Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Effects of a Lactobacillus salivarius probiotic short-term intervention on S. mutans, Lactobacillus spp. and C. albicans – a randomized pilot study with pre-school
children
1
Department of Developmental Age Dentistry, Institute of Dentistry, Jagiellonian University Medical College, Kraków, Poland
2
Faculty of Biology, Laboratory of Athopology, Instute of Zoology and Biomedical Research, Kraków,Poland
3
Witold Chodzko Institute of Rural Health, Lublin, Poland
These authors had equal contribution to this work
Corresponding author
Iwona Gregorczyk-Maga
Department of Developmental Age Dentistry, Institute of Dentistry, Jagiellonian University Medical College, Krakow, Poland (2019), Institute of Dentistry, Jagiellonian University Medical College, Krakow, Poland (2019), Poland
Department of Developmental Age Dentistry, Institute of Dentistry, Jagiellonian University Medical College, Krakow, Poland (2019), Institute of Dentistry, Jagiellonian University Medical College, Krakow, Poland (2019), Poland
KEYWORDS
TOPICS
- Health effects of chemical pollutants in agricultural areas , including occupational and non-occupational effects of agricultural chemicals (pesticides, fertilizers) and effects of industrial disposal (heavy metals, sulphur, etc.) contaminating the atmosphere, soil and water
- Prevention of occupational diseases in agriculture, forestry, food industry and wood industry
- State of the health of rural communities depending on various factors: social factors, accessibility of medical care, etc.
ABSTRACT
Introduction and objective:
The aim of the study is to evaluate the effect of short-term, oral supplementation of non-viable Lactobacillus salivarius (HM6 Paradens) on the number of caries-related microorganisms in the supragingival plaque biofilm of pre-school children.
Material and methods:
The study is prospective, randomized and observational in design performed on 2 parallel groups (test and control) of 72 childrenaged between 3 – 6 years, with or without early childhood caries (ECC). The primary outcomes measured are changes in S. mutans counts (number of colony-forming units – CFU) and the percent of the total viable counts) in dental plaque biofilm within the groups between baseline and 2-weeks follow-up, while secondary outcomes are changes in Lactobacilli spp. and C. albicans counts.
Results:
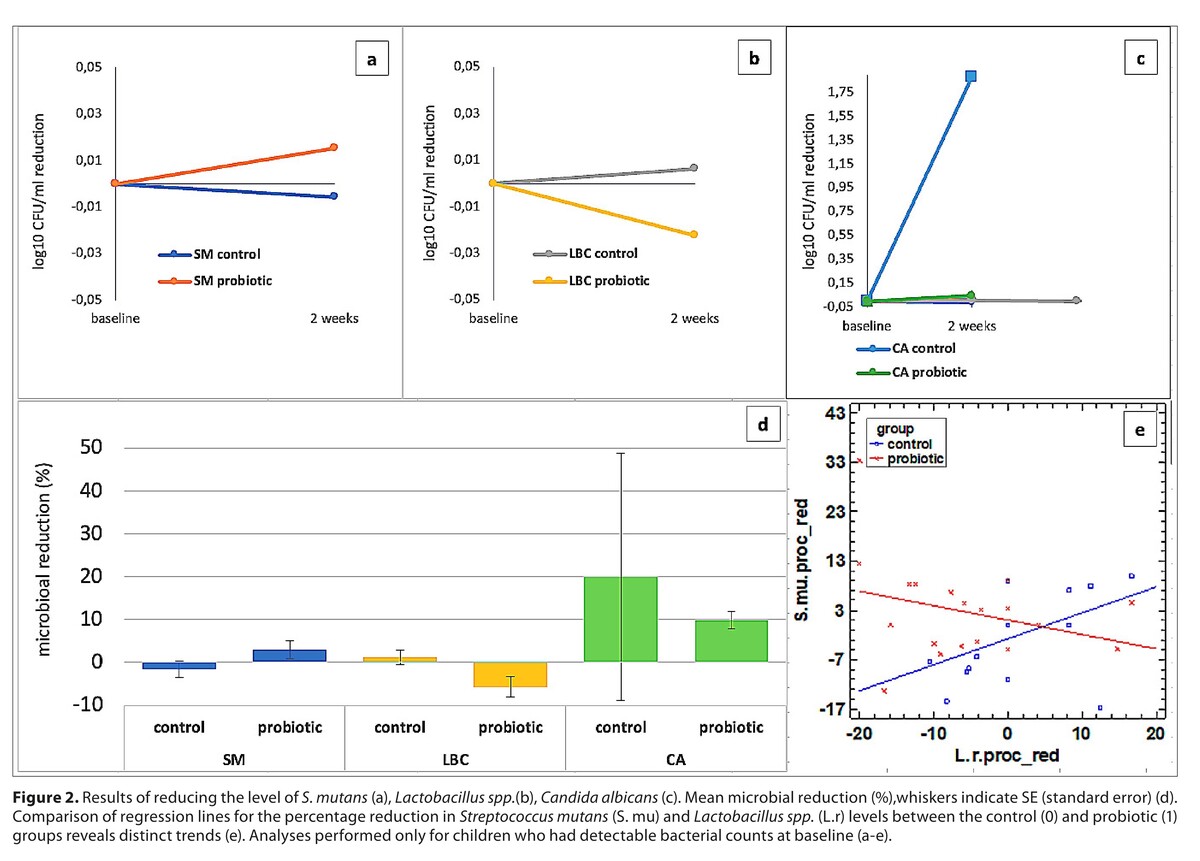
For analysis performed only on the children with detectable bacterial counts at baseline, the reduction in the level of S. mutans increased in the control group, and decreased in the probiotic group, Lactobacillus spp. increased in the probiotic group and decreased in the control group, and for C. albicans, the level decreased in both the control and probiotic groups after 2 weeks.
Conclusions:
The presence of L.salivarius (HM6 Paradens) may modify the interactions between S. mutans and Lactobacillus spp., which could support microbiological homeostasis and have a beneficial impact on ECC prevention.
The aim of the study is to evaluate the effect of short-term, oral supplementation of non-viable Lactobacillus salivarius (HM6 Paradens) on the number of caries-related microorganisms in the supragingival plaque biofilm of pre-school children.
Material and methods:
The study is prospective, randomized and observational in design performed on 2 parallel groups (test and control) of 72 childrenaged between 3 – 6 years, with or without early childhood caries (ECC). The primary outcomes measured are changes in S. mutans counts (number of colony-forming units – CFU) and the percent of the total viable counts) in dental plaque biofilm within the groups between baseline and 2-weeks follow-up, while secondary outcomes are changes in Lactobacilli spp. and C. albicans counts.
Results:
For analysis performed only on the children with detectable bacterial counts at baseline, the reduction in the level of S. mutans increased in the control group, and decreased in the probiotic group, Lactobacillus spp. increased in the probiotic group and decreased in the control group, and for C. albicans, the level decreased in both the control and probiotic groups after 2 weeks.
Conclusions:
The presence of L.salivarius (HM6 Paradens) may modify the interactions between S. mutans and Lactobacillus spp., which could support microbiological homeostasis and have a beneficial impact on ECC prevention.
FUNDING
This research was funded by the Jagiellonian
University Medical College, Kraków Poland (Grant No. K/
ZDS/007912, N41/DBS/000164 and N41/DBS/000662).
REFERENCES (25)
1.
Phantumvanit P, Makino Y, Ogawa H, et al. WHO Global Consultation on Public Health Intervention against Early Childhood Caries. Community Dent Oral Epidemiol. 2018;46:280–287. doi:10.1111/cdoe.12362.
2.
Twetman S. Prevention of dental caries as a non-communicable disease. Eur J Oral Sci. 2018;126:19–25. doi:10.1111/eos.12528.
3.
Pitts N, Tagami T, Weintraub, et al. Dental caries. Nat Rev Dis Primers. 2017;3:17030.
4.
Hajishengallis E, Parsaei Y, Klein MI, et al. Advances in the microbial etiology and pathogenesis of early childhood caries. Mol Oral Microbiol. 2017;32:24–34. doi:10.1111/omi.12152.
5.
Lemos JA, Palmer SR, Zeng L, et al. The Biology of Streptococcus mutans. Microbiol Spectr. 2019;7:10. doi:10.1128/microbiolspec.GPP3-0051-2018.
6.
Pereira D, Seneviratne CJ, Koga-Ito CY, et al. Is the oral fungal pathogen Candida albicans a cariogen? Oral Dis. 2018;24(4):518–526.
7.
Xiao J, Huang X, Alkhers, et al. Candida albicans and early childhood caries: a systematic review and meta-analysis. Caries Res. 2018;52(1–2):102–112.
8.
Xiao J, Grier A, Faustoferri RC, et al. Association between Oral Candida and Bacteriome in Children with Severe ECC. J Dent Res. 2018;97(13):1468–1476. doi:10.1177/0022034518790941.
9.
A Collaborative Effort of the American Academy of Pedodontics and the American Academy of Pediatrics. Policy on early childhood caries(ECC): classifications, consequences, and preventive strategies. Pediatr Dent. 2016;38:52–54.
10.
Shi J, Wang Q, Ruan G, et al. Efficacy of probiotics against dental caries in children: a systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2023;63(29):9977–9994. doi:10.1080/10408398.2022.2077693.
11.
Luo SC, Wei SM, Luo XT, et al. How probiotics, prebiotics, synbiotics, and postbiotics prevent dental caries: an oral microbiota perspective. NPJ Biofilms Microbiomes. 2024;10(1):14. doi:10.1038/s41522-024-00488-7.
12.
Huang X, Bao J, Yang M, et al. The role of Lactobacillus plantarum in oral health: a review of current studies. J Oral Microbiol. 2024;22:2411815. doi:10.1080/20002297.2024.2411815.
13.
Nishihara T, Suzuki N, Yoneda M, et al. Effects of Lactobacillus salivarius-containing tablets on caries risk factors: A randomized open-label clinical trial. BMC Oral Health. 2014;14:110.
14.
Sañudo AI, Luque R, Díaz-Ropero M.P, et al. In vitro and in vivo anti-microbial activity evaluation of inactivated cells of Lactobacillus salivarius CECT 5713 against Streptococcus mutans. Arch Oral Biol. 2017; 84:58–63. doi:10.1016/j.archoralbio.2017.09.014.
15.
Krzyściak W, Kościelniak D, Papież M, et al. Effect of a Lactobacillus Salivarius Probiotic on a Double-Species Streptococcus Mutans and Candida Albicans Caries Biofilm. Nutrients. 2017;9:11. doi:10.3390/nu9111242.
16.
Hansson L, Hedner T, Dahlöf B. Prospective randomized open blinded end-point (PROBE) study. A novel design for intervention trials. Blood Press. 1992;1(2):113–9. doi:10.3109/08037059209077502.
18.
Szczeklik K, Owczarek D, Cibor D, et al. Relative homogeneity of oral bacterial flora in Crohn’s disease compared to ulcerative colitis and its connections with antioxidant defense-Preliminary report. Folia Med. Crac. 2019;59:15–35.
19.
Jussiaux F, Miot-Sertier C, Nguyen-Lopez D, et al. Reliability of MALDI-TOF mass spectrometry to identify oral isolates of Streptococcus salivarius and Lactobacillus spp. Arch Oral Biol. 2021;121:104983. doi:10.1016/j.archoralbio.2020.104983.
20.
Meurman JH, Stamatova IH, Probiotics: Evidence of Oral Health Implications. Folia Med (Plovdiv). 2018;60:21–29. doi:10.1515/folmed-2017-0080.
21.
Gruner D, Paris S, Schwendicke F. Probiotics for managing caries and periodontitis: Systematic review and meta-analysis. J Dent. 2016;48:16–25. doi:10.1016/j.jdent.2016.03.002.
22.
Sivamaruthi BS, Kesika P, Chaiyasut C. A Review of the Role of Probiotic Supplementation in Dental Caries. Probiotics and antimicrobial proteins. 2020;12(4):1300–1309. https://doi.org/10.1007/s12602....
23.
Zare J, Amerian A, E Basir L, et al. Effects of the Consumption of Probiotic Yogurt Containing Bifidobacterium lactis Bb12 on the Levels of Streptococcus mutans and Lactobacilli in Saliva of Students with Initial Stages of Dental Caries: A Double-Blind Randomized Controlled Trial. Caries Res. 2020;54:68–74.
24.
Olczak-Kowalczyk D, Gozdowski D, Turska-Szybka A. Protective Factors for Early Childhood Caries in 3-Year-Old Children in Poland. Front Pediatr. 2021;9:583660. doi:10.3389/fped.2021.583660.
25.
Patil RU, Dastoor PP, Unde MP. Comparative evaluation of antimicrobial effectiveness of probiotic milk and fluoride mouthrinse on salivary Streptococcus mutans counts and plaque scores in children – An in vivo experimental study. J Indian Soc Pedod Prev Dent. 2019;37(4):378–382. doi:10.4103/JISPPD.JISPPD_45_19.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.