Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
CASE REPORT
Analysis of changes in electromyographic masticatory muscle activity in relation to the selected correction of refractive error
1
Department of Sports Medicine, Medical University, Lublin, Poland
2
Interdisciplinary Scientific Group of Sports Medicine, Department of Sports Medicine, Medical University, Lublin, Poland
3
Department of Rehabilitation and Physiotherapy, Medical University, Lublin, Poland
4
Students’ Scientific Association at the Department of General and Paediatric Ophthalmology, Medical University, Lublin,
Poland
5
Department of General and Pediatric Ophthalmology, Medical University, Lublin, Poland
6
Department of Functional Masticatory Disorders, Medical University, Lublin, Poland
Corresponding author
Ann Agric Environ Med. 2022;29(3):457-462
KEYWORDS
TOPICS
ABSTRACT
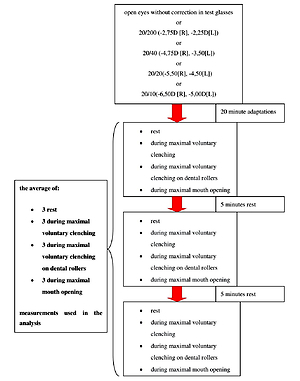
Wearing glasses is safe, effective, and the most popular method in correcting myopia. The study aimed to analyze the changes in electromyographic activity of the masticatory muscles about the selected correction of refractive error. Two muscle pairs were analyzed: the anterior part of the temporalis muszle and the superficial part of the masseter muscle. The patient was fitted with 20/200, 20/40 20/20, 20/10 corrections of refractive terror, and during each correction of refractive error, the changes in the recording of bioelectrical activity during rest, during maximal voluntary clenching, during maximal voluntary clenching on dental rollers were analyzed. With greater correction of refractive error, resting temporal muscle activity increases. Appropriate correction of refractive error may be an option in the treatment of masticatory muscle pathology. This phenomenon requires further research.
REFERENCES (33)
1.
Cashell G. A Short History of Spectacles. Proc R Soc Med. 1971; 64: 1063–1064.
2.
Berthold L. Mitteilungen zur Geschichte der Medizin und der Naturwissenschaften; Deutsche Gesellschaft für Geschichte der Medizin, Natur und Tech. 1907; 6: 26.
3.
Flitcroft DL, He M, Jonas JB, et al. IMI – Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies. Invest Ophthalmol Vis Sci. 2019; 60: M20–M30, doi:10.1167/iovs.18-25957.
4.
Baird PN, Saw S-M, Lanca C, et al. Myopia. Nat Rev Dis Primers. 2020; 6: 99, doi:10.1038/s41572-020-00231-4.
5.
Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmol. 2016; 123: 1036–1042, doi:10.1016/j.ophtha.2016.01.006.
6.
Carr BJ, Stell WK. The Science Behind Myopia. In Webvision: The Organization of the Retina and Visual System. Kolb H, Fernandez E, Nelson R, (editors). University of Utah Health Sciences Center: Salt Lake City (UT); 1995. PMID: 29266913.
7.
Haarman AEG, Enthoven CA, Tideman JWL, et al. The Complications of Myopia: A Review and Meta-Analysis. Invest Ophthalmol Vis Sci. 2020; 61: 49, doi:10.1167/iovs.61.4.49.
8.
Williams K, Hammond C. High Myopia and Its Risks. Community Eye Health. 2019; 32: 5–6.
9.
Hu M, Zhou Y, Huang S, et al. Population Prevalence of Myopia, Glasses Wear and Free Glasses Acceptance among Minority versus Han Schoolchildren in China. PLoS One. 2019; 14: e0215660, doi:10.1371/journal.pone.0215660.
10.
Yazdani N, Sadeghi R, Ehsaei A, et al. Under-Correction or Full Correction of Myopia? A Meta-Analysis. J Optom. 2021; 14: 11–19, doi:10.1016/j.optom.2020.04.003.
11.
Monaco A, Cattaneo R, Spadaro A, et al. Visual Input Effect on EMG Activity of Masticatory and Postural Muscles in Healthy and in Myopic Children. Eur J Paediatr Dent. 2006; 7: 18–22.
12.
Zieliński G, Matysik-Woźniak A, Rapa M, et al. The Influence of Visual Input on Electromyographic Patterns of Masticatory and Cervical Spine Muscles in Subjects with Myopia. J Clin Med. 2021; 10: 5376, doi:10.3390/jcm10225376.
13.
Zieliński G, Suwała M, Ginszt M, et al. Bioelectric Activity of Mastication Muscles and the Functional Impairment Risk Groups Concerning the Masticatory Muscles. Acta Bioeng Biomech. 2018; 20: 161–166.
14.
Osiewicz MA, Lobbezoo F, Loster BW, et al. Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD): The Polish Version of a Dual-Axis System for the Diagnosis of TMD.* RDC/TMD Form. J Stoma. 2013; 66: 576–649.
15.
Al-Khotani A, Naimi-Akbar A, Albadawi E, et al. Prevalence of Diagnosed Temporomandibular Disorders among Saudi Arabian Children and Adolescents. J Headache Pain. 2016; 17: 41, doi:10.1186/s10194-016-0642-9.
16.
Ey-Chmielewska H, Teul I, LorkowskI J. Functional Disorders Of The Temporomandibular Joints As A Factor Responsible For Sleep Apnoea. Ann Acad Med Stetin. 2014; 60: 65–68.
17.
Facial Pain | National Institute of Dental and Craniofacial Research Available online: http://www.nidcr.nih.gov/resea... (accessed on 1 March 2018).
18.
Abouelhuda AM, Kim H-S, Kim S-Y, Kim Y-K. Association between Headache and Temporomandibular Disorder. J Korean Assoc Oral Maxillofac Surg. 2017; 43: 363–367, doi:10.5125/jkaoms.2017.43.6.363.
19.
Speciali JG, Dach F. Temporomandibular Dysfunction and Headache Disorder. Headache. 2015; 55 Suppl 1: 72–83, doi:10.1111/head.12515.
20.
Hara K, Shinozaki T, Okada-Ogawa A, et al. Headache Attributed to Temporomandibular Disorders and Masticatory Myofascial Pain. J Oral Sci. 2016; 58: 195–204, doi:10.2334/josnusd.15-0491.
21.
Azzam D, Ronquillo Y. Snellen Chart. In StatPearls; StatPearls Publishing: Treasure Island (FL). 2021. PMID: 32644387.
22.
Tsui E, Patel P. Calculated Decisions: Visual Acuity Testing (Snellen Chart). Emerg Med Pract. 2020; 22: CD1–CD2.
23.
Ginszt M, Zieliński G. Novel Functional Indices of Masticatory Muscle Activity. J Clin Med. 2021; 10: 1440. doi:10.3390/jcm10071440.
24.
Zieliński G, Byś A, Ginszt M, et al. Depression and Resting Masticatory Muscle Activity. J Clin Med. 2020; 9(4): 1097. doi:10.3390/jcm9041097.
25.
Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of Recommendations for SEMG Sensors and Sensor Placement Procedures. J Electromyogr Kinesiol. 2000; 10: 361–374.
26.
Cohen J. Statistical Power Analysis for the Behavioral Sciences.; Elsevier Science: Burlington, 2013; ISBN 978-1-4832-7648-9.
27.
Zieliński G, Filipiak Z, Ginszt M, et al. The Organ of Vision and the Stomatognathic System—Review of Association Studies and Evidence-Based Discussion. Brain Sciences. 2022; 12: 14, doi:10.3390/brainsci12010014.
28.
Somisetty S, M Das J. Neuroanatomy, Vestibulo-Ocular Reflex. In StatPearls; StatPearls Publishing: Treasure Island (FL), 2021. PMID: 31424881.
29.
Stack B, Sims A. The Relationship between Posture and Equilibrium and the Auriculotemporal Nerve in Patients with Disturbed Gait and Balance. Cranio. 2009; 27: 248–260. doi:10.1179/crn.2009.036.
30.
Büttner-Ennever JA, Büttner U. Neuroanatomy of the Oculomotor System. The Reticular Formation. Rev Oculomot Res. 1988; 2: 119–176.
31.
Bradnam L, Barry C. The Role of the Trigeminal Sensory Nuclear Complex in the Pathophysiology of Craniocervical Dystonia. J Neurosci. 2013; 33: 18358–18367, doi:10.1523/JNEUROSCI.3544-13.2013.
32.
Akinci A, Güven A, Degerliyurt A, et al. The Correlation between Headache and Refractive Errors. J AAPOS. 2008; 12: 290–293, doi:10.1016/j.jaapos.2007.11.018.
33.
Lajmi H, Choura R, Ben Achour B, et al. Headache Associated with Refractive Errors: Characteristics and Risk Factors. Rev Neurol (Paris). 2021; 177: 947–954, doi:10.1016/j.neurol.2020.10.008.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.