Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
An analysis of anxiety and selected aspects of personality in women with ischemic heart disease according to P.T. Costa and R. R. McCrae theory – The role of psychosocial factors in ischemic heart disease
1
Department of Clinical Psychology, Medical University, Lublin, Poland
2
Department of Cardiology, Medical University, Lublin, Poland
3
Department of Anaesthesiology and Intensive Therapy, Medical University, Lublin, Poland
Corresponding author
Tomasz Zapolski
Katedra i Klinika Kardiologii; Uniwersytet Medyczny, ul. Jaczewskiego 8, 20-954, Lublin, Poland
Katedra i Klinika Kardiologii; Uniwersytet Medyczny, ul. Jaczewskiego 8, 20-954, Lublin, Poland
Ann Agric Environ Med. 2021;28(1):107-113
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Risk factors for ischemic heart disease (IHD) are very numerous and not fully defined. In addition to classic risk factors, different factors are also distinguished, among them psychological aspects chich have rarely been subject to detailed analyses.
Objective:
The aim of study was an analysis of the anxiety structure, including the five factors of personality: neuroticism (NEU), extraversion (EXT), openness (OPE), agreeableness (AGR) and conscientiousness (CON), in women with IHD.
Material and methods:
The study involved 140 women aged 37–74 years with IHD confirmed by coronary angiography. Psychological examination was conducted using R.B. Cattell’s IPAT Anxiety Scale and P.T. Costa and R.R. McCrae’s NEO-FFI Personality Inventory.
Results:
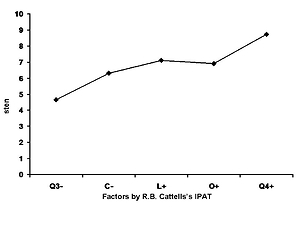
The results obtained from the IPAT Anxiety Scale showed that the study group of 140 women with IHD had the correct level of internal integrity (Q3– ). The dominant factor in the anxiety structure in 88.7% of subjects was neurotic tension (Q4+). A lack of sense of safety was indicated by 72.6% of subjects (L+), 69.3% experienced a strong tendency to self-blame and experience a sense of guilt (O + ), and over 51.6% of women with IHD expressed decreased emotional stability (C – ). The level of general anxiety was high (GA=7.3). The analysis of the five factors of personality revealed that the dominant factors in the structure of personality of women with IHD were CON in 69.3%, AGR in 46.7% and EXT in 45.2%. NEU and OPE were moderately significant factors.
Conclusions:
Women with IHD are characterised by a high level of anxiety, increased neurotic tension, decreased emotional stability, auto-aggression and a sense of danger and distrust. Women with IHD demonstrate a high level of factors, such as extraversion, agreeableness and conscientiousness.
Risk factors for ischemic heart disease (IHD) are very numerous and not fully defined. In addition to classic risk factors, different factors are also distinguished, among them psychological aspects chich have rarely been subject to detailed analyses.
Objective:
The aim of study was an analysis of the anxiety structure, including the five factors of personality: neuroticism (NEU), extraversion (EXT), openness (OPE), agreeableness (AGR) and conscientiousness (CON), in women with IHD.
Material and methods:
The study involved 140 women aged 37–74 years with IHD confirmed by coronary angiography. Psychological examination was conducted using R.B. Cattell’s IPAT Anxiety Scale and P.T. Costa and R.R. McCrae’s NEO-FFI Personality Inventory.
Results:
The results obtained from the IPAT Anxiety Scale showed that the study group of 140 women with IHD had the correct level of internal integrity (Q3– ). The dominant factor in the anxiety structure in 88.7% of subjects was neurotic tension (Q4+). A lack of sense of safety was indicated by 72.6% of subjects (L+), 69.3% experienced a strong tendency to self-blame and experience a sense of guilt (O + ), and over 51.6% of women with IHD expressed decreased emotional stability (C – ). The level of general anxiety was high (GA=7.3). The analysis of the five factors of personality revealed that the dominant factors in the structure of personality of women with IHD were CON in 69.3%, AGR in 46.7% and EXT in 45.2%. NEU and OPE were moderately significant factors.
Conclusions:
Women with IHD are characterised by a high level of anxiety, increased neurotic tension, decreased emotional stability, auto-aggression and a sense of danger and distrust. Women with IHD demonstrate a high level of factors, such as extraversion, agreeableness and conscientiousness.
ACKNOWLEDGEMENTS
The study was supported by the Grant No. DS 377 from the Medical University in Lublin, Poland
REFERENCES (46)
1.
Lubiszewska B, Skóra E, Kruk M, Broda G, Księżycka E, Kurjata P, et al. Prevalence of classical risk factors in Polish women with premature coronary artery disease. Kardiol Pol. 2010; 68: 1032–7.
2.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart Disease and Stroke Statistics—2018 Update A Report From the American Heart Association. Circulation. 2018; 137: e67–e492.
3.
Kershaw KN, Brenes GA, Charles LE, Coday M, Daviglus ML, Denburg NL, Kroenke CH, Safford MM, Savla T, Tindle HA, Tinker LF, Van Horn L. Associations of stressful life events and social strain with incident cardiovascular disease in the Women’s Health Initiative. J Am Heart Assoc. 2014; 3: e000687.
4.
Felix AS, Lehman A, Nolan TS, Sealy-Jefferson S, Breathett K, Hood DB, Addison D, Anderson CM, Cené CW, Warren BJ, Jackson RD, Williams KP. Stress, resilience, and cardiovascular disease risk among black women. Circulation: Cardiovascular Quality and Outcomes. 2019;12: e005284.
5.
Colpani V, Baena CP, Jaspers L, van Dijk GM, Farajzadegan Z, Dhana K, Tielemans MJ, Voortman T, Freak-Poli R, Veloso GGV, Chowdhury R, Kavousi M, Muka T, Franco OH. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis. Eur J Epidemiol. 2018; 33(9): 831–845.
6.
Domíngu F, Fuster V, Fernández-Alvira, JM, Fernández-Friera L, López-Melgar B, Blanco-Rojo R, Fernández-Ortiz A, García-Pavía P, Sanz J, Mendiguren J, Ibañez B, Bueno H, Lara-Pezzi E, Ordovás JM. Association of sleep duration and quality with subclinical atherosclerosis. J Am Coll Cardiol. 2019; 73(2): 134–144.
7.
Nasiłowska-Barud A, Zapolski T, Barud M, Wysokiński A. Overt and covert anxiety as a toxic factor in ischemic heart disease in women: The link between psychological factors and heart disease. Med Sci Monit. 2017; 23: 751–8.
8.
Mehta P K, Wei J, Wenger N K. Ischemic heart disease in women: A Focus on risk factors. Trends Cardiovasc Med. 2015; 25(2): 140–5.
9.
Pietras T, Witusik A, Panek M, Szemraj J, Górski P. Anxiety, depression and methods of stress coping in patients with nicotine dependence syndrome. Med Sci Monit. 2011; 17: CR272–6.
10.
Mikaliūkštienė A, Žagminas K, Juozulynas A, Narkauskaitė L, Sąlyga J, Jankauskienė K, et al. Prevalence and determinants of anxiety and depression symptoms in patients with type 2 diabetes in Lithuania. Med Sci Monit. 2014; 20: 182–90.
11.
Shi H, Feng G, Wang Z, Zhou C, Zhong G, Hu Y, et al. Relationships between Depressive Symptoms and Endothelial Function Among Out-patients of a General Hospital in China. Med Sci Monit. 2015; 21: 1812–9.
12.
Vaccarino V, Bremner JD. Behavioral, emotional and neurobiological determinants of coronary heart disease risk in women. Neurosci Biobehav Rev. 2017; 74: 297–309.
13.
Carney RM, Freedland KE. Depression and coronary heart disease. Nat Rev Cardiol. 2017; 14: 145–155.
14.
Fauerbach JA, Bush DE, Thombs BD, McCann UD, Fogel J, Ziegelstein RC. Depression following acute myocardial infarction: a prospective relationship with ongoing health and function. Psychosomatics. 2005; 46: 355–1.
15.
Lichtman IH, Froelicher ES, Blumenthal IA, Carney RM, Doering LV, Frasure-Smith N, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: systematic review and recommendations: a scientific statement from the American Heart Association. Circulation. 2014; 129: 1350–1369.
16.
Celano Ch, Daunis D, Lakko H, Campbell K, Huffman J. Anxiety disorders and cardiovascular disease. Curr Psychiatry Rep. 2016; 18(11): 101–110.
17.
Khayyam-Nekonei Z, Neshatdoost H, Yousefy A, Sadeghi M, Manshaee S. Psychologiacal factors and coronary heart disease. Atherosclerosis. 2013; 9: 102–111.
18.
Sadowski M, Gąsior M, Gierlotka M, Janion M, Poloński L. Clinical characteristics of Polish women with ST-segment elevation acute myocardial infarction. Kardiol Pol. 2010; 68: 627–4.
19.
Mack M, Gopal A. Epidemiology, traditional and novel risk factors in coronary artery disease. Heart Failure Clinics. 2016; 12(1): 1–10.
20.
McCrae RR, Costa PT Jr. Validation of the five–factor model of personality across instruments and observers. J Pers Soc Psych. 1987; 52: 81–90.
21.
Hornowska E. Testy psychologiczne: teoria i praktyka. Warszawa. Scholar; 2007: 136.
22.
Nasiłowska-Barud A, Żuk M, Jabłońska-Brzozowska J, Wysokiński A, Brzozowski W. Psychological problems in patients with atrial fibrillation. Post Nauk Med. 2015; 8: 540–544.
23.
Nasiłowska-Barud A, Kowalik M. Characteristics of depressive changes and anxiety in patients with essential hypertension. An UMCS Sec D. 2004; 59(1): 428–433.
24.
Young Bok L, Jihan MD Y, Hyun Ho C, Bu Seok J, Hyung-Keun K, Sang-Woo K, Sung Soo K, Yong Gyu P, Hiun Suk C. The association between peptic ulcer diseases and mental health problems. A population-based study a STROBE compliant article. Meidcine. 2017; 96(34): e7728.
25.
Robinson D, Coons M, Haensel H, Valais M, Yale J-F. Diabetes Canada 2018 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2018; 42 (Suppl 1): S130-S141.
26.
Unseld M, Krammer K, Lubowitzki S, Jachs M, Baumann L, Vyssoki B, Riedel J, Puhr H, Zehentgruber S, Prager G, Masel EK, Preusser M, Jaeger U, Gaiger A. Screening for post-traumatic stress disorders in 1017 cancer patients and correlation with anxiety, depression, and distress. Psycho-Oncology. 2019; 28: 2382–2388.
27.
Prado-Olivares J, Chover-Sierra E. Preoperatory anxiety in patients undergoing cardiac surgery. Diseases. 2019; 7(2): 46.
28.
Vaccarino V, Badimon L, Bremner JD, Cenko E, Cubedo J, Dorobantu M. Depression and coronary heart disease: 2018 position paper of the ESC working group on coronary pathophysiology and microcirculation. Eur Heart J. 2019; 0: 1–15.
29.
Kozela M, Bobak M, Beala AM, Micek A, Kubinova R, Malyutina S, et al. The association of depressive symptoms with cardiovascular and all-cause mortality in Central and Extern Europe: Prospective results of the HAPIEE study. Eur J Prev Kardiol. 2016; 23: 1839–1847.
30.
Ansari I, Fallahi F, Ghanem A, Babakhani E, Hashemi Z, Mohammadian E, et al. The relation between depression and ischemic heart disease among middle aged people: a case control study. J Basic Clin Pathophysiol. 2019; 7: 15–20.
31.
Cohen BE, Panguluri P, Na B, Whooley MA. Psychological risk factors and the metabolic syndrome in patients with coronary heart disease: findings from the Heart and Soul Study. Psychiatry Res. 2010; 175: 133–7.
32.
Baune BT, Neuhauser H, Ellert U, Berger K. The role of the inflammatory markers ferritin, transferring and fibrinogen in the relationship between major depression and cardiovascular disorders: the German Healt Interview and Examination Survey. Acta Psychiatr Scand. 2010; 121: 135–2.
33.
Chuvet-Gelinier J-C, Bonin B. Stress, anxiety and depression in heart disease patients: A major challenge for cardiac rehabilitation. Ann Physic Rehabil Med. 2017; 60: 6–12.
34.
Moser DK, Dracup K, McKinley S, Yamasaki K, Kim CJ, Riegel B. An international perspective on gender differences in anxiety early after acute myocardial infarction. Psychosom Med. 2003; 65: 511–6.
35.
Eaker ED, Pinsky J, Castelli WP. Myocardial infarction and coronary death among women: psychosocial predictors from a 20-year follow-up of women in the Framingham Study. Am J Epidemiol. 1992; 135: 854–4.
36.
Stone SV, Costa PT. Disease-prone personality or distress-prone personality? The role of neuroticism in coronary heart disease. In: Friedman HS (Ed.). Personality and disease. New York: Wiley, 1990; 178–9.
37.
Eichstaedt JC, Schwartz HA, Kern MI, Park G, Labarthe DR, Merchant RM, et al. Psychological language on Twitter predicts county-level heart rate mortality. Psychol Sci. 2015; 26: 159–9.
38.
Alams A, Moller J, Iqbal R, Forsell Y. Effect of neuroticism on risk cardiovascular disease in depressed persons – a Swedish population – based cohort study. BMC Cardiovasc Disord. 2017; 17: 185.
39.
Costa PT, Zonderman AB, Engel BT, Baile WF, Brimlow DL, Brinker J. The relation of chest pain symptoms to angiographic findings of coronary artery stenosis and neuroticism. Psychosom Med. 1985; 47: 285–3.
40.
Costa PT Jr. Influence of the normal personality dimension of neuroticism on chest pain symptoms and coronary artery disease. Am J Cardiol. 1987; 60: 20J–6J.
41.
Goldberg LR. An alternative “descriprion of personality”: the big-five factor structure. J Pers Soc Psychol. 1990; 59: 1216–9.
42.
Luchetti M, Barkley JM, Stephan Y, Terracciano A, Sutin AR. Five-factor model personality traits and inflammatory markers: new data and meta-analysis. Psychoneuroendocrinology. 2014; 50: 181–3.
43.
Mõtus R, Luciano M, Starr JM, Pollard MC, Deary IJ. Personality traits and inflammation in men and women in their early 70s: the Lothian Birth Cohort 1936 study of healthy aging. Psychosom Med. 2013; 75: 11–9.
44.
Garcia M, Mulvagh SL, Bairey Merz CN, Bering JE, Manson JE. Cardiovascular disease in women: Clinical perspectives. Circ Res. 2016; 118(8): 1273–1293.
45.
Pierce GL, Kalil1 GZ, Ajibewa1 T, Holwerda SW, Persons J, Moser DJ, Fiedorowicz JG. Anxiety independently contributes to elevated inflammation in humans with obesity. Obesity. 2017; 25: 286–289.
46.
Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, Kessler RC. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006; 63(7): 824–830.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.