Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
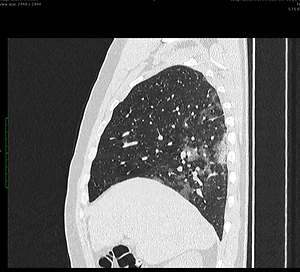
Diagnostic value of chest CT scanning for determination of Covid-19 severity in individual lung lobes
1
Medical University, Lublin, Poland
2
Department of Radiology VOXEL, Łańcut, Poland
3
University Hospital No 1, Lublin, Polan
Ann Agric Environ Med. 2022;29(1):115-119
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
CT examination is an important diagnostic tool in assessment of the severity of the infection and course of the disease. The aim of the study was to evaluate the degree and frequency of involvement of individual lung lobes and the population Lobe Involvement Coefficient (pLIC) value in the investigated population.
Material and methods:
The analyzed material comprised 124 patients aged 18–92 years. CT examinations were performed using a 16- and 32-row CT LightSpeed apparatus. The spatial distribution of typical Covid -19 pathological changes was analyzed, divided into five lung lobes. The degree of the severity of lobe involvement was assessed using counters and percentages, as well as the population Lobe Involvement Coefficient (pLIC). Statistical analysis of data was performed with the use of Statistica 10.0 software. Values were measured on an oridinal scale. Anova Friedman’s test was used to compare lobes.
Results:
Statistically significant differences in the involvement between most of the individual lobes were shown. There was no statistically significant difference in the degree of lobe involvement between the left and right upper lobes, nor in the left and right lower lobes. The highest pILC was demonstrated for the lower lobe and the lowest value was obtained for the middle lobe.
Conclusions:
The lower lobes were affected most frequently and most severely, with no statistical difference between the right and left sides. The middle lobe was affected relatively least frequently and lightly. The introduced pLIC index allows quantitative assessment of individual lobes involvement in relation to the entire studied population.
CT examination is an important diagnostic tool in assessment of the severity of the infection and course of the disease. The aim of the study was to evaluate the degree and frequency of involvement of individual lung lobes and the population Lobe Involvement Coefficient (pLIC) value in the investigated population.
Material and methods:
The analyzed material comprised 124 patients aged 18–92 years. CT examinations were performed using a 16- and 32-row CT LightSpeed apparatus. The spatial distribution of typical Covid -19 pathological changes was analyzed, divided into five lung lobes. The degree of the severity of lobe involvement was assessed using counters and percentages, as well as the population Lobe Involvement Coefficient (pLIC). Statistical analysis of data was performed with the use of Statistica 10.0 software. Values were measured on an oridinal scale. Anova Friedman’s test was used to compare lobes.
Results:
Statistically significant differences in the involvement between most of the individual lobes were shown. There was no statistically significant difference in the degree of lobe involvement between the left and right upper lobes, nor in the left and right lower lobes. The highest pILC was demonstrated for the lower lobe and the lowest value was obtained for the middle lobe.
Conclusions:
The lower lobes were affected most frequently and most severely, with no statistical difference between the right and left sides. The middle lobe was affected relatively least frequently and lightly. The introduced pLIC index allows quantitative assessment of individual lobes involvement in relation to the entire studied population.
REFERENCES (14)
1.
M-Y Ng, EYP Lee, Yang J, et al. Imaging Profile of the COVID-19 Infection: Radiologic Findings and Literature Review. Radiology Cardiothoracic Imaging. 2020; (2): e200034.
2.
Bernheim A, Mei X, Huang M, et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology. 2020; (295): 200463.
3.
Chung M, Bernheim A, Mei X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology. 2020; (295): 202–207.
4.
Wong HYF, Lam HYS, Fong AH-T, et al. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology 2020; (296): E72-E78.
5.
Haseli S, Khalili N, Bakhshayeshkaram M, Sanei Taheri M, Moharramzad Y. Lobar Distribution of COVID-19 Pneumonia Based on Chest Computed Tomography Findings; A Retrospective Study. Arch Acad Emerg Med. 2020; 8.
6.
Zu ZY, Jiang MD, Xu PP, et al. Coronavirus Disease 2019 (COVID-19): A Perspective from China. Radiology. 2020; (296): E15-E25.
7.
Asgharian B, Price O, Oberdörster G. A Modeling Study of the Effect of Gravity on Airflow Distribution and Particle Deposition in the Lung. Inhalation Toxicology. 2006; (18): 473–481.
8.
Warren MA, Zhao Z, Koyama T, et al. Severity scoring of lung oedema on the chest radiograph is associated with clinical outcomes in ARDS. Thorax. 2018; (73): 840–846.
9.
Smoleń A. Biostatystyka w badaniach medycznych i praktyce klinicznej. Polskie Archiwum Medecyny Wewnętrznej. 2016; (1): 3–20.
10.
Ai T, Yang Z, Hou H, et al. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020; (296): E32-E40.
11.
Pan F, Ye T, Sun P, et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020; (295): 715–721.
12.
Bettinelli D, Kays C, Bailliart O, et al. Effect of gravity on chest wall mechanics. J Appl Physiol. 2002; (92): 709–716.
13.
Yang R, Li X, Liu H, et al. Chest CT Severity Score: An Imaging Tool for Assessing Severe COVID-19. Radiology Cardiothoracic Imaging. 2020; (2): e200047.
14.
Bao C, Liu X, Zhang H, Li Y, Liu J. Coronavirus Disease 2019 (COVID-19) CT Findings: A Systematic Review and Meta-analysis. J Am College Radiol. 2020; (17): 701–709.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.