10.
Timofeeva AV, Fedorov IS, Chagovets VV, Zubkov VV, Makieva MI, Sugak AB, Frankevich VE, Sukhikh GT. The Impact of Maternal SARS-CoV-2 Infection Next to Pre-Immunization with Gam-COVID-Vac (Sputnik V) Vaccine on the 1-Day-Neonate’s Blood Plasma Small Non-Coding RNA Profile: A Pilot Study. COVID. 2022; 2(7): 837–857. https://doi.org/10.3390/covid2....
11.
Mohapatra RK, Kuppili S, Kumar Suvvari T, Kandi V, Behera A, Verma S, Kudrat-E-Zahan, Biswal SK, Al-Noor TH, El-Ajaily MM, Sarangi AK, Dhama K. SARS-CoV-2 and its variants of concern including Omicron: A never ending pandemic. Chem Biol Drug Des. 2022; 99(5): 769–788. https://doi.org/10.1111/cbdd.1....
12.
Aleem A, Akbar Samad AB, Slenker AK. Emerging Variants of SARS-CoV-2 And Novel Therapeutics Against Coronavirus (COVID-19). In: StatPearls [Internet]. Treasure Island (F.L.): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/b... (Updated: 2022.05.12).
13.
Ahmad FB, Cisewski JA, Minino A, Anderson RN. Provisional Mortality Data – United States, 2020. MMWR Morb Mortal Wkly Rep. 2021; 70(14): 519–522. https://doi.org/10.15585/mmwr.....
14.
Axfors C, Ioannidis JPA. Infection fatality rate of COVID-19 in community-dwelling elderly populations. Eur J Epidemiol. 2022; 37: 235–249. https://doi.org/10.1007/s10654....
15.
Stokes EK, Zambrano LD, Anderson KN, Marder EP, Raz KM, El Burai Felix S, Tie Y, Fullerton KE. Coronavirus Disease 2019 Case Surveillance – United States. MMWR Morb Mortal Wkly Rep. 2020; 69(24): 759–765. https://doi.org/10.15585/mmwr.....
16.
Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020; 11(1): 29. https://doi.org/10.1186/s13293....
17.
Dutkiewicz J, Mackiewicz B, Lemieszek MK. COVID 19 – Possible interrelations with respiratory comorbidities caused by occupational exposure to various hazardous bioaerosols. Part I. Occurrence, epidemiology and presumed origin of the pandemic. Ann Agric Environ Med. 2020; 27(4): 491–504. https://doi.org/10.26444/aaem/....
18.
Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, Agha M, Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. International Journal of Surgery. 2020; 78: 185–193. https://doi.org/10.1016/j.ijsu....
19.
Işik NA, Çelik GK, Ayran G. Turkish validity and reliability of coronavirus anxiety scale. Curr Psychol. 2022; 1–9. https://doi.org/10.1007/s12144....
20.
Lutomski P, Kaczoruk M, Florek-Łuszczki M. Ageing policy in Poland during the COVID-19 pandemic. Ann Agric Environ Med. 2021; 28(4): 551–557. https://doi.org/10.26444/aaem/....
21.
Pandey K, Thurman M, Johnson Samuel D, et al. Mental Health Issues During and After COVID-19 Vaccine Era Brain Res Bull. 2021; 176: 161–173. https://doi.org/10.1016/j.brai....
22.
Wróblewska I, Bartyzel M, Chmielowiec B, Puścion M, Chmielewski JP. The impact of depression on the quality of life in elderly people. Med Og Nauk Zdr. 2021; 27(2): 199–204. https://doi.org/10.26444/monz/....
23.
Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020; 186: 31–34. https://doi.org/10.1016/j.puhe....
24.
Bastiampillai T, Allison S, Looi JCL. Spanish Flu (1918–1920) Impact on U.S. Suicide Rates by Race: Potential Future Effects of the COVID-19 Pandemic. Prim Care Companion CNS Disord. 2021; 23(6): 21com03088. https://doi.org/10.4088/PCC.21....
25.
Koda M, Harada N, Eguchi A, Nomura S, Ishida Y. Reasons for Suicide During the COVID-19 Pandemic in Japan. JAMA Netw Open. 2022; 5(1): e2145870. https://doi.org/10.1001/jamane....
26.
Gotlib J, Rzońca E, Baranowska B, Tataj-Puzyna U, Pawlicka P, Jaworski M, Wójcik-Fatla A, Panczyk M. Is job seniority a protective factor against anxiety among midwives during the SARS-CoV-2 pandemic? Ann Agric Environ Med. 2021; 28(2): 352–357. https://doi.org/10.26444/aaem/....
27.
Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020; 5(5): e256. https://doi.org/10.1016/S2468-....
28.
Di Gennaro F, Pizzol D, Marotta C, Antunes M, Racalbuto V, Veronese N, Smith L. Coronavirus Diseases (COVID-19) Current Status and Future Perspectives: A Narrative Review. Int J Environ Res Public Health. 2020; 17(18): 2690. https://doi.org/10.3390/ijerph....
29.
Ornell F, Schuch JB, Sordi A O, Kessler FHP. “Pandemic fear” and COVID-19: mental health burden and strategies. Braz J Psychiatry. 2020; 42: 232–235. https://doi.org/10.1590/1516-4....
30.
Xiao H, Zhang Y, Kong D, Li S, Yang N. Social Capital and Sleep Quality in Individuals Who Self-Isolated for 14 Days During the Coronavirus Disease 2019 (COVID-19) Outbreak in January 2020 in China. Med Sci Monit. 2020; 26: e923921. https://doi.org/10.12659/MSM.9....
31.
Ustawa z dnia 5 grudnia 2008 r. o zapobieganiu oraz zwalczaniu zakażeń i chorób zakaźnych u ludzi (DzU 2021 poz. 2069). https://isap.sejm.gov.pl/isap.... (Updated: 2022.05.04).
32.
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020; 33(2): e100213. https://doi.org/10.1136/gpsych....
33.
Nowicki GJ, Młynarska M, Ślusarska B, Jabłuszewska K, Bartoszek A, Kocka K, Przybylska-Kuć S. Loneliness as a factor conditioning the quality of life in people over 65. Medycyna Rodzinna. 2018; 3: 208–215. https://doi.org/10.25121/MR.20....
34.
Wojciechowska W. Sense of coherence and psychosocial aspects of the process of ageing as determinants of acceptance and coping with a chronic disease in patients under long-term care. Polish Nursing/Pielegniarstwo Polskie. 2022; 83(1): 11–18. https://doi.org/10.20883/pielp....
35.
Richard-Denis A, Benazet D, Thompson C, Mac-Thiong JM. Determining priorities in functional rehabilitation related to the quality of life one-year following a traumatic spinal cord injury. J Spinal Cord Med. 2018. 1–6. https://doi.org/10.1080/107902....
36.
Ahmad NA, Abd Razak MA, Kassim MS, Sahril N, Ahmad FH, Harith AA, Mahmud NA, Abdul Aziz FA, Hasim MH, Ismail H, Mohd Sidik S. Association between functional limitations and depression among community-dwelling older adults in Malaysia. Geriatr Gerontol Int. 2020; 20(2): 21–25. https://doi.org/10.1111/ggi.14.... PMID: 33370850.
37.
Gariépy G, Honkaniemi H, Quesnel-Vallée A. Social support and protection from depression: a systematic review of current findings in Western countries. Br J Psychiatry. 2016; 209(4): 284–293. https://doi.org/10.1192/bjp.bp....
38.
Tengku Mohd TAM, Yunus RM, Hairi F, Hairi NH,Choo WY. Social support and depression among community-dwelling older adults in Asia: a systematic review. BMJ Open. 2019; 9: e026667. https://doi.org/10.1136/bmjope....
39.
Chruściel P, Kulik T, Jakubowska K, Nalepa D. Differences in the Perception of Social Support Among Rural Area Seniors-A Cross-Sectional Survey of Polish Population. Int J Environ Res Public Health. 2018; 15(6): 1288. https://doi.org/10.3390/ijerph....
40.
Engelen L, Rahmann M, de Jong E. Design for healthy ageing – the relationship between design, well-being, and quality of life: a review. Building Res Information. 2022; 50:1–2, 19–35, https://doi.org/10.1080/096132....
41.
Krägeloh CU, Kersten P, Rex Billington D, Hsien-Chuan Hsu P, Owczarek D, Landon J, Feng XJ. Validation of the WHOQOL-BREF quality of life questionnaire for general use in New Zealand: confirmatory factor analysis and Rasch analysis. Qual Life Res. 2013; 22: 1451–1457. https://doi.org/10.1007/s11136....
42.
Kok RM, Reynolds, CF. Management of Depression in Older Adults. JAMA. 2017; 317(20): 2114. https://doi.org/10.1001/jama.2....
43.
Świtalski J, Dykowska G, Czerw A, Szpakowski R, Fronczak A. Quality of life, functional efficiency and risk of depression among patients staying in selected long-term care facilities–pilot study. Gerontologia Pol. 2018; 26(3): 182–189.
44.
Gerino E, Rolle L, Sechi C, Brustia P. Loneliness, resilience, mental health, and quality of life in old age: A structural equation model. Frontiers in psychology. 2017; 8: 2003. https://doi.org/10.3389/fpsyg.....
45.
Kim B, Hyeyoun Jun H, Jisun Lee J, Yun Min Kim YM. Social Support, Activities of Daily Living, and Depression among Older Japanese and Korean Immigrants in the U.S., Social Work in Public Health. 2020; 35(4): 163–176. https://doi.org/10.1080/193719....
46.
Mahmud NA, Shahein NA, Yoep N, Mahmud MAF, Maw Pin T, Paiwai F, Yusof M, Muhamad NA. Influence of social support on limitation in daily living among older persons in Malaysia. Geriatrics and Gerontology International. 2020; 20(S2): 26–32. https://doi.org/10.1111/ggi.14....
47.
Ruetzler K, Szarpak L, Filipiak KJ, Ladny JR, Smereka J. The COVID-19 pandemic – a view of the current state of the problem. Disaster Emerg Med J. 2020;5(2):106–107. https://doi.org/10.5603/DEMJ.a....
48.
Unalan D, Gocer S, Basturk M, Baydur H, Ozturk A. Coincidence of low social support and high depressive score on quality of life in elderly. European Geriatric Med. 2015; 6(4): 319–324. https://doi.org/10.1016/j.eurg....
49.
Lu C, Yuan L, Lin W, Zhou Y, Pan S. Depression and resilience mediates the effect of family function on quality of life of the elderly. Arch Gerontol Geriatrics. 2017; 71: 34–42. https://doi.org/10.1016/j.arch....
50.
Zhao X, Zhang D, Wu M, Yang Y, Xie H, Li Y, Jia J, Su Y. Loneliness and depression symptoms among the elderly in nursing homes: A moderated mediation model of resilience and social support. Psychiatry Res. 2018: 268: 143–151. https://doi.org/10.1016/j.psyc....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.