Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Use of neural network based on international classification ICD-10 in patients with head and neck injuries in Lublin Province, Poland, between 2006–2018, as a predictive value of the outcomes of injury sustained
1
Chair and Department of Trauma Surgery and Emergency Medicine, Medical University, Lublin, Poland
2
Department of Machine Design and Mechatronics, Faculty of Mechanical Engineering, University of Technology, Lublin,
Poland
3
I Department of Psychiatry, Psychotherapy and Early Intervention, Medical University, Lublin, Poland
4
Orthopaedic Department, Łęczna Hospital, Poland
5
Department of Computer Science, Faculty of Electrical Engineering and Computer Science, University of Technology, Lublin, Poland
Corresponding author
Mariusz Jojczuk
Chair and Department of Trauma Surgery and Emergency Medicine, Medical University of Lublin, Staszica 11, 20-081, Lublin, Poland
Chair and Department of Trauma Surgery and Emergency Medicine, Medical University of Lublin, Staszica 11, 20-081, Lublin, Poland
Ann Agric Environ Med. 2023;30(2):281-286
KEYWORDS
headTBIinjuryneckmortalityArtificial Neural Networkartificial intelligencemortality predictiontrauma scoring systeminjury scoring system
TOPICS
ABSTRACT
Introduction and objective:
Head and neck injuries are a heterogeneous group in terms of both clinical course and prognosis. For years, there have been attempts to create an ideal tool to predict the outcomes and severity of injuries. The aim of this study was evaluation of the use of selected artificial intelligence methods for outcome predictions of head and neck injuries.
Material and methods:
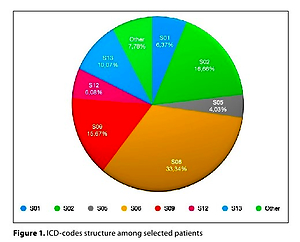
6,824 consecutive cases of patients who sustained head and neck injuries, treated in hospitals in the Lublin Province between 2006–2018, whose data was provided by National Institute of Public Health / National Institute of Hygiene, were analyzed retrospectively. Patients were qualified using International Statistical Classification of Diseases and Related Health Problems (10th Revision). The multilayer perceptron (MLP) structure was utilized in numerical studies. Neural network training was achieved with the Broyden-Fletcher-Goldfarb-Shanno (BFGS) method.
Results:
In the designed network, the highest classification efficiency was obtained for the group of deaths (80.7%). The average value of correct classifications for all analyzed cases was 66%. The most important variable influencing the prognosis of an injured patient was diagnosis (weight 1.929). Gender and age were variables of less significance with weight 1.08 and 1.073, respectively.
Conclusions:
Designing a neural network was hindered due to the large amount of cases and linking of a large number of deaths with specific diagnosis (S06). With a predictive value of 80.7% for mortality, ANN can be a promising tool in the future; however, additional variables should be introduced into the algorithm to increase the predictive value of the network. Further studies, including other types of injuries and additional variables, are needed to introduce this method into clinical use.
Head and neck injuries are a heterogeneous group in terms of both clinical course and prognosis. For years, there have been attempts to create an ideal tool to predict the outcomes and severity of injuries. The aim of this study was evaluation of the use of selected artificial intelligence methods for outcome predictions of head and neck injuries.
Material and methods:
6,824 consecutive cases of patients who sustained head and neck injuries, treated in hospitals in the Lublin Province between 2006–2018, whose data was provided by National Institute of Public Health / National Institute of Hygiene, were analyzed retrospectively. Patients were qualified using International Statistical Classification of Diseases and Related Health Problems (10th Revision). The multilayer perceptron (MLP) structure was utilized in numerical studies. Neural network training was achieved with the Broyden-Fletcher-Goldfarb-Shanno (BFGS) method.
Results:
In the designed network, the highest classification efficiency was obtained for the group of deaths (80.7%). The average value of correct classifications for all analyzed cases was 66%. The most important variable influencing the prognosis of an injured patient was diagnosis (weight 1.929). Gender and age were variables of less significance with weight 1.08 and 1.073, respectively.
Conclusions:
Designing a neural network was hindered due to the large amount of cases and linking of a large number of deaths with specific diagnosis (S06). With a predictive value of 80.7% for mortality, ANN can be a promising tool in the future; however, additional variables should be introduced into the algorithm to increase the predictive value of the network. Further studies, including other types of injuries and additional variables, are needed to introduce this method into clinical use.
REFERENCES (55)
1.
Moses H, Powers D, Keeler J, et al. Opportunity Cost of Surgical Management of Craniomaxillofacial Trauma. Craniomaxillofacial Trauma & Reconstruction. 2016;9(1):076–081. doi:10.1055/s-0035-1566160.
2.
Centers for Disease Control and Prevention. (2015). Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. National Center for Injury Prevention and Control; Division of Unintentional Injury Prevention. Atlanta, GA. Published January 31, 2019. Accessed June 7, 2022. https://www.cdc.gov/traumaticb....
3.
Sethi RKV, Kozin ED, Fagenholz PJ, Lee DJ, Shrime MG, Gray ST. Epidemiological survey of head and neck injuries and trauma in the United States. Otolaryngol Head Neck Surg. 2014;151(5):776–784. doi:10.1177/0194599814546112.
4.
Mohamed A, Mulcaire J, Clover AJP. Head and neck injury in major trauma in Ireland: a multicentre retrospective analysis of patterns and surgical workload. Ir J Med Sci. 2021;190(1):395–401. doi:10.1007/s11845-020-02304-5.
5.
Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic Brain Injury–Related Emergency Department Visits, Hospitalizations, and Deaths — United States, 2007 and 2013. MMWR Surveill Summ. 2017;66(9):1–16. doi:10.15585/mmwr.ss6609a1.
6.
Sandstrom CK, Nunez DB. Head and Neck Injuries: Special Considerations in the Elderly Patient. Neuroimaging Clin N Am. 2018;28(3):471–481. doi:10.1016/j.nic.2018.03.008.
7.
Peeters W, van den Brande R, Polinder S, et al. Epidemiology of traumatic brain injury in Europe. Acta Neurochir (Wien). 2015;157(10):1683–1696. doi:10.1007/s00701-015-2512-7.
8.
Andersson EH, Björklund R, Emanuelson I, Stålhammar D. Epidemiology of traumatic brain injury: a population based study in western Sweden. Acta Neurol Scand. 2003;107(4):256–259. doi:10.1034/j.1600-0404.2003.00112.x.
9.
Peterson AB, Zou H, Thomas KE, Daugherty J. Traumatic Brain Injury-related Hospitalizations and Deaths by Age Group, Sex And Mechanism of Injury: United States 2016/2017 URL: https://stacks.cdc.gov/view/cd....
10.
Majdan M, Plancikova D, Brazinova A, et al. Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis. Lancet Public Health. 2016;1(2):e76-e83. doi:10.1016/S2468-2667(16)30017-2.
11.
Fakhry SM, Morse JL, Garland JM, et al. Redefining geriatric trauma: 55 is the new 65. J Trauma Acute Care Surg. 2021;90(4):738–743. doi:10.1097/TA.0000000000003062.
12.
Rogers FB, Morgan ME, Brown CT, et al. Geriatric Trauma Mortality: Does Trauma Center Level Matter? Am Surgeon. 2021;87(12):1965–1971. doi:10.1177/0003134820983190.
13.
Faul M, Wald MM, Rutland-Brown W, Sullivent EE, Sattin RW. Using a Cost-Benefit Analysis to Estimate Outcomes of a Clinical Treatment Guideline: Testing the Brain Trauma Foundation Guidelines for theTreatment of Severe Traumatic Brain Injury. J Trauma: Injury Infect Critical Care. 2007;63(6):1271–1278. doi:10.1097/TA.0b013e3181493080.
14.
van Dijck JTJM, Dijkman MD, Ophuis RH, de Ruiter GCW, Peul WC, Polinder S. In-hospital costs after severe traumatic brain injury: A systematic review and quality assessment. PLoS ONE. 2019;14(7):e0219529. doi:10.1371/journal.pone.0219529.
15.
Maas AIR, Menon DK, Adelson PD, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16(12):987–1048. doi:10.1016/S1474–4422(17)30371-X.
16.
Civil ID, Schwab CW. The Abbreviated Injury Scale, 1985 Revision: A Condensed Chart For Clinical Use: J Trauma: Injury Infect Critical Care. 1988;28(1):87–90. doi:10.1097/00005373–198801000–00012.
17.
Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the Trauma Score. J Trauma. 1989;29(5):623–629. doi:10.1097/00005373–198905000–00017.
18.
Baker SP, O'neill B. The injury severity score: an update. J Trauma Injury Infect Critical Care. 1976;16(11):882–885. doi:10.1097/00005373–197611000–00006.
19.
Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma. 1997;43(6):922–925; discussion 925–926. doi:10.1097/00005373–199712000–00009.
20.
Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma. 1987;27(4):370–378.
21.
Osler T, Rutledge R, Deis J, Bedrick E. ICISS: an international classification of disease-9 based injury severity score. J Trauma. 1996;41(3):380–386; discussion 386–388. doi:10.1097/00005373–199609000–00002.
22.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. The Lancet. 1974;304(7872):81–84. doi:10.1016/S0140–6736(74)91639–0.
23.
Mena JH, Sanchez AI, Rubiano AM, et al. Effect of the Modified Glasgow Coma Scale Score Criteria for Mild Traumatic Brain Injury on Mortality Prediction: Comparing Classic and Modified Glasgow Coma Scale Score Model Scores of 13. J Trauma Injury Infect Critical Care. 2011;71(5):1185–1193. doi:10.1097/TA.0b013e31823321f8.
24.
Gagné M, Moore L, Beaudoin C, Batomen Kuimi BL, Sirois MJ. Performance of International Classification of Diseases-based injury severity measures used to predict in-hospital mortality: A systematic review and meta-analysis. J Trauma Acute Care Surg. 2016;80(3):419–426. doi:10.1097/TA.0000000000000944.
25.
Nogalski A. Wykorzystanie Klasyfikacji ICD-10 Do Określenia Ciężkości Obrażeń Na Podstawie Współczynników Ryzyka Dla Populacji Poszkodowanych w Wyniku Urazów w Regionie Lubelskim: Praca Na Stopień Doktora Habilitowanego Nauk Medycznych. Instytut Zastosowań Techniki; 2008.
26.
Jojczuk M, Nogalski A, Krakowski P, Prystupa A. Mortality prediction by ‘Life Threat Index’ compared to widely used trauma scoring systems. Ann Agric Environ Med. 2022;29(2):258–263. doi:10.26444/aaem/142182.
27.
Peng J, Xiang H. Trauma undertriage and overtriage rates: are we using the wrong formulas? Am J Emergency Med. 2016;34(11):2191–2192. doi:10.1016/j.ajem.2016.08.061.
28.
Elgin LB, Appel SJ, Grisham D, Dunlap S. Comparisons of Trauma Outcomes and Injury Severity Score. J Trauma Nurs. 2019;26(4):199–207. doi:10.1097/JTN.0000000000000449.
29.
Skinner HG, Blanchard J, Elixhauser A. Trends in Emergency Department Visits, 2006–2011. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2006. Accessed August 22, 2022. http://www.ncbi.nlm.nih.gov/bo....
30.
Hosny A, Parmar C, Quackenbush J, Schwartz LH, Aerts HJWL. Artificial intelligence in radiology. Nat Rev Cancer. 2018;18(8):500–510. doi:10.1038/s41568–018–0016–5.
31.
Syed A, Zoga A. Artificial Intelligence in Radiology: Current Technology and Future Directions. Semin Musculoskelet Radiol. 2018;22(05):540–545. doi:10.1055/s-0038–1673383.
32.
Karpiński R, Krakowski P, Jonak J, Machrowska A, Maciejewski M, Nogalski A. Diagnostics of Articular Cartilage Damage Based on Generated Acoustic Signals Using ANN—Part I: Femoral-Tibial Joint. Sensors. 2022;22(6):2176. doi:10.3390/s22062176.
33.
Karpiński R, Krakowski P, Jonak J, Machrowska A, Maciejewski M, Nogalski A. Diagnostics of Articular Cartilage Damage Based on Generated Acoustic Signals Using ANN—Part II: Patellofemoral Joint. Sensors. 2022;22(10):3765. doi:10.3390/s22103765.
34.
Karpiński R. Knee joint osteoarthritis diagnosis based on selected acoustic signal discriminants using machine learning. Applied Computer Sci. 2022;18(2):71–85. doi:10.35784/acs-2022–14.
35.
Kheradvar A, Jafarkhani H, Guy TS, Finn JP. Prospect of artificial intelligence for the assessment of cardiac function and treatment of cardiovascular disease. Future Cardiol. 2021;17(2):183–187. doi:10.2217/fca-2020–0128.
36.
Syaifullah AH, Shiino A, Kitahara H, Ito R, Ishida M, Tanigaki K. Machine Learning for Diagnosis of AD and Prediction of MCI Progression From Brain MRI Using Brain Anatomical Analysis Using Diffeomorphic Deformation. Front Neurol. 2021;11:576029. doi:10.3389/fneur.2020.576029.
37.
Institute for Systems and Technologies of Information, Control and Communication, ed. VISIGRAPP 2020: Proceedings of the 15th International Joint Conference on Computer Vision, Imaging and Computer Graphics Theory and Applications: Valletta, Malta, February 27–29, 2020. SCITEPRESS – Science and Technology Publications, Lda; 2020.
38.
Penny W, Frost D. Neural Networks in Clinical Medicine. Med Decis Making. 1996;16(4):386–398. doi:10.1177/0272989X9601600409.
39.
Lang E, Pitts L, Damron S, Rutledge R. Outcome after severe head injury: An analysis of prediction based upon comparison of neural network versus logistic regression analysis. Neurological Res. 1997;19(3):274–280. doi:10.1080/01616412.1997.11740813.
40.
Maurer LR, Bertsimas D, Bouardi HT, et al. Trauma outcome predictor: An artificial intelligence interactive smartphone tool to predict outcomes in trauma patients. J Trauma Acute Care Surg. 2021;91(1):93–99. doi:10.1097/TA.0000000000003158.
41.
Cardosi JD, Shen H, Groner JI, Armstrong M, Xiang H. Machine learning for outcome predictions of patients with trauma during emergency department care. BMJ Health Care Inform. 2021;28(1):e100407. doi:10.1136/bmjhci-2021–100407.
42.
Klug M, Barash Y, Bechler S, et al. A Gradient Boosting Machine Learning Model for Predicting Early Mortality in the Emergency Department Triage: Devising a Nine-Point Triage Score. J Gen Intern Med. 2020;35(1):220–227. doi:10.1007/s11606–019–05512–7.
43.
Rau CS, Kuo PJ, Chien PC, Huang CY, Hsieh HY, Hsieh CH. Mortality prediction in patients with isolated moderate and severe traumatic brain injury using machine learning models. Kou YR, ed. PLoS ONE. 2018;13(11):e0207192. doi:10.1371/journal.pone.0207192.
44.
Hale AT, Stonko DP, Brown A, et al. Machine-learning analysis outperforms conventional statistical models and CT classification systems in predicting 6-month outcomes in pediatric patients sustaining traumatic brain injury. Neurosurgical Focus. 2018;45(5):E2. doi:10.3171/2018.8.FOCUS17773.
45.
Tsiklidis EJ, Sims C, Sinno T, Diamond SL. Using the National Trauma Data Bank (NTDB) and machine learning to predict trauma patient mortality at admission. PLoS One. 2020;15(11):e0242166. doi:10.1371/journal.pone.0242166.
46.
Mou Z, Godat LN, El-Kareh R, Berndtson AE, Doucet JJ, Costantini TW. Electronic health record machine learning model predicts trauma inpatient mortality in real time: A validation study. J Trauma Acute Care Surg. 2022;92(1):74–80. doi:10.1097/TA.0000000000003431.
47.
Pearl A, Caspi R, Bar-Or D. Artificial Neural Network Versus Subjective Scoring in Predicting Mortality in Trauma Patients. Stud Health Technol Inform. 2006;124:1019–1024.
48.
Majdan M, Brazinova A, Rusnak M, Leitgeb J. Outcome Prediction after Traumatic Brain Injury: Comparison of the Performance of Routinely Used Severity Scores and Multivariable Prognostic Models. J Neurosci Rural Pract. 2017;08(01):020–029. doi:10.4103/0976–3147.193543.
49.
Berecki-Gisolf J, Tharanga Fernando D, D’Elia A. International classification of disease based injury severity score (ICISS): A data linkage study of hospital and death data in Victoria, Australia. Injury. 2022;53(3):904–911. doi:10.1016/j.injury.2022.01.011.
50.
Allen CJ, Baldor DJ, Schulman CI, Pizano LR, Livingstone AS, Namias N. Assessing Field Triage Decisions and the International Classification Injury Severity Score (ICISS) at Predicting Outcomes of Trauma Patients. Am Surgeon. 2017;83(6):648–652. doi:10.1177/000313481708300632.
51.
Tran Z, Zhang W, Verma A, et al. The derivation of an International Classification of Diseases, Tenth Revision–based trauma-related mortality model using machine learning. J Trauma Acute Care Surg. 2022;92(3):561–566. doi:10.1097/TA.0000000000003416.
52.
Christie SA, Conroy AS, Callcut RA, Hubbard AE, Cohen MJ. Dynamic multi-outcome prediction after injury: Applying adaptive machine learning for precision medicine in trauma. Kou YR, ed. PLoS ONE. 2019;14(4):e0213836. doi:10.1371/journal.pone.0213836.
53.
Raj R, Luostarinen T, Pursiainen E, et al. Machine learning-based dynamic mortality prediction after traumatic brain injury. Sci Rep. 2019;9(1):17672. doi:10.1038/s41598–019–53889–6.
54.
Hsu MH, Li YC, Chiu WT, Yen JC. Outcome Prediction after Moderate and Severe Head Injury Using an Artificial Neural Network. Stud Health Technol Inform. 2005;116:241-5.
55.
Poznańska A, Goryński P, Seroka W, Stokwiszewski J, Radomski P, Wojtyniak B. Nationwide General Hospital Morbidity Study as a source of data about Polish population health. Przegl Epidemiol. Published online 2019:69–80. doi:10.32394/pe.73.08.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.