Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Gender gap in health condition and quality of life at advanced age
1
Institute of Statistics and Demography, Collegium of Economic Analysis, SGH Warsaw School of Economics, Warsaw, Poland
2
Department of Pharmacology and Toxicology, Faculty of Medicine and Health Sciences, University of Zielona Góra, Poland
3
National Institute of Geriatrics, Rheumatology and Rehabilitation, Warsaw, Poland
4
Department of Internal Medicine, Faculty of Medicine and Health Sciences, University of Zielona Góra, Poland
5
Department of Women’s Health, Institute of Rural Health, Lublin, Poland
Corresponding author
Iwona Bojar
Department of Women’s Health, Institute of Rural Health, Jaczewskiego 2, 20-090, Lublin, Poland
Department of Women’s Health, Institute of Rural Health, Jaczewskiego 2, 20-090, Lublin, Poland
Ann Agric Environ Med. 2020;27(4):636-643
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Increased life expectancy, share of the very old in populations and differences in the prevalence or types of health problems between male and female seniors pose challenges for health and social care systems in providing adequate care.
Objective:
The aim of the study is to compare the health condition and quality of life between women and men aged 90 or over, as well as to correlate the quality of life at advanced age with demographic and health conditions.
Material and methods:
The study was conducted in Poland in 2015–2018 on 870 women and 264 men aged 90 or over who were able to communicate logically and had no dementia diagnosed previously by a physician. The author’s questionnaire, Katz Index of Independence in Activities of Daily Living, Abbreviated Mental Test Score and WHO Quality of Life-Bref questionnaires were used.
Results:
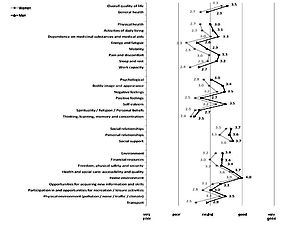
The women aged 90 or over had a significantly higher prevalence of chronic pain (76% vs 60%), urinary incontinence (60% vs 44%), falls and syncopes (39% vs 25%), stool incontinence (17% vs 9%), more severe functional and cognitive impairment and lower quality of life than men at the same age. City residence, being widowed, chronic pain, geriatric giants and functional impairment were factors found to decrease all aspects of the life quality, while age in the studied interval decreased only physical health’ assessment. Lack of education only affected negatively psychological health while cognitive impairment decreased the assessment of physical and psychological health, as well as social relationships.
Conclusions:
Men who reached the age of 90 or over assessed their health condition and quality of life better than women at the same age.
Increased life expectancy, share of the very old in populations and differences in the prevalence or types of health problems between male and female seniors pose challenges for health and social care systems in providing adequate care.
Objective:
The aim of the study is to compare the health condition and quality of life between women and men aged 90 or over, as well as to correlate the quality of life at advanced age with demographic and health conditions.
Material and methods:
The study was conducted in Poland in 2015–2018 on 870 women and 264 men aged 90 or over who were able to communicate logically and had no dementia diagnosed previously by a physician. The author’s questionnaire, Katz Index of Independence in Activities of Daily Living, Abbreviated Mental Test Score and WHO Quality of Life-Bref questionnaires were used.
Results:
The women aged 90 or over had a significantly higher prevalence of chronic pain (76% vs 60%), urinary incontinence (60% vs 44%), falls and syncopes (39% vs 25%), stool incontinence (17% vs 9%), more severe functional and cognitive impairment and lower quality of life than men at the same age. City residence, being widowed, chronic pain, geriatric giants and functional impairment were factors found to decrease all aspects of the life quality, while age in the studied interval decreased only physical health’ assessment. Lack of education only affected negatively psychological health while cognitive impairment decreased the assessment of physical and psychological health, as well as social relationships.
Conclusions:
Men who reached the age of 90 or over assessed their health condition and quality of life better than women at the same age.
Raczkiewicz D, Bejga P, Owoc J, Witczak M, Bojar I. Gender gap in health condition and quality of life at advanced age. Ann Agric Environ Med.
2020; 27(4): 636–643. doi: 10.26444/aaem/125753
REFERENCES (43)
1.
European Commission. The 2012 Ageing Report – Economic and budgetary projections for 27 EU Member States (2010–2060). European Economy 2/2012. ec.europa.eu/economy_finance /publications/../ee- 2012.
2.
Healthy life years, life expectancy statistics. Eurostat 2018. http://appsso.eurostat.ec.euro....
3.
Thomas PA. Gender, social engagement, and limitations in late life. Social Science & Medicine Volume 2011; 73(9): 1428–143.
4.
Health at a Glance: Europe – Life expectancy and healthy life expectancy at birth, OECD iLibrary 2012: Statistics, www.oecdbetterlifeindex.org/…/united-kingdom/2012.
5.
Life expectancy at birth, male, females (years). World Bank 2018. https://data.worldbank.org/ind....
6.
Sundberg L, Agahi N, Fritzell J, Fors S. Why is the gender gap in life expectancy decreasing? The impact of age- and cause-specific mortality in Sweden 1997–2014. Int J Public Health 2018; 63(6): 673–681. doi: 10.1007/s00038-018-1097-3.
7.
Luy M, Wegner-Siegmundt C. The impact of smoking on gender differences in life expectancy: more heterogeneous than often stated. Eur J Public Health 2015; 25: 706–710. doi: 10.1093/eurpub/cku211.
8.
Austad SN. Sex differences in health and aging: a dialog between the brain and gonad? GeroScience 2019; 41: 267–273.
9.
Zhang Y, Wu L, Wang Y, Zhang M, Li L, Zhu D. et al. Protective Role of Estrogen-induced miRNA-29 Expression in Carbon Tetrachloride-induced Mouse Liver Injury. The Journal of Biological Chemistry 2012; 287: 14851–14862. doi: 10.1074/jbc.M111.314922.
10.
Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med 2012; 55: 163–170. doi: 10.1016/j.ypmed.2012.06.017.
11.
Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biology of Sex Differences 2017; 8(33): 1–16.
12.
Kulik TB, Janiszewska M, Piróg E, Pacian A, Stefanowicz A, Żołnierczuk-Kieliszczek D. et al. Sytuacja zdrowotna osób starszych w Polsce i innych krajach europejskich [The health situation of older people in Poland and other European countries]. Medycyna Ogólna i Nauki o Zdrowiu [General Medicine and Health Science] 2011; 17(2): 90–95 (in Polish).
13.
Sytuacja demograficzna osób starszych i konsekwencje starzenia się ludności Polski w świetle prognozy na lata 2014–2050. Główny Urząd Statystyczny, Warszawa, 2014.
14.
Pinkas J, Gujski M, Humeniuk E, Raczkiewicz D, Bejga P, Owoc A, et al. State of health and quality of life of women at advanced age. Medical Science Monitor 2016; 22: 3095–3105.
15.
Shelkey M, Wallace M. Katz index of independence in activities of daily living (ADL). Try this, Best Practices in Nursing Care to Older Adults International Journal of Older People; Issue Number 2, Revised 2012.
16.
Romanik W, Łazarewicz M. The Polish version of the Abbreviated Mental Test Score (AMTS) – methodology issues. Psychiatr Psychol Klin 2017; 17(3): 203–207. doi: 10.15557/PiPK.2017.0024.
17.
Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res 2004; 13: 299–310.
18.
Piniero-Rodriges M.A, Facchini A, Thume E, Maia F. Gender and incidence of functional disability in the elderly: a systematic review. Cadernos de Saude Publica 2009; 25(3): 464–476.
19.
European Year for Active Ageing and Intergenerational Solidarity 2012. European Parliament 2011, www.europarl.europa.eu/news/pl/news-room/content/20110314IPR15479012.
20.
Luo Y, Hawkley LC, Waite LJ, & Cacioppo JT. Loneliness, health, and mortality in old age: A national longitudinal study. Soc Sci Med. 2012; 74: 907–914. doi: 10.1016/j.socscimed.2011.11.028.
21.
Sytuacja demograficzna osób starszych i konsekwencje starzenia się ludności Polski w świetle prognozy na lata 2014–2050 [Demographic situation of the elderly and consequences of the aging of the Polish population according to the forecast for 2014–2050], Central Statistical Office in Poland, Warsaw 2014 (in Polish).
22.
Noei H, Sahaf R, et al. The Relationship between gender and disability in the eldery people in Tehran municipality pension organization. Iranian Journal of Ageing 2017; 12(1): 6–15.
23.
Winkler P, Pochobradsky E, Wirl Ch. Gesundheit und Krankheit der älteren Generation in Österreich [Health and disease of the older generation in Austria]. Wien 2012 (in German).
24.
Mossakowska M, Więcek A, Błędowski P. Aspekty medyczne, psychologiczne, socjologiczne i ekonomiczne starzenia się ludzi w Polsce – Polsenior. Część 1. Rozdział 4. Przebieg badania – Badania dodatkowe [Medical, psychological, sociological and economic aspects of the aging of people in Poland – Polsenior – Part 1. Chapter 4. The course of the study – Additional tests]. Termedia Wydawnictwa Medyczne Poznań 2012 (in Polish).
25.
Głowacka M, Mitura K, Kornatowski T, Haor B, Zabielska P, Biercewicz M, et al. Mental capacity of elderly people according to the AMTS as shown on the example of nursing home residents. Gerontologia Polska 2017; 25: 223–228.
26.
Slusarska B, Nowicki GJ, Bartoszek A, Wittwer S, Zboina B, Naylor K. Health problems of the elderly aged 65–75 years supervised community nurse. Gerontologia Polska 2016; 24: 17–25.
27.
Kim JL, Park JH, KimBJ, Kim MD. Interactive influences of demographics on the Mini-Mental State Examination (MMSE) and the demographics-adjusted norms for MMSE in elderly Koreans. International Psychogeriatrics 2011; 24(4): 642–650.
28.
Connolly A, Gaehl E, Martin H, Morris J, Purandare N. Underdiagnosis of dementia in primary care: variations in the observed prevalence and comparisons to the expected prevalence. Aging Ment Health. 2011; 15(8): 978–984. doi: 10.1080/13607863.2011.596805.
29.
Jitapunkul S, Chansirikanjana S, Thamarpirat J. Undiagnosed dementia and value of serial cognitive impairment screening in developing countries: A population-based study. Geriatr Gerontol Int. 2009; 9: 47–53.
30.
Lang L, Clifford A, Wei L, Zhang D, Leung D, Augustine G, Danat IM, Zhou W, Copeland JR, Anstey KJ, Chen R. Prevalence and determinants of undetected dementia in the community: a systematic literature review and a meta-analysis. BMJ Open. 2017 Feb 3; 7(2): e011146. doi: 10.1136/bmjopen-2016-011146.
31.
Inouye SK, Studenski S, Tinetti ME, & Kuszel GA. Geriatric Syndromes: Clinical Research and Policy Implications of a Core Geriatric Concept. Journal of American Geriatric Society 2007; 55(5): 780–791.
32.
Cruz-Jentoft AJ, Landi F, Topinkova E. Understanding sarcopenia as a geriatric syndrome. Current Opinion in Clinical Nutrition Metabolic Care 2010; 13(1): 1–7.
33.
Foley AL, Loharuka S, Barrett JA, Mathews R, Williams K, McGrother CW. Association between the Geriatric Giants of urinary incontinence and falls in older people using data from the Leicestershire MRC Incontinence Study. Age and Ageing Jan 2012; 41(1): 35–40. doi: 10.1093/ageing/afr125.
34.
Kamińska MS, Brodowski J, Karakiewicz B. Fall Risk Factors in Community-Dwelling Elderly Depending on Their Physical Function, Cognitive Status and Symptoms of Depression. Int J Environ Res Public Health. 2015: 12(4): 3406–3416. doi: 10.3390/ijerph120403406.
35.
Talarska D, Kropińska S, Strugała M, Szewczyczak M, Tobis S, Wieczorowska-Tobis K. The most common factors hindering the independent functioning of the elderly at home by age and sex. European Review for Medical and Pharmacological Sciences 2017; 21: 775–785.
36.
Mane AB, Sanjana T, Patil PR, Sriniwas T. Prevalence and correlates of fear of falling among elderly population in urban area of Karnataka, India. J Midlife Health. 2014 Jul-Sep; 5(3): 150–155.
37.
Shiran Z, Moyes S, McLean C, Serchfield G, Welch D, Jacobs R, et al. Self-reported hearing, vision and quality of life: older people in New Zealand. Australian Asian Journal of Ageing 2016; 35(2): 98–105.
38.
Burzyńska M, Kępa M, Bryła M, Maniecka-Bryła I. Samoocena stanu zdrowia i zachowań zdrowotnych starszych mieszkańców wsi [Self-assessment of health status and health behaviours of older rural inhabitants]. In P. Szukalski (Ed). Starzenie się ludności a solidarność międzypokoleniowa [Aging of the population and intergenerational solidarity] (pp.181–195). University of Lodz 2014 (in Polish).
39.
Keevil LV, Romero-Ortuno R. Ageing well: a review of sarcopenia and frailty. Proceedings of the Nutrition Society 2015; 74(4): 337–347.
40.
Quality of Life in Urban and Rural Europe. European Foundation for the Improvement of Living and Working Conditions. EUROFOUND. Cornell University ILR School 2014 https://digitalcommons.ilr.cor....
41.
Silverstein M, Parker MG. Leisure Activities and Quality of Life among the Oldest Old in Sweden. Research on Ageing 2012. https://doi.org/10.1177/016402....
42.
Begg S.J. Health in a ‘post-transition’ Australia: adding years to life or life to years? Australian Health Review 2013; 38(1): 1–5.
43.
Struktura ludności według wieku w latach 1970–2050. Główny Urząd Statystyczny. https://stat.gov.pl/obszary-te....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.