Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Socioeconomic characteristic of burned children families
1
University of Wrocław, Poland
2
Marciniak Hospital, Wrocław, Poland
3
Medical University, Wrocław, Poland
Ann Agric Environ Med. 2022;29(3):417-423
KEYWORDS
TOPICS
ABSTRACT
Objective:
The aim of the study was to determine the relationship between the socioeconomic factors and chosen parameters of burns in children.
Material and methods:
An anonymous survey was conducted among caregivers of 200 children hospitalized due to burns in 5 Polish hospitals. The socioeconomic factors and location of the burn, surface of the burn, depth of the injury, type of treatment, and length of hospitalization were analyzed. Statistical analysis was performed using Statistica v.12.
Results:
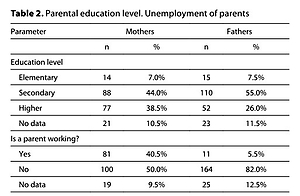
Single parenthood was related with longer hospitalisation of the child, higher degree of burn wound, and more frequent operative treatment (p < 0.05). Children from families with several children (≥3) more often had severe burns than the only children (p = 0.018). A statistically significant relationship was observed between fathers’ age and the surface of burn wound, burn depth, burn severity, type of required treatment, and duration of hospitalization (p < 0.05). In the group of children with minor burns, the percentage of mothers with secondary education was lower than in mothers with primary education (p = 0.004) and with higher education (p = 0.006). In the group with average burns, the proportion of mothers with secondary education was higher than with primary education (p = 0.019). In the group of children with severe burns, the percentage of fathers with primary education was higher than the percentage of fathers with secondary (p = 0.005) and higher education (p = 0.018). The surface of burn was higher in children those fathers had lower education (p < 0.05). Fathers’ unemployment was related to higher surface of burn in children (p < 0.05).
Conclusions:
The relationship between socioeconomic factors and analyzed parameters of burns is important to identify the groups for which preventive actions should be designed.
The aim of the study was to determine the relationship between the socioeconomic factors and chosen parameters of burns in children.
Material and methods:
An anonymous survey was conducted among caregivers of 200 children hospitalized due to burns in 5 Polish hospitals. The socioeconomic factors and location of the burn, surface of the burn, depth of the injury, type of treatment, and length of hospitalization were analyzed. Statistical analysis was performed using Statistica v.12.
Results:
Single parenthood was related with longer hospitalisation of the child, higher degree of burn wound, and more frequent operative treatment (p < 0.05). Children from families with several children (≥3) more often had severe burns than the only children (p = 0.018). A statistically significant relationship was observed between fathers’ age and the surface of burn wound, burn depth, burn severity, type of required treatment, and duration of hospitalization (p < 0.05). In the group of children with minor burns, the percentage of mothers with secondary education was lower than in mothers with primary education (p = 0.004) and with higher education (p = 0.006). In the group with average burns, the proportion of mothers with secondary education was higher than with primary education (p = 0.019). In the group of children with severe burns, the percentage of fathers with primary education was higher than the percentage of fathers with secondary (p = 0.005) and higher education (p = 0.018). The surface of burn was higher in children those fathers had lower education (p < 0.05). Fathers’ unemployment was related to higher surface of burn in children (p < 0.05).
Conclusions:
The relationship between socioeconomic factors and analyzed parameters of burns is important to identify the groups for which preventive actions should be designed.
REFERENCES (56)
1.
Tran S, Jacques MA, Holland AJ. Assessment and management of minor burns in children. Aust J Gen Pract. 2019;48(9):590–594. doi:10.31128/AJGP-04-19-4919.
2.
Norbury WB, Herndon DN. Management of Acute Pediatric Hand Burns. Hand Clin. 2017;33(2):237–242. doi:10.1016/j.hcl.2016.12.002.
3.
Alnababtah K, Khan S. Socio-demographic factors which significantly relate to the prediction of burns severity in children. Int J Burns Trauma. 2017;7(5):56–63.
4.
Pediatric Disaster Branch of Chinese Pediatric Society of Chinese Medical Association; Pediatric Branch of Chinese People’s Liberation Army (Zheng C-Z). Expert consensus on the prevention and first-aid management of burns in children. Zhongguo Dang Dai Er Ke Za Zhi. 2021;23(12):1191–1199. doi:10.7499/j.issn.1008-8830.2109026.
5.
Loos M-LHJ, Almekinders CAM, Heymans MW, et al. Incidence and characteristics of non-accidental burns in children: A systematic review. Burns. 2020; 46(6):1243–1253. https://doi.org/10.1016/j.burn....
6.
Mathur A, Mehra L, Diwan V, et al. Unintentional Childhood Injuries in Urban and Rural Ujjain, India: A Community-Based Survey. Children. 2018; 5(2): 23. https://doi.org/10.3390/childr....
7.
Keshavarz M, Javanmardi F, Mohammdi AA. A Decade Epidemiological Study of Pediatric Burns in South West of Iran. World J Plast Surg. 2020;9(1):67–72. doi:10.29252/wjps.9.1.67.
8.
Trop M, Herzog SA, Pfurtscheller K, et al. The past 25 years of pediatric burn treatment in Graz and important lessons been learned. An overview. Burns. 2015;41(4):714–720. https://doi.org/10.1016/j.burn....
9.
Gabbe BJ, Watterson DM, Singer Y, et al. Outpatient presentations to burn centers: Data from the Burns Registry of Australia and New Zealand outpatient pilot project. Burns. 2015; 41(3): 446–453. https://doi.org/10.1016/j.burn....
10.
Goltsman D, Li Z, Bruce E, et al. Spatial analysis of pediatric burns shows geographical clustering of burns and ‘hotspots’ of risk factors in New South Wales, Australia. Burns. 2016;42(4):754–762. https://doi.org/10.1016/j.burn....
11.
Dhopte A, Bamal R, Tiwari VK. A prospective analysis of risk factors for pediatric burn mortality at a tertiary burn center in North India. Burns & Trauma, 2017;5:30. https://doi.org/10.1186/s41038....
12.
Lee CJ, Mahendraraj K, Houng A, et al. Pediatric burns: a single institution retrospective review of incidence, etiology, and outcomes in 2273 burn patients (1995–2013). J Burn Care Res. 2016;37(6):e579-e585. https://doi.org/10.1097/BCR.00....
13.
Kawalec A. Environmental factors of burns in children – review. Medycyna Środowiskowa – Environmental Medicine. 2015;18(3):40–46.
14.
Emond A, Sheahan C, Mytton J, et al. Developmental and behavioural associations of burns and scalds in children: a prospective population-based study. Arch Dis Child. 2017;102(5):428–483. doi:10.1136/archdischild-2016-311644.
15.
Kawalec A, Pawlas K. Struktura oparzeń wśród dzieci na Dolnym Śląsku (Polska). Probl Hig Epidemiol. 2014;95(2):394–399.
16.
Kawalec A, Kawalec A, Pawlas K. Struktura oparzeń wśród dzieci na Dolnym Śląsku (Polska). Część II. Probl Hig Epidemiol. 2014;95(3): 744–747.
17.
Lam NN, Hung NT, Duc NM, et al. Epidemiology And Risk Factors For Death Of Pediatric Burns In A Developing Country. An Experience From The National Burn Hospital. Ann Burns Fire Disasters. 2021;34(3):213–217.
18.
Kawalec A. The changes in the number of patients admissions due to burns in Paediatric Trauma Centre in Wroclaw (Poland) in March 2020. Burns. 2020;46(7):1713–1714. doi: 10.1016/j.burns.2020.05.007.
19.
Charvillat O, Plancq M-C, Haraux E, et al. Epidemiological analysis of burn injuries in children during the first COVID-19 lockdown, and a comparison with the previous five yearsAnalyse épidémiologique des brulures chez les enfants pendant le premier confinement COVID-19 et comparaison avec les cinq années précédentes. Annales de Chirurgie Plastique Esthétique. 2021;66(4):285–290. https://doi.org/10.1016/j.anpl....
20.
Sanford EL, Zagory J, Blackwell J-M, et al. Changes in pediatric trauma during COVID-19 stay-at-home epoch at a tertiary pediatric hospital. J Pediatric Surg. 2021;56(5):918–922. https://doi.org/10.1016/j.jped....
21.
Williams FN, Chrisco L, Nizamani R, et al. COVID-19 related admissions to a regional burn center: The impact of shelter-in-place mandate. Burns Open. 2020;4(4):158–159. https://doi.org/10.1016/j.burn....
22.
Sethuraman U, Stankovic C, Singer A, et al. Burn visits to a pediatric burn center during the COVID-19 pandemic and ‘Stay at home’ period. Burns. 2021;47(2):491–492. doi:10.1016/j.burns.2020.08.004.
23.
Kuzański W. Oparzenia u dzieci. In: Tkaczyk M, editor. Stany nagłe. Pediatria. 2nd ed. Warszawa: Medical Tribune Polska; 2018. p. 251–267.
24.
Collier ZJ, Ramaiah V, Glick JC, et al. A 6-Year Case-Control Study of the Presentation and Clinical Sequelae for Noninflicted, Negligent, and Inflicted Pediatric Burns. J Burn Care Res. 2017;38(1):e101-e124. doi:10.1097/BCR.0000000000000408.
25.
Borg BA, Durgham M, Shanti CM, et al. Sink bathing burns: A unique opportunity for an injury prevention initiative. Burns. 2020;46(8): 1875–1879. https://doi.org/10.1016/j.burn....
26.
Sözen I, Güldogan CE, Yasti AÇ. Etiology of childhood burns and parental awareness in Turkey. Ulus Cerrahi Derg. 2015;32(3):168–172. doi:10.5152/UCD.2016.3285.
27.
Elsous A, Salah M, Ouda M. Childhood burns: an analysis of 124 admissions in the Gaza Strip. Ann Burns Fire Disasters. 2015;28(4):253–258.
28.
Ibrahem AM, Rashed KJ, Babakir-Mina M, et al. Mother’s characteristics, knowledge and practices about children burn injury in Sulaimani City. Kurdistan J Applied Res. 2017; 2(2), 6–12. https://doi.org/10.24017/scien....
29.
Laursen B, Nielsen JW. Influence of sociodemographic factors on the risk of unintentional childhood home injuries. Eur J Public Health. 2008;18(4):366–70. doi: 10.1093/eurpub/ckn034.
30.
Laitakari E, Koljonen V, Rintala R, et al. Incidence and risk factors of burn injuries among infants, Finland 1990–2010. J Pediatr Surg. 2015;50(4):608–12. doi: 10.1016/j.jpedsurg.2014.05.034.
31.
Karan A, Amado V, Vitorino P, et al. Evaluating the socioeconomic and cultural factors associated with pediatric burn injuries in Maputo, Mozambique. Pediatr Surg Int. 2015; 31(11):1035–40. doi: 10.1007/s00383-015-3761-5.
32.
Shai D, Lupinacci P. Fire fatalities among children: an analysis across Philadelphia’s census tracts. Public Health Rep. 2003;118(2):115–26. doi: 10.1016/S0033-3549(04)50226-1.
33.
Mashreky SR, Rahman A, Khan TF, et al. Determinants of childhood burns in rural Bangladesh: A nested case-control study. Health Policy. 2010;96(3):226–30. doi: 10.1016/j.healthpol.2010.02.004.
34.
Mercier C, Blond MH. Epidemiological survey of childhood burn injuries in France. Burns. 1996;22(1):29–34. doi: 10.1016/0305-4179(95)00073-9.
35.
Mercier C, Blond MH. Enquete épidémiologique française sur la brl^ure de l’enfant de 0 a 5 ans. Archives de Pédiatrie. 1995; 2(10): 949–956. doi: 10.1016/0929-693X(96)89890-3.
36.
Heng JS, Atkins J, Clancy O, et al. Geographical analysis of socioeconomic factors in risk of domestic burn injury in London 2007–2013. Burns. 2015;41(3):437–45. doi: 10.1016/j.burns.2014.12.001.
37.
Aghaei A, Mehrabi Y, Ramezankhani A, et al. Factors related to pediatric burn in Iran: A case-control study. Int J Pediatrics. 2018;6(6), 7823–7832.
38.
Joseph KE, Adams CD, Goldfarb IW, et al. Parental correlates of unintentional burn injuries in infancy and early childhood. Burns. 2002;28:455–463. doi: 10.1016/S0305-4179(02)00035-9.
39.
Tajiki I, Vizeshfar F, Keshtkaran Z. The effect of training program based on health belief model on burn prevention knowledge in mothers of children aged to 1–3 years: A randomized controlled. Burns. 2021;16:S0305-4179(21)00309-0. doi: 10.1016/j.burns.2021.11.001.
40.
D’cunha A, Rebekah G, Mathai J, et al. Understanding burn injuries in children—A step toward prevention and prompt first aid. Burns. 2021;24:S0305-4179(21)00190-X. doi: 10.1016/j.burns.2021.07.010.
41.
Khandarmaa TO, Harun-Or-Rashid M, Sakamoto J. Risk factors of burns among children in Mongolia. Burns. 2012;38(5):751–7. doi: 10.1016/j.burns.2011.11.006.
42.
El-Badawy A, Mabrouk AR. Epidemiology of childhood burns in the burn unit of Ain Shams University in Cairo, Egypt. Burns. 1998;24(8):728–32. doi: 10.1016/s0305-4179(98)00097-7.
43.
Forjuoh SN, Guyer B, Strobino DM, et al. Risk factors for childhood burns: a case-control study of Ghanaian children. J Epidemiol Community Health. 1995;49(2):189–93. doi: 10.1136/jech.49.2.189.
44.
Delgado J, Ramírez-Cardich ME, Gilman RH, et al. Risk factors for burns in children: crowding, poverty, and poor maternal education. Inj Prev. 2002;8(1):38–41. doi: 10.1136/ip.8.1.38.
45.
Wang S, Li D, Shen C, et al. Epidemiology of burns in pediatric patients of Beijing City. BMC pediatrics. 2016; 16(1): 1–7. doi: 10.1186/s12887-016-0686-7.
46.
Niekerk AV, Reimers A, Laflamme L. Area characteristics and determinants of hospitalised childhood burn injury: a study in the city of Cape Town. Public Health. 2006;120(2):115–24. doi: 10.1016/j.puhe.2005.08.015.
47.
Colvin JD, Richardson T, Ginther DK, et al. Economy-Sensitive Conditions: Are Some Pediatric Hospitalizations Triggered By Economic Recessions? Health Aff (Millwood). 2020;39(10):1783–1791. doi: 10.1377/hlthaff.2020.00732.
48.
Dinesh A, Polanco T, Khan K, et al. Our Inner-city Children Inflicted With Burns: A Retrospective Analysis of Pediatric Burn Admissions at Harlem Hospital, NY. J Burn Care Res. 2018;23;39(6):995–999. doi: 10.1093/jbcr/iry026.
49.
Dedovic Z, Brychta P, Koupilová I, et al. Epidemiology of childhood burns at the Burn Centre in Brno, Czech Republic. Burns. 1996;22(2):125–129. doi: 10.1016/0305-4179(95)00106-9.
50.
Gyedu A, Nakua EK, Otupiri E, et al. Incidence, characteristics and risk factors for household and neighbourhood injury among young children in semiurban Ghana: a population-based household survey. Inj Prev. 2015;21(e1):e71–9. doi: 10.1136/injuryprev-2013-040950.
51.
Padalko A, Cristall N, Gawaziuk JP, et al. Social Complexity and Risk for Pediatric Burn Injury: A Systematic Review. Journal of Burn Care & Research. 2019;40(4): 478–499. https://doi.org/10.1093/jbcr/i....
52.
Patel DD, Rosenberg M, Rosenberg L, et al. Poverty, population density, and the epidemiology of burns in young children from Mexico treated at a U.S. pediatric burn facility. Burns. 2018; 44(5): 1269–1278. https://doi.org/10.1016/j.burn....
53.
Kamal NN. Home Unintentional Non-fatal Injury Among Children Under 5 Years of Age in a Rural Area, El Minia Governorate, Egypt. J Community Health. 2013;38:873–879. doi: 10.1007/s10900-013-9692-y.
54.
Istre GR, McCoy M, Carlin DK, et al. Residential fire related deaths and injuries among children: fireplay, smoke alarms, and prevention. Inj Prev. 2002;8(2): 128–32. doi: 10.1136/ip.8.2.128.
55.
Lal ST, Bhatti DJ. Burn injury in infants and toddlers: risk factors, circumstances, and prevention. Indian Journal of Burns. 2017;25(1):72. doi: 10.4103/ijb.ijb_14_17.
56.
Główny Urząd Statystyczny: Dochody i warunki życia ludności Polski (raport z badania EU-SILC 2014). Warszawa: Zakład Wydawnictw Statystycznych; 2015.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.