Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Can cannabidiol (CBD) help with low back pain?
1
Department of Medical Chemistry, Medical University, Lublin, Poland
2
Department and Clinic of Neurosurgery and Pediatric Neurosurgery, Medical University, Lublin, Poland
Corresponding author
Bartłomiej Kulesza
Department of Medical Chemistry, Medical University, Lublin, Chodźki 4a (Collegium Pharmaceuticum), 20-093, Lublin, Poland
Department of Medical Chemistry, Medical University, Lublin, Chodźki 4a (Collegium Pharmaceuticum), 20-093, Lublin, Poland
Ann Agric Environ Med. 2023;30(3):549-554
KEYWORDS
TOPICS
- Biological agents posing occupational risk in agriculture, forestry, food industry and wood industry and diseases caused by these agents (zoonoses, allergic and immunotoxic diseases)
- Work-related accidents and injuries in agriculture, forestry, food industry and wood industry: incidence, causes, social aspects and prevention
- State of the health of rural communities depending on various factors: social factors, accessibility of medical care, etc.
ABSTRACT
Introduction and objective:
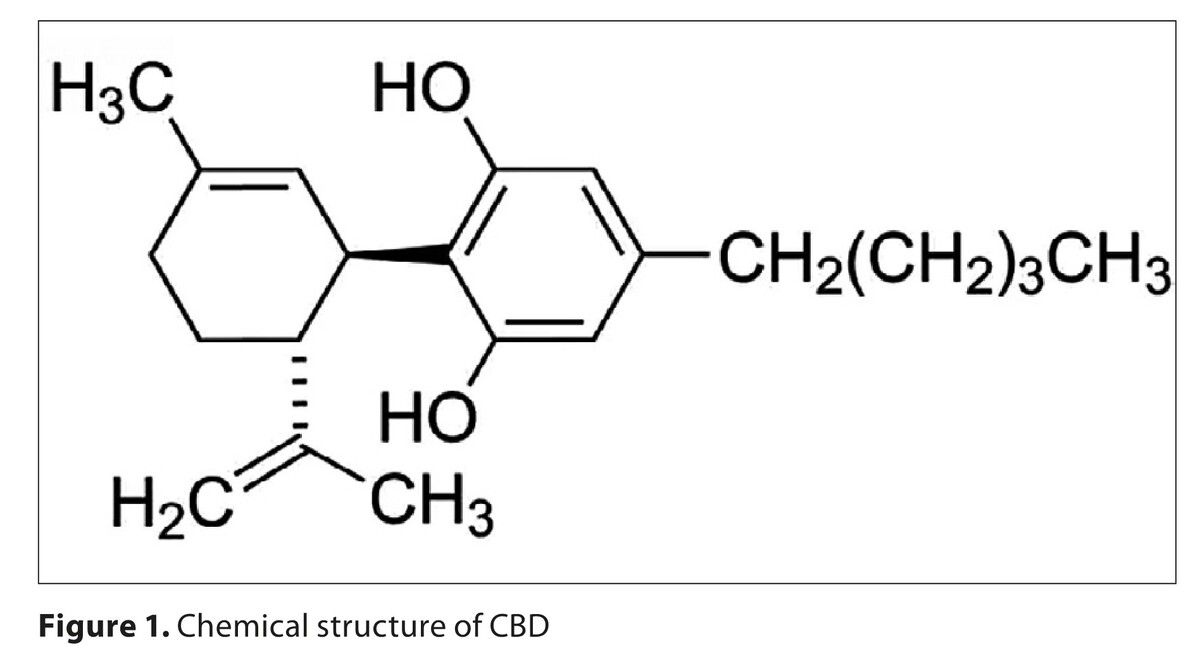
Low back pain (LBP) is a major cause of disability and the main reason why individual patients need medical attention. Pharmacological treatment options for LBP are limited and are often associated with serious side-effects. This makes it necessary to search for new painkillers. One potential therapeutic agent is cannabidiol (CDB). Cannabidiol and tetrahydrocannabinol are the most researched components of cannabis, the plant more commonly known as marijuana or hemp. To the best of our knowledge, this is the first narrative review of the effects of CBD alone on acute and chronic back pain.
Review methods:
Based on the guidelines provided by the Primary Reporting Items for Systematic Reviews and Meta-Analyses Statement (PRISMA), the PubMed/ MEDLINE database was used to identify articles for analysis from the last 30 years. Due to the limited number of studies on this topic, all types of studies that met the inclusion criteria were included. After analysis, 10 studies were included in this review.
Brief description of the state of knowledge:
Currently, the use of medical marijuana continues to increase and the Food and Drug Administration (FDA) has already approved four cannabis-based drugs. Cannabidiol (CBD) is a relatively safe substance for humans and generally well tolerated. It is a substance that is easily available and often taken by patients with LBP.
Summary:
Evidence for the effectiveness of CBD in the treatment of acute low back pain is lacking. There was only one clinical trial conducted in the Emergency Department that showed no superiority of CBD over placebo in acute LBP. The majority of studies concern chronic rather than acute LBP. Although most of the results suggest a beneficial effect of cannabinoids in relieving chronic LBP, hard evidence is lacking. Rigorous randomized controlled trials are needed.
Low back pain (LBP) is a major cause of disability and the main reason why individual patients need medical attention. Pharmacological treatment options for LBP are limited and are often associated with serious side-effects. This makes it necessary to search for new painkillers. One potential therapeutic agent is cannabidiol (CDB). Cannabidiol and tetrahydrocannabinol are the most researched components of cannabis, the plant more commonly known as marijuana or hemp. To the best of our knowledge, this is the first narrative review of the effects of CBD alone on acute and chronic back pain.
Review methods:
Based on the guidelines provided by the Primary Reporting Items for Systematic Reviews and Meta-Analyses Statement (PRISMA), the PubMed/ MEDLINE database was used to identify articles for analysis from the last 30 years. Due to the limited number of studies on this topic, all types of studies that met the inclusion criteria were included. After analysis, 10 studies were included in this review.
Brief description of the state of knowledge:
Currently, the use of medical marijuana continues to increase and the Food and Drug Administration (FDA) has already approved four cannabis-based drugs. Cannabidiol (CBD) is a relatively safe substance for humans and generally well tolerated. It is a substance that is easily available and often taken by patients with LBP.
Summary:
Evidence for the effectiveness of CBD in the treatment of acute low back pain is lacking. There was only one clinical trial conducted in the Emergency Department that showed no superiority of CBD over placebo in acute LBP. The majority of studies concern chronic rather than acute LBP. Although most of the results suggest a beneficial effect of cannabinoids in relieving chronic LBP, hard evidence is lacking. Rigorous randomized controlled trials are needed.
REFERENCES (70)
1.
Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006;332(7555):1430–1434. https://doi.org/10.1136/bmj.33....
2.
Mattiuzzi C, Lippi G, Bovo C. Current epidemiology of low back pain. J Hosp Manag Health Policy 2020;4:15 https://jhmhp.amegroups.com/ar....
3.
Ehrlich GE. Low back pain. Bull World Health Organ. 2003;81(9):671–676. https://apps.who.int/iris/hand....
4.
Atlas SJ, Deyo RA. Evaluating and managing acute low back pain in the primary care setting. J Gen Intern Med. 2001;16(2):120–131. https://doi.org/10.1111/j.1525....
5.
Longo UG, Loppini M, Denaro L, et al. Rating scales for low back pain. Br Med Bull. 2010;94:81–144. https://doi.org/10.1093/bmb/ld....
6.
Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88 Suppl 2:21–24. http://dx.doi.org/10.2106/JBJS....
7.
Saragiotto BT, Machado GC, Ferreira ML, et al. Paracetamol for low back pain. Cochrane Database Syst Rev. 2016;2016(6):CD012230. Published 2016 Jun 7. https://doi.org/10.1002/146518....
8.
Machado GC, Maher CG, Ferreira PH, et al. Non-steroidal anti-inflammatory drugs for spinal pain: a systematic review and meta-analysis. Ann Rheum Dis. 2017;76(7):1269–1278. https://doi.org/10.1136/annrhe....
9.
Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514–530. https://doi.org/10.7326/M16-23....
10.
Vargatu I. Williams textbook of endocrinology. Acta Endocrinol (Buchar). 2016 Jan-Mar;12(1):113. https://doi.org/10.4183/aeb.20....
11.
First L, Douglas W, Habibi B, et al. Cannabis Use and Low-Back Pain: A Systematic Review. Cannabis Cannabinoid Res. 2020;15;5(4):283–289. https://doi.org/10.1089/can.20....
12.
Morgan MM, Christie MJ. Analysis of opioid efficacy, tolerance, addiction and dependence from cell culture to human. Br J Pharmacol. 2011;164(4):1322–1334. https://doi.org/10.1111/j.1476....
13.
Russo EB. History of cannabis and its preparations in saga, science, and sobriquet. Chem Biodivers. 2007;4(8):1614–1648. https://doi.org/10.1002/cbdv.2....
14.
Hill KP, Palastro MD, Johnson B, et al. Cannabis and Pain: A Clinical Review. Cannabis Cannabinoid Res. 2017;2(1):96–104. https://doi.org/10.1089/can.20....
15.
Bridgeman MB, Abazia DT. Medicinal Cannabis: History, Pharmacology, And Implications for the Acute Care Setting. PT. 2017;42(3):180–188. https://www.ncbi.nlm.nih.gov/p....
16.
Pagano C, Navarra G, Coppola L, et al. Cannabinoids: Therapeutic Use in Clinical Practice. Inter J Molec Sci. 2022;23(6):3344. https://doi.org/10.3390/ijms23....
18.
Tahir MN, Shahbazi F, Rondeau-Gagné S, et al. The biosynthesis of the cannabinoids. J Cannabis Res. 2021;3;7. https://doi.org/10.1186/s42238....
19.
Amin MR, Ali DW. Pharmacology of Medical Cannabis. Adv Exp Med Biol. 2019;1162:151–165. https://doi.org/10.1007/978-3-....
20.
Significant seizure reductions in patients with Dravet syndrome. https://www.epidiolexhcp.com/e... (access: 01.03.2023).
21.
Golub V, Reddy DS. Cannabidiol Therapy for Refractory Epilepsy and Seizure Disorders. Adv Exp Med Biol. 2021;1264:93–110. https://doi.org/10.1007/978-3-....
22.
Manera C, Bertini S. Cannabinoid-Based Medicines and Multiple Sclerosis. Adv Exp Med Biol. 2021;1264:111–129. https://doi.org/10.1007/978-3-....
23.
Keating GM. Delta-9-Tetrahydrocannabinol/Cannabidiol Oromucosal Spray (Sativex®): A Review in Multiple Sclerosis-Related Spasticity. Drugs. 2017;77(5):563–574. https://doi.org/10.1007/s40265....
24.
Corroon J, Phillips JA. A Cross-Sectional Study of Cannabidiol Users. Cannabis Cannabinoid Res. 2018;3(1):152–161. https://doi.org/10.1089/can.20....
25.
World Health Organization Expert Committee on Drug Dependence. Cannabidiol (CBD) Pre-Review Report Agenda Item 5.2 and Peer Review, 2017. https://www.drugsandalcohol.ie... (access: 01.03.2023).
26.
O’Brien K, Blair P. Medicinal Cannabis and CBD in Mental Healthcare; Switzerland: Springer Cham; 2021.
27.
O’Brien K. Cannabidiol (CBD) in Cancer Management. Cancers. 2022;14(4):885. https://doi.org/10.3390/cancer....
28.
Maroon J, Bost J. Review of the neurological benefits of phytocannabinoids. Surg Neurol Int. 2018;26(9):91. https://doi.org/10.4103/sni.sn....
29.
Machado Bergamaschi M, Helena Costa Queiroz R, Waldo Zuardi A, et al. Safety and Side Effects of Cannabidiol, a Cannabis sativa Constituent. Current Drug Safety 2011;6(4):237–249. https://doi.org/10.2174/157488....
30.
Wheeler M, Merten JW, Gordon BT, et al. CBD (Cannabidiol) Product Attitudes, Knowledge, and Use Among Young Adults. Subst Use Misuse. 2020;55(7):1138–1145. https://doi.org/10.1080/108260....
31.
Lovecchio F, Langhans MT, Bennett T, et al. Prevalence of Cannabidiol Use in Patients With Spine Complaints: Results of an Anonymous Survey. Int J Spine Surg. 2021;15(4):663–668. https://doi.org/10.14444/8087.
32.
Chesney E, Oliver D, Green A, et al. Adverse effects of cannabidiol: a systematic review and meta-analysis of randomized clinical trials.Neuro Psycho Pharmacol. 2020;45:1799–1806. https://doi.org/10.1038/s41386....
33.
Berger BA, Stolz U, Colvin J, et al. Epidemiology of cannabidiol related cases reported in the National Poison Data System – 2019–2020. Am J Emerg Med. 2021;48:218–223. https://doi.org/10.1016/j.ajem....
34.
National Library of Medicine. National Center for Biotechnology Information. https://pubchem.ncbi.nlm.nih.g... (access: 01.03.2023).
35.
Tahir MN, Shahbazi F, Rondeau-Gagné S, et al. The biosynthesis of the cannabinoids. J Cannabis Res. 2021;15;3(1):7. https://doi.org/10.1186/s42238....
36.
Appendino, G. The early history of cannabinoid research. Rend. Fis. Acc. Lincei 2020;31,919–929. https://doi.org/10.1007/s12210....
37.
World Health Organization (WHO). Cannabidiol (CBD) Critical Review Report; Expert Committee on Drug Dependence Fortieth Meeting Geneva, 4–7 June 2018; World Health Organization (WHO): Geneva, Switzerland, 2018; Available online: https://www.who.int/medicines/... (access: 20.07.2021).
38.
Hallak JE, Dursun SM, Bosi DC, et al. The interplay of cannabinoid and NMDA glutamate receptor systems in humans: preliminary evidence of interactive effects of cannabidiol and ketamine in healthy human subjects. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(1):198–202. https://doi.org/10.1016/j.pnpb....
39.
McGuire P, Robson P, Cubala WJ, et al. Cannabidiol (CBD) as an Adjunctive Therapy in Schizophrenia: A Multicenter Randomized Controlled Trial. Am J Psychiatry. 2018;175(3):225–231. https://doi.org/10.1176/appi.a....
40.
White CM. A Review of Human Studies Assessing Cannabidiol’s (CBD) Therapeutic Actions and Potential. J Clin Pharmacol. 2019;59(7):923–934. https://doi.org/10.1002/jcph.1....
41.
Zuardi AW, Crippa JA, Hallak JE, et al. Cannabidiol for the treatment of psychosis in Parkinson’s disease. J Psychopharmacol. 2009;23(8):979–983. https://doi.org/10.1177/026988....
42.
van de Donk T, Niesters M, Kowal MA, et al. An experimental randomized study on the analgesic effects of pharmaceutical-grade cannabis in chronic pain patients with fibromyalgia. Pain. 2019;160(4):860–869. https://doi.org/10.1097/j.pain....
43.
Ko GD, Bober SL, Mindra S, et al. Medical cannabis – the Canadian perspective. J Pain Res. 2016;9:735–744. https://doi.org/10.2147/JPR.S9....
44.
Costa B, Trovato AE, Comelli F, et al. The non-psychoactive cannabis constituent cannabidiol is an orally effective therapeutic agent in rat chronic inflammatory and neuropathic pain. Eur J Pharmacol. 2007;556(1–3):75–83. https://doi.org/10.1016/j.ejph....
45.
Zou S, Kumar U. Cannabinoid Receptors and the Endocannabinoid System: Signaling and Function in the Central Nervous System. Int J Mol Sci. 2018;13:19(3):833. https://doi.org/10.3390/ijms19....
46.
Woodhams SG, Sagar DR, Burston JJ, et al. The role of the endocannabinoid system in pain. Handb Exp Pharmacol. 2015;227:119–143. https://doi.org/10.1007/978-3-....
47.
Finn DP, Haroutounian S, Hohmann AG, et al. Cannabinoids, the endocannabinoid system, and pain: a review of preclinical studies. Pain. 2021;1(162) Suppl 1:S5–S25. https://doi.org/10.1097/j.pain....
48.
Mackie K. Cannabinoid Receptors: Where They are and What They do. J Neuroendocrinol. 2008;20:10–14. https://doi.org/10.1111/j.1365....
49.
Hill MN, Sun JC, Tse MT, et al. Altered responsiveness of serotonin receptor subtypes following long-term cannabinoid treatment. Int J Neuropsychopharmacol. 2006;9(3):277–286. https://doi.org/10.1017/S14611....
50.
Kathmann M, Flau K, Redmer A, et al. Cannabidiol is an allosteric modulator at mu- and delta-opioid receptors. Naunyn Schmiedebergs Arch Pharmacol. 2006;372(5):354–361. https://doi.org/10.1007/s00210....
51.
Mlost J, Bryk M, Starowicz K. Cannabidiol for Pain Treatment: Focus on Pharmacology and Mechanism of Action. Int J Mol Sci. 2020;21(22):8870. https://doi.org/10.3390/ijms21....
52.
De Gregorio D, McLaughlin RJ, Posa L, et al. Cannabidiol modulates serotonergic transmission and reverses both allodynia and anxiety-like behavior in a model of neuropathic pain. Pain. 2019;160(1):136–150. https://doi.org/10.1097/j.pain....
53.
Hayes C, Martin JH. Lack of efficacy of cannabidiol for relieving back pain: time to re-set expectations? MJA. 2021;214(8),360–361. https://doi.org/10.5694/mja2.5....
54.
Bebee B, Taylor DM, Bourke E, et al. The CANBACK trial: a randomised, controlled clinical trial of oral cannabidiol for people presenting to the emergency department with acute low back pain. Med J Aust. 2021;214(8):370–375. https://doi.org/10.5694/mja2.5....
55.
Eskander JP, Spall J, Spall A, et al. Cannabidiol (CBD) as a treatment of acute and chronic back pain: A case series and literature review. J Opioid Manag. 2020;16(3):215–218. https://doi.org/10.5055/jom.20....
56.
Meng H, Deshpande A. Cannabinoids in chronic non-cancer pain medicine: moving from the bench to the bedside. BJA Educ. 2020;20(9):305–311. https://doi.org/10.1016/j.bjae....
57.
Abdallah FW, Hussain N, Weaver T, et al. Analgesic efficacy of cannabinoids for acute pain management after surgery: a systematic review and meta-analysis. Reg Anesth Pain Med. 2020;45(7):509–519. https://doi.org/10.1136/rapm-2....
58.
Shah RM, Saklecha A, Patel AA, et al. Analyzing the Impact of Cannabinoids on the Treatment of Spinal Disorders. Curr Rev Musculoskelet Med. 2022;15(2):133–142. https://doi.org/10.1007/s12178....
59.
Yassin M, Oron A, Robinson D. Effect of adding medical cannabis to analgesic treatment in patients with low back pain related to fibromyalgia: an observational cross-over single centre study. Clin Exp Rheumatol. 2019;37(Suppl 116(1)):13–20.
60.
Yassin M, Garti A, Robinson D. Effect of medicinal cannabis therapy (MCT) on severity of chronic low back pain, sciatica and lumbar range of motion. Int J Anesthesiol Pain Med. 2016;2(1):5. https://doi.org/10.21767/2471-....
61.
Takakuwa KM, Hergenrather JY, Shofer FS, et al. The Impact of Medical Cannabis on Intermittent and Chronic Opioid Users with Back Pain: How Cannabis Diminished Prescription Opioid Usage. Cannabis Cannabinoid Res. 2020;5(3):263–270. https://doi.org/10.1089/can.20....
62.
Ueberall MA, Vila Silván C, Essner U, et al. Effectiveness, Safety, and Tolerability of Nabiximols Oromucosal Spray vs Typical Oral Long-Acting Opioid Analgesics in Patients with Severe Neuropathic Back Pain: Analysis of 6-Month Real-World Data from the German Pain e-Registry. Pain Med. 2022;23(4):745–760. https://doi.org/10.1093/pm/pna....
63.
Hoggart B, Ratcliffe S, Ehler E, et al. A multicentre, open-label, follow-on study to assess the long-term maintenance of effect, tolerance and safety of THC/CBD oromucosal spray in the management of neuropathic pain. J Neurol. 2015;262(1):27–40. https://doi.org/10.1007/s00415....
64.
Lovecchio F, Langhans MT, Bennett T, et al. Prevalence of Cannabidiol Use in Patients With Spine Complaints: Results of an Anonymous Survey. Int J Spine Surg. 2021;15(4):663–66.
65.
Harvey AM. Classification of chronic pain – descriptions of chronic pain syndromes and definitions of pain terms. Clin J Pain. 1995;11(2):163. https://doi.org/10.1097/000025....
66.
Thomson S. Failed back surgery syndrome – definition, epidemiology and demographics. Br J Pain. 2013;7(1):56–59. https://doi.org/10.1177/204946....
67.
Mondello E, Quattrone D, Cardia L, et al. Cannabinoids and spinal cord stimulation for the treatment of failed back surgery syndrome refractory pain. J Pain Res. 2018;11:1761–1767. https://doi.org/10.2147/JPR.S1....
68.
Fitzcharles MA, Baerwald C, Ablin J, et al. Efficacy, tolerability and safety of cannabinoids in chronic pain associated with rheumatic diseases (fibromyalgia syndrome, back pain, osteoarthritis, rheumatoid arthritis): A systematic review of randomized controlled trials. Schmerz. 2016;30(1):47–61. https://doi.org/10.1007/s00482....
69.
Senderovich H, Wagman H, Zhang D, et al. The Effectiveness of Cannabis and Cannabis Derivatives in Treating Lower Back Pain in the Aged Population: A Systematic Review. Gerontol. 2022;68:612–624. https://doi.org/10.1159/000518....
70.
Xantus G, Zavori L, Matheson C, et al. Cannabidiol in low back pain: scientific rationale for clinical trials in low back pain. Exp Rev Clinical Pharmacol. 2021;14(6):671–675. https://doi.org/10.1080/175124....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.