Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
Editor's Choice
REVIEW PAPER
Role of vitamin D3 in selected pulmonary diseases with particular emphasis on lung fibrosis
1
Department of Medical Biology, Institute of Rural Health, Lublin, Poland
Corresponding author
Marta Kinga Lemieszek
Department of Medical Biology, Institute of Rural Health, Jaczewskiego 2, 20-090, Lublin, Poland
Department of Medical Biology, Institute of Rural Health, Jaczewskiego 2, 20-090, Lublin, Poland
Ann Agric Environ Med. 2023;30(1):31-44
KEYWORDS
calcidiolcalcitriolasthmacystic fibrosischronic obstructive pulmonary diseaseidiopathic pulmonary fibrosissarcoidosisCOVID-19hypersensitivity pneumonitis
TOPICS
ABSTRACT
Introduction and objective:
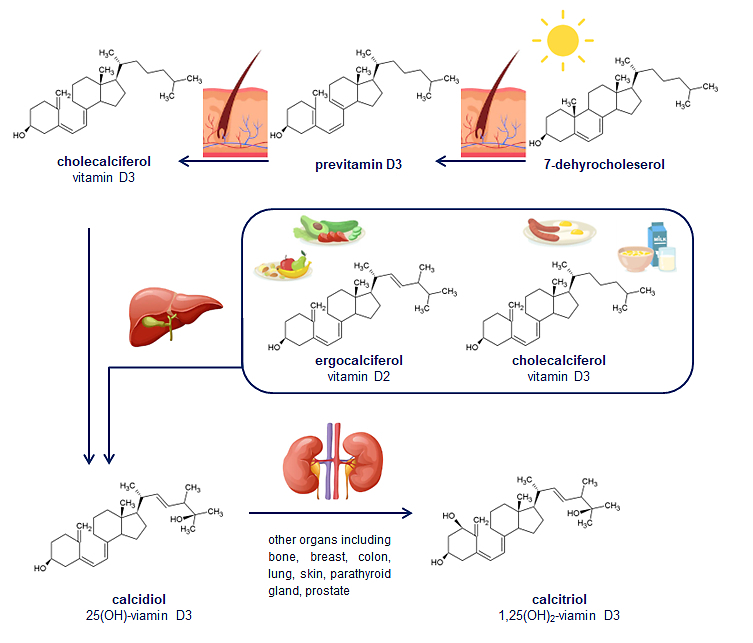
For many years vitamin D3 was known only as a regulator of the calcium-phosphate and water-electrolyte balances. Recent studies have paid special attention to other biological effects of calcitriol (the bioactive form of vitamin D3) with particular emphasis on its influence on immune function. Thus, any alterations, especially deficiencies, in the physiological level of calcitriol have serious health consequences. The aim of the study was to summarise the current state of knowledge concerning the role of vitamin D3 in selected pulmonary diseases.
Review methods:
The review was based on data obtained from articles published in PubMed between 2000–2022. Papers were reviewed for scientific merit and relevance.
Brief description of the state of knowledge:
In the reviewed literature, much attention was paid to clinical studies focused on the role of vitamin D3 in the pathogenesis of selected respiratory diseases. As revealed in research over the last two decades, vitamin D3 deficiency increases the risk and worsens the course of asthma, cystic fibrosis, chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis, as well as COVID-19. Surprisingly, vitamin D supplementation has not always proved to be an effective therapeutic strategy. The review also presents the unique concept of the possibility of using vitamin D3 in the prevention and treatment of pulmonary fibrosis in the course of hypersensitivity pneumonitis.
Summary:
Due to the multiplicity and variety of factors that affect the metabolism of vitamin D3, effective counteracting, and even more eliminating the negative consequences of disorders in the level and activity of calcitriol in the respiratory tract, seems to be a breakneck action. On the other hand, only a deep understanding of the role of calcitriol in the pathogenesis of lung diseases provides the chance to develop an effective therapy.
For many years vitamin D3 was known only as a regulator of the calcium-phosphate and water-electrolyte balances. Recent studies have paid special attention to other biological effects of calcitriol (the bioactive form of vitamin D3) with particular emphasis on its influence on immune function. Thus, any alterations, especially deficiencies, in the physiological level of calcitriol have serious health consequences. The aim of the study was to summarise the current state of knowledge concerning the role of vitamin D3 in selected pulmonary diseases.
Review methods:
The review was based on data obtained from articles published in PubMed between 2000–2022. Papers were reviewed for scientific merit and relevance.
Brief description of the state of knowledge:
In the reviewed literature, much attention was paid to clinical studies focused on the role of vitamin D3 in the pathogenesis of selected respiratory diseases. As revealed in research over the last two decades, vitamin D3 deficiency increases the risk and worsens the course of asthma, cystic fibrosis, chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis, as well as COVID-19. Surprisingly, vitamin D supplementation has not always proved to be an effective therapeutic strategy. The review also presents the unique concept of the possibility of using vitamin D3 in the prevention and treatment of pulmonary fibrosis in the course of hypersensitivity pneumonitis.
Summary:
Due to the multiplicity and variety of factors that affect the metabolism of vitamin D3, effective counteracting, and even more eliminating the negative consequences of disorders in the level and activity of calcitriol in the respiratory tract, seems to be a breakneck action. On the other hand, only a deep understanding of the role of calcitriol in the pathogenesis of lung diseases provides the chance to develop an effective therapy.
ACKNOWLEDGEMENTS
The research was supported by a grant from the National
Science Centre, Poland [Grant No, UMO-2020/38/E/
NZ7/00366, 2021].
REFERENCES (143)
1.
Tripkovic L, Lambert H, Hart K, et al. Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: a systematic review and meta-analysis. Am J Clin Nutr. 2012;95(6):1357–1364. https://doi.org/10.3945/ajcn.1....
2.
Machado Cda S, Venancio VP, Aissa AF, et al. Vitamin D3 deficiency increases DNA damage and the oxidative burst of neutrophils in a hypertensive rat model. Mutat Res Genet Toxicol Environ Mutagen. 2016;798–799:19–26. https://doi.org/10.1016/j.mrge....
3.
Christakos S, Dhawan P, Verstuyf A, et al. Vitamin D: metabolism, molecular mechanism of action, and pleiotropic effects. Physiol Rev. 2016;96(1):365–408. https://doi.org/10.1152/physre....
4.
Sassi F, Tamone C, D’Amelio P. Vitamin D: nutrient, hormone, nd immunomodulator. Nutrients. 2018;10(11):1656. https://doi.org/10.3390/nu1011....
5.
Adams JS, Hewison M. Extrarenal expression of the 25-hydroxyvitamin D-1-hydroxylase. Arch Biochem Biophys. 2012;523(1):95–102. https://doi.org/10.1016/j.abb.....
6.
Borel P, Caillaud D, Cano NJ. Vitamin D bioavailability: state of the art. Crit Rev Food Sci Nutr. 2015;55(9):1193–205. https://doi.org/10.1080/104083....
7.
Holick MF. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. 2017;18(2):153–165. https://doi.org/10.1007/s11154....
8.
Rusińska A, Płudowski P, Walczak M, et al. Vitamin D supplementation guidelines for general population and groups at risk of vitamin D deficiency in Poland-recommendations of the Polish Society of Pediatric Endocrinology and Diabetes and the expert panel with participation of national specialist consultants and representatives of scientific societies-2018 update. Front Endocrinol (Lausanne). 2018;9:246. https://doi.org/10.3389/fendo.....
9.
Sutton AL, MacDonald PN. Vitamin D: more than a “bone-a-fide” hormone. Mol Endocrinol. 2003;17(5):777–791. https://doi.org/10.1210/me.200....
10.
Pike JW, Meyer MB, Lee SM, et al. The vitamin D receptor: contemporary genomic approaches reveal new basic and translational insights. J Clin Invest. 2017;127(4):1146–1154. https://doi.org/10.1172/jci888....
11.
Zmijewski MA, Carlberg C. Vitamin D receptor(s): In the nucleus but also at membranes? Exp Dermatol. 2020;29(9):876–884. https://doi.org/10.1111/exd.14....
12.
Barry EL, Rees JR, Peacock JL, et al. Genetic variants in CYP2R1, CYP24A1, and VDR modify the efficacy of vitamin D3 supplementation for increasing serum 25-hydroxyvitamin D levels in a randomized controlled trial. J Clin Endocrinol Metab. 2014;99(10):E2133–137. https://doi.org/10.1210/jc.201....
13.
Bahrami A, Sadeghnia HR, Tabatabaeizadeh SA, et al. Genetic and epigenetic factors influencing vitamin D status. J Cell Physiol. 2018;233(5):4033–4043. https://doi.org/10.1002/jcp.26....
14.
Rozmus D, Płomiński J, Augustyn K, et al. rs7041 and rs4588 Poly-morphisms in Vitamin D Binding Protein Gene (VDBP) and the Risk of Diseases. Int J Mol Sci. 2022;23(2):933. https://doi.org/10.3390/ijms23....
15.
Al-Daghri NM, Mohammed AK, Bukhari I, et al. Efficacy of vitamin D supplementation according to vitamin D-binding protein polymorphisms. Nutrition. 2019;63–64:148–154. https://doi.org/10.1016/j.nut.....
16.
Di Rosa M, Malaguarnera M, Nicoletti F, Malaguarnera L. Vitamin D3: a helpful immuno-modulator. Immunology. 2011 Oct;134(2):123–39. https://doi.org/10.1111/j.1365....
17.
Wei R, Christakos S. Mechanisms Underlying the Regulation of Innate and Adaptive Immunity by Vitamin D. Nutrients. 2015;7(10):8251–8260. https://doi.org/10.3390/nu7105....
18.
Ahmad S, Arora S, Khan S, et al. Vitamin D and its therapeutic relevance in pulmonary diseases. J Nutr Biochem. 2021;90:108571. https://doi.org/10.1016/j.jnut....
19.
Chun RF, Liu PT, Modlin RL, et al. Impact of vitamin D on immune function: lessons learned from genome-wide analysis. Front Physiol. 2014;5:151. https://doi.org/10.3389/fphys.....
20.
Small AG, Harvey S, Kaur J, et al. Vitamin D upregulates the macrophage complement receptor immunoglobulin in innate immunity to microbial pathogens. Commun Biol. 2021;4(1):401. https://doi.org/10.1038/s42003....
21.
Anand SP, Selvaraj P. Effect of 1, 25 dihydroxyvitamin D(3) on matrix metalloproteinases MMP-7, MMP-9 and the inhibitor TIMP-1 in pulmonary tuberculosis. Clin Immunol. 2009;133(1):126–131. https://doi.org/10.1016/j.clim....
22.
Sadeghi K, Wessner B, Laggner U, et al. Vitamin D3 down-regulates monocyte TLR expression and triggers hyporesponsiveness to pathogen-associated molecular patterns. Eur J Immunol. 2006;36(2):361–370. https://doi.org/10.1002/eji.20....
23.
Almerighi C, Sinistro A, Cavazza A, et al. 1Alpha,25-dihydroxy-vitamin D3 inhibits CD40L-induced pro-inflammatory and immuno -modulatory activity in human monocytes. Cytokine. 2009;45(3):190–197. https://doi.org/10.1016/j.cyto....
24.
Adorini L, Penna G, Giarratana N, et al. Dendritic cells as key targets for immunomodulation by Vitamin D receptor ligands. J Steroid Biochem Mol Biol. 2004;89–90(1–5):437–441. https://doi.org/10.1016/j.jsbm....
25.
Piemonti L, Monti P, Sironi M, et al. Vitamin D3 affects differentiation, maturation, and function of human monocyte-derived dendritic cells. J Immunol. 2000;164(9):4443–4451. https://doi.org/10.4049/jimmun....
26.
Penna G, Amuchastegui S, Giarratana N, et al. 1,25-Dihydroxyvitamin D3 selectively modulates tolerogenic properties in myeloid but not plasmacytoid dendritic cells. J Immunol. 2007;178(1):145–153. https://doi.org/10.4049/jimmun....
27.
Sassi F, Tamone C, D’Amelio P. Vitamin D: nutrient, hormone, and immuno modulator. Nutrients. 2018;10(11):1656. https://doi.org/10.3390/nu1011....
28.
Daniel C, Sartory NA, Zahn N, et al. Immune modulatory treatment of trinitrobenzene sulfonic acid colitis with calcitriol is associated with a change of a T helper (Th) 1/Th17 to a Th2 and regulatory T cell profile. J Pharmacol Exp Ther. 2008;324(1):23–33. https://doi.org/10.1124/jpet.1....
29.
Mora JR, Iwata M, von Andrian UH. Vitamin effects on the immune system: vitamins A and D take centre stage. Nat Rev Immunol. 2008;8(9):685–698. https://doi.org/10.1038/nri237....
30.
Baeke F, Korf H, Overbergh L, et al. Human T lymphocytes are direct targets of 1,25-dihydroxyvitamin D3 in the immune system. J Steroid Biochem Mol Biol. 2010;121(1–2):221–227. https://doi.org/10.1016/j.jsbm....
31.
Chen S, Sims GP, Chen XX, et al. Modulatory effects of 1,25-dihydroxyvitamin D3 on human B cell differentiation. J Immunol. 2007;179(3):1634–1647. https://doi.org/10.4049/jimmun....
32.
Wang TT, Nestel FP, Bourdeau V, et al. Cutting edge: 1,25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression. J Immunol. 2004;173(5):2909–2912. https://doi.org/10.4049/jimmun....
33.
Liu PT, Stenger S, Li H, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;311(5768):1770–1773. https://doi.org/10.1126/scienc....
34.
Chakraborty K, Ghosh S, Koley H, et al. Bacterial exotoxins downregulate cathelicidin (hCAP-18/LL-37) and human beta-defensin 1 (HBD-1) expression in the intestinal epithelial cells. Cell Microbiol. 2008;10(12):2520–2537. https://doi.org/10.1111/j.1462....
35.
Hewison M. An update on vitamin D and human immunity. Clin Endocrinol (Oxf). 2012;76(3):315–325. https://doi.org/10.1111/j.1365....
36.
Ganz T. Defensins: antimicrobial peptides of vertebrates. C R Biol. 2004;327(6):539–549. https://doi.org/10.1016/j.crvi....
37.
Kościuczuk EM, Lisowski P, Jarczak J, et al. Cathelicidins: family of antimicrobial peptides. A review. Mol Biol Rep. 2012;39(12):10957–10970. doi: 10.1007/s11033-012-1997-x. Epub 2012 Oct 14. https://doi.org/10.1007/s11033....
38.
van Harten RM, van Woudenbergh E, van Dijk A, et al. Cathelicidins: immunomodulatory antimicrobials. Vaccines (Basel). 2018;6(3):63. https://doi.org/10.3390/vaccin....
39.
Gombart AF. The vitamin D-antimicrobial peptide pathway and its role in protection against infection. Future Microbiol. 2009;4(9):1151–1165. https://doi.org/10.2217/fmb.09....
40.
Steinstraesser L, Koehler T, Jacobsen F, et al. Host defense peptides in wound healing. Mol Med. 2008;14(7–8):528–37. https://doi.org/10.2119/2008-0....
41.
Hansdottir S, Monick MM, Hinde SL, et al. Respiratory epithelial cells convert inactive vitamin D to its active form: potential effects on host defense. J Immunol. 2008;181(10):7090–7099. https://doi.org/10.4049/jimmun....
42.
Quirt J, Hildebrand KJ, Mazza J, et al. Asthma. Allergy Asthma Clin Immunol. 2018;14(Suppl 2):50. https://doi.org/10.1186/s13223....
43.
Zhao DD, Yu DD, Ren QQ, et al. Association of vitamin D receptor gene polymorphisms with susceptibility to childhood asthma: A meta-analysis. Pediatr Pulmonol. 2017;52(4):423–429. https://doi.org/10.1002/ppul.2....
44.
Nasiri-Kalmarzi R, Abdi M, Hosseini J, et al. Association of vitamin D genetic pathway with asthma susceptibility in the Kurdish population. J Clin Lab Anal. 2020;34(1):e23039. https://doi.org/10.1002/jcla.2....
45.
Fawzy MS, Elgazzaz MG, Ibrahim A, et al. Association of group-specific component exon 11 polymorphisms with bronchial asthma in children and adolescents. Scand J Immunol. 2019;89(3):e12740. https://doi.org/10.1111/sji.12....
46.
Paraskakis E Iordanidou M Tavridou A, et al. Vitamin D receptor and vitamin D binding protein polymorphisms are associated with asthma control in children. Eur Respir J 2012;40(Suppl.56)4569. https://www.ers-education.org/....
47.
Randolph AG, Yip WK, Falkenstein-Hagander K, et al. Vitamin D-binding protein haplotype is associated with hospitalization for RSV bronchiolitis. Clin Exp Allergy. 2014;44(2):231–237. https://doi.org/10.1111/cea.12....
48.
Brehm JM, Acosta-Pérez E, Klei L, et al. Vitamin D insufficiency and severe asthma exacerbations in Puerto Rican children. Am J Respir Crit Care Med. 2012;186(2):140–146. https://doi.org/10.1164/rccm.2....
49.
Chinellato I, Piazza M, Sandri M, et al. Vitamin D serum levels and markers of asthma control in Italian children. J Pediatr. 2011;158(3):437–441. https://doi.org/10.1016/j.jped....
50.
Beyhan-Sagmen S, Baykan O, Balcan B, et al. Association Between Severe Vitamin D Deficiency, Lung Function and Asthma Control. Arch Bronconeumol. 2017;53(4):186–191. English, Spanish. https://doi.org/10.1016/j.arbr....
51.
Korn S, Hübner M, Jung M, Blettner M, Buhl R. Severe and uncontrolled adult asthma is associated with vitamin D insufficiency and deficiency. Respir Res. 2013;14(1):25. https://doi.org/10.1186/1465-9....
52.
Tachimoto H, Mezawa H, Segawa T, et al. Improved control of childhood asthma with low-dose, short-term vitamin D supplementation: a randomized, double-blind, placebo-controlled trial. Allergy. 2016;71(7):1001–9. https://doi.org/10.1111/all.12....
53.
Zosky GR, Hart PH, Whitehouse AJ, et al. Vitamin D deficiency at 16 to 20 weeks’ gestation is associated with impaired lung function and asthma at 6 years of age. Ann Am Thorac Soc. 2014;11(4):571–577. https://doi.org/10.1513/annals....
54.
Denlinger LC, King TS, Cardet JC, et al. Vitamin D supplementation and the risk of colds in patients with asthma. Am J Respir Crit Care Med. 2016;193(6):634–641. https://doi.org/10.1164/rccm.2....
55.
Shteinberg M, Haq IJ, Polineni D, et al. Cystic fibrosis. Lancet. 2021; 397(10290):2195–2211. https://doi.org/10.1016/s0140-....
56.
Elkin SL, Fairney A, Burnett S, et al. Vertebral deformities and low bone mineral density in adults with cystic fibrosis: a cross-sectional study. Osteoporos Int. 2001;12(5):366–372. https://doi.org/10.1007/s00198....
57.
Grey V, Atkinson S, Drury D, et al. Prevalence of low bone mass and deficiencies of vitamins D and K in pediatric patients with cystic fibrosis from 3 Canadian centers. Pediatrics. 2008;122(5):1014–1020. https://doi.org/10.1542/peds.2....
58.
Neville LA, Ranganathan SC. Vitamin D in infants with cystic fibrosis diagnosed by newborn screening. J Paediatr Child Health. 2009;45(1–2):36–41. https://doi.org/10.1111/j.1440....
59.
Daley T, Hughan K, Rayas M, et al. Vitamin D deficiency and its treatment in cystic fibrosis. J Cyst Fibros. 2019;18(Suppl.2):S66-S73. https://doi.org/10.1016/j.jcf.....
60.
Walkowiak J, Lisowska A, Blaszczyński M. The changing face of the exocrine pancreas in cystic fibrosis: pancreatic sufficiency, pancreatitis and genotype. Eur J Gastroenterol Hepatol. 2008;20(3):157–160. https://doi.org/10.1097/meg.0b....
61.
Boyle MP, Noschese ML, Watts SL, et al. Failure of high-dose ergocalciferol to correct vitamin D deficiency in adults with cystic fibrosis. Am J Respir Crit Care Med. 2005;172(2):212–217. https://doi.org/10.1164/rccm.2....
62.
Green D, Carson K, Leonard A, et al. Current treatment recommendations for correcting vitamin D deficiency in pediatric patients with cystic fibrosis are inadequate. J Pediatr. 2008;153(4):554–559. https://doi.org/10.1016/j.jped....
63.
Rovner AJ, Stallings VA, Schall JI, et al. Vitamin D insufficiency in children, adolescents, and young adults with cystic fibrosis despite routine oral supplementation. Am J Clin Nutr. 2007;86(6):1694–1699. https://doi.org/10.1093/ajcn/8....
64.
Gronowitz E, Larkö O, Gilljam M, et al. Ultraviolet B radiation improves serum levels of vitamin D in patients with cystic fibrosis. Acta Paediatr. 2005;94(5):547–552. https://doi.org/10.1111/j.1651....
65.
Khazai NB, Judd SE, Jeng L, et al. Treatment and prevention of vitamin D insufficiency in cystic fibrosis patients: comparative efficacy of ergocalciferol, cholecalciferol, and UV light. J Clin Endocrinol Metab. 2009;94(6):2037–2043. https://doi.org/10.1210/jc.200....
66.
Grossmann RE, Zughaier SM, Liu S, et al. Impact of vitamin D supplementation on markers of inflammation in adults with cystic fibrosis hospitalized for a pulmonary exacerbation. Eur J Clin Nutr. 2012;66(9):1072–1074. https://doi.org/10.1038/ejcn.2....
67.
McCauley LA, Thomas W, Laguna TA, et al. Vitamin D deficiency is associated with pulmonary exacerbations in children with cystic fibrosis. Ann Am Thorac Soc. 2014;11(2):198–204. https://doi.org/10.1513/annals....
68.
Olszowiec-Chlebna M, Koniarek-Maniecka A, Brzozowska A, Błauż A, Rychlik B, Stelmach I. Vitamin D inhibits pro-inflammatory cytokines in the airways of cystic fibrosis patients infected by Pseudomonas aeruginosa- pilot study. Ital J Pediatr. 2019;45(1):41. https://doi.org/10.1186/s13052....
69.
Barnes PJ. Cellular and molecular mechanisms of chronic obstructive pulmonary disease. Clin Chest Med. 2014;35(1):71–86. https://doi.org/10.1016/j.ccm.....
70.
Dawson-Hughes B, Heaney RP, Holick MF, et al. Estimates of optimal vitamin D status. Osteoporos Int. 2005;16(7):713–716. https://doi.org/10.1007/s00198....
71.
Janssens W, Lehouck A, Carremans C, et al. Vitamin D beyond bones in chronic obstructive pulmonary disease: time to act. Am J Respir Crit Care Med. 2009;179(8):630–636. https://doi.org/10.1164/rccm.2....
72.
Malinovschi A, Masoero M, Bellocchia M, et al. Severe vitamin D deficiency is associated with frequent exacerbations and hospitalization in COPD patients. Respir Res. 2014;15(1):131. https://doi.org/10.1186/s12931....
73.
Forli L, Halse J, Haug E, et al. Vitamin D deficiency, bone mineral density and weight in patients with advanced pulmonary disease. J Intern Med. 2004;256(1):56–62. https://doi.org/10.1111/j.1365....
74.
Janssens W, Bouillon R, Claes B, et al. Vitamin D deficiency is highly prevalent in COPD and correlates with variants in the vitamin D-binding gene. Thorax. 2010;65(3):215–220. https://doi.org/10.1136/thx.20....
75.
Persson LJ, Aanerud M, Hiemstra PS, et al. Chronic obstructive pulmonary disease is associated with low levels of vitamin D. PLoS One. 2012;7(6):e38934. https://doi.org/10.1371/journa....
76.
Fu L, Fei J, Tan ZX, et al. Low vitamin D status is associated with inflammation in patients with chronic obstructive pulmonary disease. J Immunol. 2021;206(3):515–523. https://doi.org/10.4049/jimmun....
77.
Sluyter JD, Camargo CA, Waayer D, et al. Effect of monthly, high-dose, long-term vitamin D on lung function: a randomized controlled trial. Nutrients. 2017;9(12):1353. https://doi.org/10.3390/nu9121....
78.
Alavi Foumani A, Mehrdad M, Jafarinezhad A, et al. Impact of vitamin D on spirometry findings and quality of life in patients with chronic obstructive pulmonary disease: a randomized, double-blinded, placebo-controlled clinical trial. Int J Chron Obstruct Pulmon Dis. 2019;14:1495–1501. https://doi.org/10.2147/copd.s....
79.
Zendedel A, Gholami M, Anbari K, et al. Effects of vitamin D intake on FEV1 and COPD exacerbation: a randomized clinical trial study. Glob J Health Sci. 2015;7(4):243–248. https://doi.org/10.5539/gjhs.v....
80.
Lehouck A, Mathieu C, Carremans C, et al. High doses of vitamin D to reduce exacerbations in chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med. 2012;156(2):105–114. https://doi.org/10.7326/0003-4....
81.
Martineau AR, James WY, Hooper RL, et al. Vitamin D3 supplemen-tation in patients with chronic obstructive pulmonary disease (ViDiCO): a multicentre, double-blind, randomised controlled trial. Lancet Respir Med. 2015;3(2):120–130. https://doi.org/10.1016/s2213-....
82.
Rafiq R, Prins HJ, Boersma WG, et al. Effects of daily vitamin D supplementation on respiratory muscle strength and physical performance in vitamin D-deficient COPD patients: a pilot trial. Int J Chron Obstruct Pulmon Dis. 2017;12:2583–2592. https://doi.org/10.2147/copd.s....
83.
Li X, Liu X, Xu Y, et al. The correlation of vitamin D level and vitamin D-binding protein gene polymorphism in chronic obstructive pulmonary disease. Zhonghua Nei Ke Za Zhi. 2014;53(4):303–307.
84.
Horita N, Miyazawa N, Tomaru K, et al. Vitamin D binding protein genotype variants and risk of chronic obstructive pulmonary disease: a meta-analysis. Respirology. 2015;20(2):219–225. https://doi.org/10.1111/resp.1....
85.
Khanna R, Nandy D, Senapati S. Systematic review and meta-analysis to establish the association of common genetic variations in vitamin D binding protein with chronic obstructive pulmonary disease. Front Genet. 2019;10:413. https://doi.org/10.3389/fgene.....
86.
Ishii T, Motegi T, Kamio K, et al. Association of group component genetic variations in COPD and COPD exacerbation in a Japanese population. Respirology. 2014;19(4):590–595. https://doi.org/10.1111/resp.1....
87.
Liu YM, Nepali K, Liou JP. Idiopathic pulmonary fibrosis: current status, recent progress, and emerging targets. J Med Chem. 2017;60(2):527–553. https://doi.org/10.1021/acs.jm....
88.
Ziesche R, Golec M, Samaha E. The RESOLVE concept: approaching patho physiology of fibroproliferative disease in aged individuals. Biogerontology. 2013;14(6):679–685. https://doi.org/10.1007/s10522....
89.
Aryal S, Nathan SD. An update on emerging drugs for the treatment of idiopathic pulmonary fibrosis. Expert Opin Emerg Drugs. 2018;23(2):159–172. https://doi.org/10.1080/147282....
90.
Abuserewa ST, Duff R, Becker G. Treatment of idiopathic pulmonary fibrosis. Cureus. 2021;13(5):e15360. https://doi.org/10.7759/cureus....
91.
Ma D, Peng L. Vitamin D and pulmonary fibrosis: a review of molecular mechanisms. Int J Clin Exp Pathol. 2019;12(9):3171–3178.
92.
Kasthuri RS, Glover SL, Boles J, et al. Tissue factor and tissue factor pathway inhibitor as key regulators of global hemostasis: measurement of their levels in coagulation assays. Semin Thromb Hemost. 2010;36(7):764–771. https://doi.org/10.1055/s-0030....
93.
Finklea JD, Grossmann RE, Tangpricha V. Vitamin D and chronic lung disease: a review of molecular mechanisms and clinical studies. Adv Nutr. 2011;2(3):244–253. https://doi.org/10.3945/an.111....
94.
Fischer KD, Agrawal DK. Vitamin D regulating TGF-ß induced epithelial-mesenchymal transition. Respir Res. 2014;15(1):146. https://doi.org/10.1186/s12931....
95.
Jiang F, Yang Y, Xue L, et al. 1?,25-dihydroxyvitamin D3 attenuates TGF-ß-induced pro-fibrotic effects in human lung epithelial cells through inhibition of epithelial-mesenchymal transition. Nutrients. 2017;9(9):980. https://doi.org/10.3390/nu9090....
96.
Faverio P, Fumagalli A, Conti S, et al. Nutritional assessment in idiopathic pulmonary fibrosis: a prospective multicentre study. ERJ Open Res. 2022;8(1):00443–2021. https://doi.org/10.1183/231205....
97.
Tzilas V, Bouros E, Barbayianni I, et al. Vitamin D prevents experimental lung fibrosis and predicts survival in patients with idiopathic pulmonary fibrosis. Pulm Pharmacol Ther. 2019;55:17–24. https://doi.org/10.1016/j.pupt....
98.
Yang L, Zhai Z, Zhang J. The role of serum 1,25-dihydroxy vitamin D3 and PCT in idiopathic pulmonary fibrosis. Int J Gen Med. 2022;15:8081–8092. https://doi.org/10.2147/ijgm.s....
99.
Yavari M, Mousavi SAJ, Janani L, et al. Effects of supplementation of vitamins D, C and E on idiopathic pulmonary fibrosis (IPF): a clinical trial. Clin Nutr ESPEN. 2022;49:295–300. https://doi.org/10.1016/j.clne....
100.
Sharma A, Ahmad Farouk I, Lal SK. COVID-19: a review on the novel coronavirus disease evolution, transmission, detection, control and prevention. Viruses. 2021;13(2):202. https://doi.org/10.3390/v13020....
101.
Lumbers ER, Head R, Smith GR, et al. The interacting physiology of COVID-19 and the renin-angiotensin-aldosterone system: Key agents for treatment. Pharmacol Res Perspect. 2022;10(1):e00917. https://doi.org/10.1002/prp2.9....
102.
Kaufman HW, Niles JK, Kroll MH, et al. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS One. 2020;15(9):e0239252. https://doi.org/10.1371/journa....
103.
Merzon E, Tworowski D, Gorohovski A, et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J. 2020;287(17):3693–3702. https://doi.org/10.1111/febs.1....
104.
D’Avolio A, Avataneo V, Manca A, et al. 25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2. Nutrients. 2020;12(5):1359. https://doi.org/10.3390/nu1205....
105.
Abdollahi A, Kamali Sarvestani H, Rafat Z, et al. The association between the level of serum 25(OH) vitamin D, obesity, and underlying diseases with the risk of developing COVID-19 infection: A case-control study of hospitalized patients in Tehran, Iran. J Med Virol. 2021;93(4):2359–2364. https://doi.org/10.1002/jmv.26....
106.
Nogues X, Ovejero D, Pineda-Moncusí M, et al. Calcifediol Treatment and COVID-19-Related Outcomes. J Clin Endocrinol Metab. 2021;106(10):e4017-e4027. https://doi.org/10.1210/clinem....
107.
Murai IH, Fernandes AL, Sales LP, et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial. JAMA. 2021;325(11):1053–1060. https://doi.org/10.1001/jama.2....
108.
Mariani J, Antonietti L, Tajer C, et al. High-dose vitamin D versus placebo to prevent complications in COVID-19 patients: multicentre randomized controlled clinical trial. PLoS One. 2022;17(5):e0267918. https://doi.org/10.1371/journa....
109.
Bassatne A, Basbous M, Chakhtoura M, et al. The link between COVID-19 and VItamin D (VIVID): a systematic review and meta-analysis. Metabolism. 2021;119:154753. https://doi.org/10.1016/j.meta....
110.
Llanos O, Hamzeh N. Sarcoidosis. Med Clin North Am. 2019;103(3):527–534. https://doi.org/10.1016/j.mcna....
111.
Kaiser Y, Eklund A, Grunewald J. Moving target: shifting the focus to pulmonary sarcoidosis as an autoimmune spectrum disorder. Eur Respir J. 2019;54(1):1802153. https://doi.org/10.1183/139930....
112.
Jain R, Yadav D, Puranik N, et al. Sarcoidosis: causes, diagnosis, clinical features, and treatments. J Clin Med. 2020;9(4):1081. https://doi.org/10.3390%2Fjcm9....
113.
Starshinova AA, Malkova AM, Basantsova NY, et al. Sarcoidosis as an Autoimmune Disease. Front Immunol. 2020;10:2933. https://doi.org/10.3389%2Ffimm....
114.
Targowski T. Differences in the metabolism of vitamin D in sarcoidosis. Post N Med. 2016; XXIX(10):750–752.
115.
Locke LW, Schlesinger LS, Crouser ED. Current sarcoidosis models and the importance of focusing on the granuloma. Front Immunol. 2020;11:1719. https://doi.org/10.3389/fimmu.....
116.
Baughman RP, Janovcik J, Ray M, et al. Calcium and vitamin D metabolism in sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2013;30(2):113–120.
117.
Saidenberg-Kermanac’h N, Semerano L, Nunes H, et al. Bone fragility in sarcoidosis and relationships with calcium metabolism disorders: a cross sectional study on 142 patients. Arthritis Res Ther. 2014;16(2):R78. https://doi.org/10.1186%2Far45....
118.
Kavathia D, Buckley JD, Rao D, et al. Elevated 1, 25-dihydroxyvitamin D levels are associated with protracted treatment in sarcoidosis. Respir Med. 2010;104(4):564–570. https://doi.org/10.1016%2Fj.rm....
119.
Kamphuis LS, Bonte-Mineur F, van Laar JA, et al. Calcium and vitamin D in sarcoidosis: is supplementation safe? J Bone Miner Res. 2014;29(11):2498–2503. https://doi.org/10.1002/jbmr.2....
120.
Newman LS, Rose CS, Maier LA: Sarcoidosis. N Engl J Med. 1997;336:1224–1235. https://doi.org/10.1056/nejm19....
121.
Wilsher ML. Seasonal clustering of sarcoidosis presenting with erythema nodosum. Eur Respir J. 1998;12:1197–1199. https://doi.org/10.1183/090319....
122.
Demirkok SS, Basaranoglu M, Akinci ED, et al. Analysis of 275 patients with sarcoidosis over a 38 year period; a single-institution experience. Respir Med. 2007;101:1147–1154. https://doi.org/10.1016/j.rmed....
123.
Swigris JJ, Olson AL, Huie TJ, et al. Sarcoidosis-related mortality in the United States from 1988 to 2007. Am J Respir Crit Care Med. 2011;183(11):1524–1530.
124.
Gerke AK, Yang M, Tang F, et al. Increased hospitalizations among sarcoidosis patients from 1998 to 2008: a population-based cohort study. BMC Pulm Med. 2012;12:19. https://doi.org/10.1186/1471-2....
125.
Mirsaeidi M, Machado RF, Schraufnagel D, et al. Racial difference in sarcoidosis mortality in the United States. Chest. 2015;147(2):438–449. https://doi.org/10.1378%2Fches....
126.
Capolongo G, Xu LH, Accardo M, et al. Vitamin-D status and mineral metabolism in two ethnic populations with sarcoidosis. J Investig Med. 2016;64(5):1025–1034. https://doi.org/10.1136/jim-20....
127.
Bolland MJ, Wilsher ML, Grey A, et al. Randomised controlled trial of vitamin D supplementation in sarcoidosis. BMJ Open. 2013;3(10):e003562. https://doi.org/10.1136/bmjope....
128.
Spagnolo P, Rossi G, Cavazza A, et al. Hypersensitivity pneumonitis: a comprehensive review. J Investig Allergol Clin Immunol. 2015;25(4):237–250.
129.
Nogueira R, Melo N, Novais E, et al. Hypersensitivity pneumonitis: Antigen diversity and disease implications. Pulmonology. 2019;25(2):97–108. https://doi.org/10.1016/j.pulm....
130.
Rittig AH, Hilberg O, Ibsen R, et al. Incidence, comorbidity and survival rate of hypersensitivity pneumonitis: a national population-based study. ERJ Open Res. 2019;5(4):00259–2018. https://doi.org/10.1183/231205....
131.
Churg A, Sin DD, Everett D, et al. Pathologic patterns and survival in chronic hypersensitivity pneumonitis. Am J Surg Pathol. 2009;33(12):1765–1770. https://doi.org/10.1097/pas.0b....
132.
Lima MS, Coletta EN, Ferreira RG, et al. Subacute and chronic hypersensitivity pneumonitis: histopathological patterns and survival. Respir Med. 2009;103(4):508–515. https://doi.org/10.1016/j.rmed....
133.
Lemieszek MK, Rzeski W, Golec M, et al. Pantoea agglomerans chronic exposure induces epithelial-mesenchymal transition in human lung epithelial cells and mice lungs. Ecotoxicol Environ Saf. 2020;194:110416. https://doi.org/10.1016/j.ecoe....
134.
Lemieszek MK, Sawa-Wejksza K, Golec M, et al. Beneficial impact of cathelicidin on hypersensitivity pneumonitis treatment-In vivo studies. PLoS One. 2021;16(5):e0251237. https://doi.org/10.1371/journa....
135.
Golec M, Reichel C, Mackiewicz B, et al. Cathelicidin LL-37, granzymes, TGF-beta1 and cytokines levels in induced sputum from farmers with and without COPD. Ann Agric Environ Med. 2009;16(2):289–297.
136.
Golec M, Reichel C, Lemieszek M, et al. Cathelicidin LL-37 in bronchoalveolar lavage and epithelial lining fluids from COPD patients and healthy individuals. J Biol Regul Homeost Agents. 2012;26(4):617–625.
137.
Lemieszek M, Golec M, Reichel C, et al. Levels of antimicrobial peptide LL-37 in BALF and ELF from patients with pulmonary fibrosis. European Respiratory Journal 2013a;42(Suppl.57):P5126. https://erj.ersjournals.com/co....
138.
Willis BC, Borok Z. TGF-beta-induced EMT: mechanisms and implications for fibrotic lung disease. Am J Physiol Lung Cell Mol Physiol. 2007;293(3):L525-L534. https://doi.org/10.1152/ajplun....
139.
Tanjore H, Xu XC, Polosukhin VV, et al. Contribution of epithelial-derived fibroblasts to bleomycin-induced lung fibrosis. Am J Respir Crit Care Med. 2009;180(7):657–665. https://doi.org/10.1164/rccm.2....
140.
Larriba MJ, García de Herreros A, Munoz A. Vitamin D and the epithelial to mesenchymal transition. Stem Cells Int. 2016;2016:6213872. https://doi.org/10.1155/2016/6....
141.
Zheng S, Yang J, Hu X, et al. Vitamin D attenuates lung injury via stimulating epithelial repair, reducing epithelial cell apoptosis and inhibits TGF-ß induced epithelial to mesenchymal transition. Biochem Pharmacol. 2020;177:113955. https://doi.org/10.1016/j.bcp.....
142.
Lemieszek M, Chilosi M, Golec M, et al. Mouse model of hypersensitivity pneumonitis after inhalation exposure to different microbial antigens associated with organic dusts. Ann Agric Environ Med. 2011;18(1):159–168.
143.
Lemieszek MK, Chilosi M, Golec M, et al. Age influence on hypersensitivity pneumonitis induced in mice by exposure to Pantoea agglomerans. Inhal Toxicol. 2013b;25(11):640–650. https://doi.org/10.3109/089583....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.