Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
The effect of zinc supplementation on the course of COVID-19 – A systematic review and meta-analysis
1
ViaMed Polyclinic, Warsaw, Poland
2
Baylor College of Medicine, Houston (TX), USA
3
Maria Sklodowska-Curie Medical Academy, Warsaw, Poland
4
International European University, Kyiv, Ukraine
5
Institute of Environmental Protection – National Research Institute, Warsaw, Poland
6
Institute of Rural Health, Lublin, Poland
7
University of La Rioja, Spain
8
Polish Society of Disaster Medicine, Warsaw, Poland
9
Medical University, Gdańsk, Poland
10
Jan Dlugosz University, Częstochowa, Poland
Ann Agric Environ Med. 2022;29(4):568-574
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Zinc is a trace element that plays a role in stimulating innate and acquired immunity. The aim of the study was to determine the antiviral effect of the administration of zinc in COVID-19 patients.
Material and methods:
A literature search was performed in P Web of Science, PubMed, Scopus and Cochrane databases from 1 January 2020 – 22 August 2022. In addition, reference lists of the included articles and their related citations in PubMed were also reviewed for additional pertinent studies.
Results:
A total of 9 eligible studies were identified. In-hospital mortality in zinc supplementation patients, and patients treated without zinc, varied and amounted to 21.6% vs. 23.04% difference (OR=0.71; 95%CI: 0.62–0.81; p<0.001). 28-day to 30-day mortality in patients treated with zinc was 7.7%, compared to 11.9% for patients treated without zinc (OR=0.61; 95%CI: 0.35–1.06; p=0.08). In-hospital adverse events among patients treated with and without COVID-19 did not show any statistically significant differences in relation to acute kidney injury occurrence (12.8% vs. 12.4%, respectively; OR=0.63; 95%CI: 0.19–2.12; p=0.45, as well as need for mechanical ventilation (13.2% vs. 14.1%; OR=0.83; 95%CI: 0.52–1.32; p=0.43).
Conclusions:
Zinc supplementation is associated with lower COVID-19 in-hospital mortality. Additionally, it is risk-free in COVID-19 patients since there have been no negative side effects, such as acute renal damage or the requirement for mechanical ventilation compared to patients without COVID-19. Due to scientific evidence and the role it represents in the human body, zinc supplementation should be taken into consideration for COVID-19 patients as an adjunct therapy.
Zinc is a trace element that plays a role in stimulating innate and acquired immunity. The aim of the study was to determine the antiviral effect of the administration of zinc in COVID-19 patients.
Material and methods:
A literature search was performed in P Web of Science, PubMed, Scopus and Cochrane databases from 1 January 2020 – 22 August 2022. In addition, reference lists of the included articles and their related citations in PubMed were also reviewed for additional pertinent studies.
Results:
A total of 9 eligible studies were identified. In-hospital mortality in zinc supplementation patients, and patients treated without zinc, varied and amounted to 21.6% vs. 23.04% difference (OR=0.71; 95%CI: 0.62–0.81; p<0.001). 28-day to 30-day mortality in patients treated with zinc was 7.7%, compared to 11.9% for patients treated without zinc (OR=0.61; 95%CI: 0.35–1.06; p=0.08). In-hospital adverse events among patients treated with and without COVID-19 did not show any statistically significant differences in relation to acute kidney injury occurrence (12.8% vs. 12.4%, respectively; OR=0.63; 95%CI: 0.19–2.12; p=0.45, as well as need for mechanical ventilation (13.2% vs. 14.1%; OR=0.83; 95%CI: 0.52–1.32; p=0.43).
Conclusions:
Zinc supplementation is associated with lower COVID-19 in-hospital mortality. Additionally, it is risk-free in COVID-19 patients since there have been no negative side effects, such as acute renal damage or the requirement for mechanical ventilation compared to patients without COVID-19. Due to scientific evidence and the role it represents in the human body, zinc supplementation should be taken into consideration for COVID-19 patients as an adjunct therapy.
ACKNOWLEDGEMENTS
The study was supported by the ERC Research Net and by the Polish Society of Disaster Medicine.
REFERENCES (61)
1.
Dzieciatkowski T, Szarpak L, Filipiak KJ, et al. COVID-19 challenge for modern medicine. Cardiol J. 2020;27(2):175–183. https://doi.org/10.5603/CJ.a20....
2.
Szarpak L, Pruc M, Nadolny K, et al. Role of a field hospital in COVID-19 pandemic. Disaster Emerg Med J. 2020;5(4):221–223. https://doi.org/10.5603/DEMJ.a....
3.
Chirico F, Sagan D, Markiwicz A, et al. SARS-CoV-2 virus mutation and loss of treatment and preventive measures as we know it now. Disaster Emerg Med J. 2021;6(4):204–205. https://doi.org/10.5603/DEMJ.a....
4.
Pruc M, Gasecka A, Szarpak L, et al. Adverse reactions of COVID-19 vaccination: where do they come from? Disaster Emerg Med J. 2021; 6(1):48–49. https://doi.org/10.5603/DEMJ.a....
5.
Batra K, Effah-Acheampong J, Batra R, et al. Evolution of SARSCoV-2 variants: A rapid literature scan. J Health Soc Sci. 2022;7(2):141–151. https://doi.org/10.19204/2022/....
6.
Gozhenko A, Szarpak L, Jaguszewski MJ, et al. COVID-19 vaccine – third dose, booster dose? What is it and is it necessary? Disaster Emerg Med J. 2021;6(4):208–209. https://doi.org/10.5603/DEMJ.a....
7.
Yaman E, Demirel B, Yimaz A, et al. Retrospective evaluation of laboratory findings of suspected paediatric COVID-19 patients with positive and negative RT-PCR. Disaster Emerg Med J. 2021;6(3):97–103. https://doi.org/10.5603/DEMJ.a....
8.
Katipoğlu B, Öztürk Sönmez L, Vatansev H, et al. Can hematological and biochemical parameters fasten the diagnosis of COVID-19 in emergency departments? Disaster Emerg Med J. 2020;5(4):175–181. https://doi.org/10.5603/DEMJ.a....
9.
Weiss P, Murdoch DR. Clinical course and mortality risk of severe COVID-19. The Lancet. 2020;395(10229):1014–1015. https://doi.org/10.1016/S0140-....
10.
Białorudzki M, Izdebski Z. Changes in the body mass of adult residents of rural and urban areas in the initial months of the COVID-19 pandemic vs. their mental, physical and sexual health. Ann Agric Environ Med. 2021;28(4):667–675. https://doi.org/10.26444/aaem/....
11.
Szarpak L, Zaczynski A, Kosior D, et al. Evidence of diagnostic value of ferritin in patients with COVID-19. Cardiol J. 2020;27(6):886–887. https://doi.org/10.5603/CJ.a20....
12.
Schmidt W, Jóźwiak B, Czabajska Z, et al. On-admission laboratory predictors for developing critical COVID-19 during hospitalization – a multivariable logistic regression model. Ann Agric Environ Med. 2022; 29(2):274–280. https://doi.org/10.26444/aaem/....
13.
Szarpak L, Rafique Z, Gasecka A, et al. A systematic review and meta-analysis of effect of vitamin D levels on the incidence of COVID-19. Cardiol J. 2021;28(5):647–654. https://doi.org/10.5603/CJ.a20....
14.
Fialek B, Pruc M, Smereka J, et al. Diagnostic value of lactate dehydrogenase in COVID-19: A systematic review and meta-analysis. Cardiol J. 2022 Jun 28. https://doi.org/10.5603/CJ.a20....
15.
Mackiewicz B, Lemieszek MK, Dulkiewicz J. COVID 19 – Possible interrelations with respiratory comorbidities caused by occupational exposure to various hazardous bioaerosols. Part II. Clinical course, diagnostics, treatment and prevention. Ann Agric Environ Med. 2021; 28(1):27–43. https://doi.org/10.26444/aaem/....
16.
Frangos T, Maret W. Zinc and cadmium in the aetiology and pathogenesis of osteoarthritis and rheumatoid arthritis. Nutrients. 2020;13(1):53. https://doi.org/10.3390/nu1301....
17.
Hojyo S, Fukada T. Roles of zinc signaling in the immune system. J Immunol Res. 2016;2016:6762343. https://doi.org/10.1155/2016/6....
18.
Iddir M, Brito A, Dingeo G, et al. Strengthening the Immune System and Reducing Inflammation and Oxidative Stress through Diet and Nutrition: Considerations during the COVID-19 Crisis. Nutrients. 2020;12(6):1562. https://doi.org/10.3390/nu1206....
19.
Ibs K-H, Rink L. Zinc-Altered Immune function. J Nutr. 2003; 133(5Suppl 1):1452S–6S. https://doi.org/10.1093/jn/133....
20.
Prasad AS. Lessons learned from experimental human model of zinc deficiency. J Immunol Res. 2020;2020:9207279. https://doi.org/10.1155/2020/9....
21.
Cakman I, Kirchner H, Rink L. Zinc supplementation reconstitutes the production of interferon-α by leukocytes from elderly persons. J Interferon Cytokine Res. 1997;17(8):469–472. https://doi.org/10.1089/jir.19....
22.
Te Velthuis AJ, van den Worm SH, Sims AC, et al. Zn2+ inhibits coronavirus and arterivirus RNA polymerase activity in vitro and zinc ionophores block the replication of these viruses in cell culture. PLoS Pathog. 2010;6(11):e1001176. https://doi.org/10.1371/journa....
23.
Xue J, Moyer A, Peng B, et al. Chloroquine is a zinc ionophore. PLoS One. 2014;9(10):e109180. https://doi.org/10.1371/journa....
24.
Wang J, Mei J, Ren G. Plant microRNAs: biogenesis, homeostasis, and degradation. Front Plant Sci. 2019;10:360. https://doi.org/10.3389/fpls.2....
25.
Boretti A, Banik BK. Zinc role in Covid-19 disease and prevention. Vacunas. 2022;23(2):147–150. https://doi.org/10.1016/j.vacu....
26.
Zheng J, Zhangm XX, Yum H, et al. Zinc at cytotoxic concentrations affects post-transcriptional events of gene expression in cancer cells. Cell Physiol Biochem. 2012;29(1–2):181–188. https://doi.org/10.1159/000337....
27.
Szarpak Ł, Nowak B, Kosior D, et al. Cytokines as predictors of COVID-19 severity: evidence from a meta-analysis. Pol Arch Intern Med. 2021;131(1):98–99. https://doi.org/10.20452/pamw.....
28.
Szarpak L, Pruc M, Gasecka A, et al. Should we supplement zinc in COVID-19 patients? Evidence from a meta-analysis. Pol Arch Intern Med. 2021;131(9):802–807.
30.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n7....
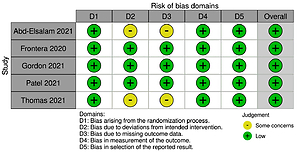
31.
Sterne JAC, Savović J, Page MJ, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. https://doi.org/10.1136/bmj.l4....
32.
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355: i4919. https://doi.org/10.1136/bmj.i4....
33.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments Res Synth Methods. 2021;12(1):55–61. https://doi.org/10.1002/jrsm.1....
34.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. https://doi.org/10.1186/1471-2....
35.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. https://doi.org/10.1136/bmj.32....
36.
Abd-Elsalam S, Soliman S, Esmail ES, et al. Do Zinc Supplements Enhance the Clinical Efficacy of Hy-droxychloroquine?: a Randomized, Multicenter Trial. Biol Trace Elem Res. 2021;199(10):3642–3646. https://doi.org/10.1007/s12011....
37.
Al Sulaiman K, Aljuhani O, Al Shaya D, et al. Evaluation of zinc sulfate as an adjunctive therapy in COVID-19 critically ill patients: a two center propensity-score matched study. Crit Care. 2021;25(1):363. https://doi.org/10.1186/s13054....
38.
Berti AD, Kale-Pradhan PB, Giuliano CA, et al. Clinical Outcomes of Zinc Supplementation Among COVID-19 Patients. Curr Drug Saf. 2022;17(4):366–369. https://doi.org/10.2174/157488....
39.
Carlucci PM, Ahuja T, Petrilli C, et al. Zinc sulfate in combination with a zinc ionophore may improve outcomes in hospitalized COVID-19 patients. J Med Microbiol. 2020;69(10):1228–1234. https://doi.org/10.1099/jmm.0.....
40.
Frontera JA, Rahimian JO, Yaghi S, et al. Treatment with Zinc is Associated with Reduced In-Hospital Mortality Among COVID-19 Patients: A Multi-Center Cohort Study. Res Sq. 2020; rs.3.rs-94509. https://doi.org/10.21203/rs.3.....
41.
Gordon AM, Hardigan PC. A Case-Control Study for the Effectiveness of Oral Zinc in the Prevention and Mitigation of COVID-19. Front Med (Lausanne). 2021;8:756707. https://doi.org/10.3389/fmed.2....
42.
Patel O, Chinni V, El-Khoury J, et al. A pilot double-blind safety and feasibility randomized controlled trial of high-dose intravenous zinc in hospitalized COVID-19 patients. J Med Virol. 2021;93(5):3261–3267. https://doi.org/10.1002/jmv.26....
43.
Thomas S, Patel D, Bittel B, et al. Effect of High-Dose Zinc and Ascorbic Acid Supplementation vs Usual Care on Symptom Length and Reduction Among Ambulatory Patients With SARS-CoV-2 Infection: The COVID A to Z Randomized Clinical Trial. JAMA Netw Open. 2021; 4(2):e210369. https://doi.org/10.1001/jamane....
44.
Yao JS, Paguio JA, Dee EC, et al. The Minimal Effect of Zinc on the Survival of Hospitalized Patients With COVID-19: An Observational Study. Chest. 2021;159(1):108–111. https://doi.org/10.1016/j.ches....
45.
Jothimani D, Kailasam E, Danielraj S, et al. COVID-19: Poor outcomes in patients with zinc deficiency. Int J Infect Dis. 2020;100:343–349. https://doi.org/10.1016/j.ijid....
46.
Ghanei E, Baghani M, Moravvej H, et al. Low serum levels of zinc and 25-hydroxyvitmain D as potential risk factors for COVID-19 susceptibility: a pilot case-control study. Eur J Clin Nutr. 2022;76(9): 1297–1302. https://doi.org/10.1038/s41430....
47.
Ali N, Fariha KA, Islam F, et al. Assessment of the role of zinc in the prevention of COVID-19 infections and mortality: A retrospective study in the Asian and European population. J Med Virol. 2021; 93(7): 4326–4333. https://doi.org/10.1002/jmv.26....
48.
Devaux CA, Rolain J-M, Raoult D. ACE2 receptor polymorphism: susceptibility to SARS-CoV-2, hyper-tension, multi-organ failure, and COVID-19 disease outcome. J Microbiol Immunol Infect. 2020;53(3): 425–435. https://doi.org/10.1016/j.jmii....
49.
Szarpak L, Pruc M, Gasecka A, et al. Should we supplement zinc in COVID-19 patients? Evidence from a me-ta-analysis. Pol Arch Intern Med. 2021;131(9):802–807. https://doi.org/10.20452/pamw.....
50.
Tabatabaeizadeh SA. Zinc supplementation and COVID-19 mortality: a meta-analysis. Eur J Med Res. 2022;27(1):70. https://doi.org/10.1186/s40001....
51.
Hunter J, Arentz S, Goldenberg J, et al. Zinc for the prevention or treatment of acute viral respiratory tract infections in adults: a rapid systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2021;11(11):e047474. https://doi.org/10.1136/bmjope....
52.
Vlieg-Boerstra B, de Jong N, Meyer R, et al. Nutrient supplementation for prevention of viral respiratory tract infections in healthy subjects: A systematic review and meta-analysis. Allergy. 2022;77(5):1373–1388. https://doi.org/10.1111/all.15....
53.
Beran A, Mhanna M, Srour O, et al. Clinical significance of micronutrient supplements in patients with coronavirus disease 2019: A comprehensive systematic review and meta-analysis. Clin Nutr ESPEN. 2022;48:167–177. https://doi.org/10.1016/j.clne....
54.
Alexander J, Tinkov A, Strand TA, et al. Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19. Nutrients. 2020;12(8):2358. https://doi.org/10.3390/nu1208....
55.
Pal A, Squitti R, Picozza M, et al. Zinc and COVID-19: Basis of Current Clinical Trials. Biol Trace Elem Res. 2021;199(8):2882–2892. https://doi.org/10.1007/s12011....
56.
Eftekhar SP, Kazemi S, Barary M, et al. Effect of Hydroxychloroquine and Azithromycin on QT Interval Prolongation and Other Cardiac Arrhythmias in COVID-19 Confirmed Patients. Cardiovasc Ther. 2021; 2021:6683098. https://doi.org/10.1155/2021/6....
57.
Pecora F, Persico F, Argentiero A, Neglia C, Esposito S. The Role of Micronutrients in Support of the Immune Response against Viral Infections. Nutrients. 2020;12(10):3198. https://doi.org/10.3390/nu1210....
58.
Im JH, Je YS, Baek J, Chung MH, Kwon HY, Lee JS. Nutritional status of patients with COVID-19. Int J Infect Dis. 2020 Nov;100:390–393. doi: 10.1016/j.ijid.2020.08.018.
59.
Fosmire GJ. Zinc toxicity. Am J Clin Nutr. 1990;51(2):225–227. https://doi.org/10.1093/ajcn/5....
60.
Meng-Yuan Li, Lin Li, Zhang Yeu, Xiao-Sheng Wang. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020;9(1):45. https://doi.org/10.1186/s40249....
61.
Duncan A, Yacoubian C, Watson N, Morrison I. The risk of copper deficiency in patients prescribed zinc supplements. J Clin Pathol. 2015; 68(9):723–725. https://doi.org/10.1136/jclinp....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.