Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Children’s well-being and expectations before planned surgery
1
Department of Paediatrics and Paediatric Nursing, Medical University, Lublin, Poland
These authors had equal contribution to this work
Corresponding author
Alina Trojanowska
Department of Peadiatrics and Peadiatric Nursing, Medical University of Lublin, Chodźki 7, 20-093, Lublin, Poland
Department of Peadiatrics and Peadiatric Nursing, Medical University of Lublin, Chodźki 7, 20-093, Lublin, Poland
Ann Agric Environ Med. 2025;32(3):391-397
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The need for surgical treatment causes a psychological burden in children and is a source of fear and anxiety, which may hinder the procedure and recovery. The aim of the study is to assess the well-being of children before surgery, paying attention to anxiety and anger, and to learn about their fears and expectations.
Material and methods:
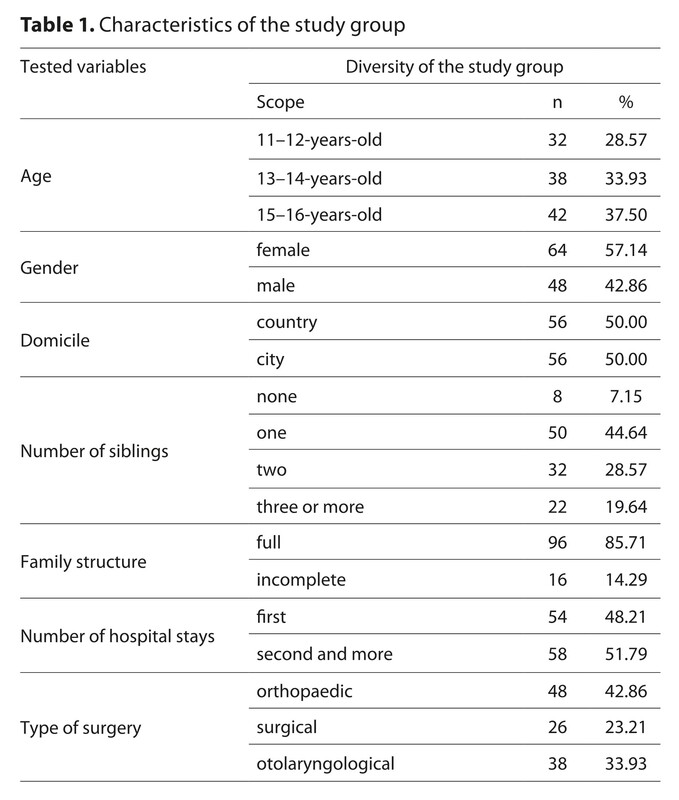
The research was conducted among 112 children aged 11–16 (average age 13.5±2.6) waiting for surgery in 3 departments (surgery, laryngology and orthopaedics) of USD in Lublin. The research used the Overt Anxiety Scale (SJN) ‘What Are You Like?’, the Anger Expression Scale (SEG), and a self-designed questionnaire.
Results:
Most children waiting for surgery had a reduced sense of security (90.0%) and felt anxiety (55.4%), anger and nervousness (50.0%), mainly due to the lack of information. Nearly all children (92.9%) experienced pre-operative anxiety. The majority of participants characterized their anxiety as mild (44.6%), while the remaining respondents classified it as moderate (28.6%) or severe (19.7%). The factor that additionally reduced well-being was the parents’ anxiety, and the sight of other sick children after the procedure. The presence of parents and the kindness and understanding of the staff had a positive impact on the emotional state of the respondents. The children were afraid of pain and limited activity. They expected information about limitations before and after the procedure, pain management and quick recovery.
Conclusions:
Children and adolescents in the pre-operative period require psychotherapeutic interventions and information support from medical staff, which may contribute to reducing their anxiety and have a positive impact on their recovery.
The need for surgical treatment causes a psychological burden in children and is a source of fear and anxiety, which may hinder the procedure and recovery. The aim of the study is to assess the well-being of children before surgery, paying attention to anxiety and anger, and to learn about their fears and expectations.
Material and methods:
The research was conducted among 112 children aged 11–16 (average age 13.5±2.6) waiting for surgery in 3 departments (surgery, laryngology and orthopaedics) of USD in Lublin. The research used the Overt Anxiety Scale (SJN) ‘What Are You Like?’, the Anger Expression Scale (SEG), and a self-designed questionnaire.
Results:
Most children waiting for surgery had a reduced sense of security (90.0%) and felt anxiety (55.4%), anger and nervousness (50.0%), mainly due to the lack of information. Nearly all children (92.9%) experienced pre-operative anxiety. The majority of participants characterized their anxiety as mild (44.6%), while the remaining respondents classified it as moderate (28.6%) or severe (19.7%). The factor that additionally reduced well-being was the parents’ anxiety, and the sight of other sick children after the procedure. The presence of parents and the kindness and understanding of the staff had a positive impact on the emotional state of the respondents. The children were afraid of pain and limited activity. They expected information about limitations before and after the procedure, pain management and quick recovery.
Conclusions:
Children and adolescents in the pre-operative period require psychotherapeutic interventions and information support from medical staff, which may contribute to reducing their anxiety and have a positive impact on their recovery.
ACKNOWLEDGEMENTS
The authors wish to thank the children and their parents, the
hospital management, and Agata Stępniewska-Król, MA, for
their participation in the study.
FUNDING
The study was funded by the Polish Ministry of
Education and Science under the project:
‘Doskonała Nauka II. Wsparcie bezpieczeństwa pacjenta
przez popularyzację dowodów naukowych w praktyce
zawodów medycznych.’ (Projekt No. KONF/SP/265/2023/01).
‘Excellent Science II. Supporting patient safety by
popularizing scientific evidence in the practice of medical
professions’. (Project No. KONF/SP/265/2023/01).
REFERENCES (29)
1.
Perrott C, Lee CA, Griffiths S, et al. Perioperative experiences of anesthesia reported by children and parents. Paediatr Anaesth. 2018;28(2):149–156. doi:10.1111/pan.13300.
2.
Suleiman-Martos N, Garcia-Lara RA, Membrive-Jimenez MJ, et al. Effect of a game-based intervention on preoperative pain and anxiety in children: A systematic review and meta-analysis. J Clin Nurs. 2022;31(23–24):3350–3367. doi:10.1111/jocn.16227.
3.
Beyliklioğlu A, Arslan S. Effect of Lavender Oil on the Anxiety of Patients Before Breast Surgery. J Perianesth Nurs. 2019;34(3):587–593. doi:10.1016/j.jopan.2018.10.002.
4.
Dudziak A, Sitarczyk M. Ekspresja gniewu a problematyczne używanie Internetu. Polskie Forum Psychologiczne. 2022(4):452–463. https://doi.org/10.34767/PFP.2....
5.
Szymaniak K. „Nie taki diabeł straszny…” – czyli poznawcze konsekwencje gniewu i ich motywacyjne podłoże. In: Zajenkowski M. Inteligencja w codziennym życiu. Warszawa: Wydawnictwo Liberi Libri; 2012:159–184.
6.
Adachi T, Yamada K, Fujino H, et al. Associations between anger and chronic primary pain: a systematic review and meta-analysis. Scand J Pain. 2021;15,22(1):1–13. doi:10.1515/sjpain-2021-0154.
7.
Fu SW, Li S, Shi ZY, et al. Interrater agreement between children’s self-reported and their mothers’ proxy-reported dental anxiety: a Chinese cross-sectional study. BMC Oral Health. 2023;10,23(1):139. doi:10.1186/s12903-023-02834-1.
8.
Breitkopf L. Emotionale Reaktionen von Kindern auf den Krankenhaus-aufenthalt Emotional reactions of children to hospitalization. Z Kinderchir. 1990;45(1):3–8. German. doi:10.1055/s-2008-1042540.
9.
Shah SB, Sinha R, Hussein SY, et al. Allaying Pediatric Preoperative Anxiety, Where are we Now? – A Nationwide Survey. J Indian Assoc Pediatr Surg. 2023;2(6):479–485. doi:10.4103/jiaps.jiaps_114_23.
10.
Zhong Y, Gong H, Long F, et al. A bibliometric analysis of research on pediatric preoperative anxiety (2007–2022). Front Pediatr. 2024;(12):1327118. doi:10.3389/fped.2024.1327118.
11.
Mustafa MS, Shafique MA, Zaidi SD, et al. Preoperative anxiety management in pediatric patients: a systemic review and meta-analysis of randomized controlled trials on the efficacy of distraction techniques. Front Pediatr. 2024;(12):1353508. doi:10.3389/fped.2024.1353508.
12.
Zwierzyńska E, Matuszewski A. Skala Jawnego Niepokoju ,,Jaki jesteś?’’ Elżbiety Skrzypek, Mieczysława Choynowskiego: podręcznik. Warszawa: Centrum Metodyczne Pomocy Psychologiczno-Pedagogicznej; 2007.
13.
Piekarski R, Szewczyk L, Bury A. Stan wyrównania metabolicznego i poziom niepokoju u nastolatków podczas pobytu na kolonii cukrzycowej. Endokrynol Ped. 2015;14.4.(53):25–28. doi:10.18544/EP-01.14.04.1627.
14.
Juczyński Z. Narzędzia pomiaru w promocji i psychologii zdrowia. Warszawa: Pracownia Testów Psychologicznych; 2012.
15.
Santapuram P, Stone AL, Walden RL, et al. Interventions for Parental Anxiety in Preparation for Pediatric Surgery: A Narrative Review. Children. 2021;8(11):1069. https://doi.org/10.3390/childr....
16.
Liu W, Xu R, Jia J, et al. Research Progress on Risk Factors of Preoperative Anxiety in Children: A Scoping Review. Int J Environ Res Public Health. 2022;9;19(16):9828. doi:10.3390/ijerph19169828.
17.
Getahun AB, Endalew NS, Mersha AT, et al. Magnitude and Factors Associated with Preoperative Anxiety among Pediatric Patients: Cross-Sectional Study. Pediatric Health Med Ther. 2020;11:485–494. doi:10.2147/PHMT.S288077.
18.
Shih MC, Elvis PR, Nguyen SA, et al. Parental Presence at Induction of Anesthesia to Reduce Anxiety: A Systematic Research and Meta-Analysis. J Perianesth Nurs. 2023;38(1):12–20. doi:10.1016/j.jopan.2022.03.008.
19.
Ghollami S, Mojen LK, Rassouli M, et al. Relationship Between Psychological Variables and Postoperative Pain in Children. J Compr Ped. 2024;15(1):127190. https://doi.org/10.5812/jcp-12....
20.
Dreuning KM, Haverman L, Bosschieter PF, et al. Age-specific and family-centered information modalities to prepare children at home for day-care surgery. J Pediatr Surg. 2023;58(3):510–517. doi:10.1016/j.jpedsurg.2022.08.023.
21.
Nytun KL, Moldestad IO, Snibsøer AK, et al. The effect of web-based preoperative information on parents of children who are going through elective ambulatory surgery: A systematic review and meta-analysis. Patient Educ Couns. 2022;105(12):3389–3397. doi:10.1016/j.pec.2022.09.006.
22.
Wu J, Yan J, Zhan L, et al. The effectiveness of distraction as preoperative anxiety management technique in pediatric patients: A systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud. 2022;130:104232. doi:10.1016/j.ijnurstu.2022.104232. Erratum in: Int J Nurs Stud. 2022;133:104285. doi:10.1016/j.ijnurstu.2022.104285.
23.
Taylan S, Kılıç KM, Özkan İ. Effects of virtual reality on pain, anxiety, and delirium in pediatric surgery: a systematic review and meta-analysis. Pediatr Surg Int. 2025;10;41(1):163. doi:10.1007/s00383-025-06084-w.
24.
Arthur T, Melendez-Torres GJ, Harris D, et al. Extended Reality Interventions for Health and Procedural Anxiety: Panoramic Meta-Analysis Based on Overviews of Reviews. J Med Internet Res. 2025;8;27:e58086. doi:10.2196/58086.
25.
Suleman SK, Yahya N, Nilsson S, et al. Comparative efficacy of pharmacological and non-pharmacological interventions for mitigating pain and anxiety associated with venipuncture: a randomised controlled trial. BMJ Paediatr Open. 2024;9;8(1):e002881. doi:10.1136/bmjpo-2024-002881.
26.
Rosenbloom BN, Frederiksen SD, Wang V, et al. Prognostic factors of chronic postsurgical pain in children and adolescents: a systematic review and meta-analysis. Reg Anesth Pain Med. 2025;5;50(2):144–152. doi:10.1136/rapm-2024-105696.
27.
Tomaszewski R, Janowska M. Psychological aspects of scoliosis surgery in children. Stud Health Technol Inform. 2012;176:428–32.
28.
Bartik K, Toruner EK. Effectiveness of a Preoperative Preparation Program on Children’s Emotional States and Parental Anxiety. J Perianesth Nurs. 2018;33(6):972–980. doi:10.1016/j.jopan.2017.09.008.
29.
Neumann AA, Desmarais EE, Iverson SL, et al. Ecological contributions to maternal-infant functioning: Differences between rural and urban family contexts. J Comm Psychol. 2020;(4)8,3:945–959. https://doi.org/10.1002/jcop.2....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.