Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Representatives of generation ‘Z’ as future doctors – results of research among final year students at medical universities in Poland
1
Department of Population Health, Division of Public Health, Medical University, Wrocław Poland
2
Faculty of Management, Department of Managing Production and Work, University of Economics, Wrocław, Poland
Corresponding author
Dorota Kiedik
Department of Population Health Division of Public Health Wroclaw Medical University, Bujwida 44, 50-345, Wroclaw, Poland
Department of Population Health Division of Public Health Wroclaw Medical University, Bujwida 44, 50-345, Wroclaw, Poland
Ann Agric Environ Med. 2023;30(1):177-182
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The nature of the work of doctors is inseparable from responsibility for human health and life, exposure to many risk factors related to physical, chemical, biological and psychosocial risks, as well as the specificity of the organization of the health care system in Poland. This prompted the authors to ask future doctors, currently students of the penultimate and the final year of medical studies, questions about what is important to them in their future profession and how studies at the medical universities met these needs.
Material and methods:
Identification of skills important for future doctors to perform their profession was conducted in the third quarter of 2020 in the form of an online diagnostic survey on a sample of 442 fifth- and sixth-year medicine students at medical universities in Poland.
Results:
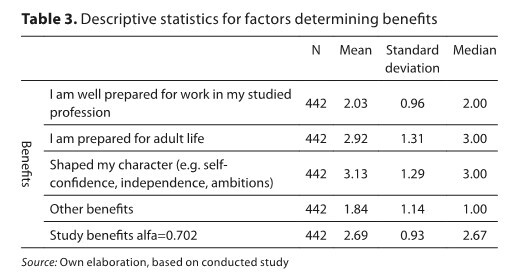
The study shows that most students graduating in medicine are satisfied with their choice and intend to work in the profession they have learned. In this study, the responders, on average, felt well prepared theoretically for their future profession, whereas when indicating their practical preparedness, it was much lower. One of the most important skills indicated by students participating in this study was communication with patients.
Conclusions:
Overall, the quality of medical studies in Poland is rated very high by the students. Nevertheless, there is a lack of or insufficient time spent on teaching and helping future doctors develop soft skills; therefore, more focus should be placed on this aspect of studies.
The nature of the work of doctors is inseparable from responsibility for human health and life, exposure to many risk factors related to physical, chemical, biological and psychosocial risks, as well as the specificity of the organization of the health care system in Poland. This prompted the authors to ask future doctors, currently students of the penultimate and the final year of medical studies, questions about what is important to them in their future profession and how studies at the medical universities met these needs.
Material and methods:
Identification of skills important for future doctors to perform their profession was conducted in the third quarter of 2020 in the form of an online diagnostic survey on a sample of 442 fifth- and sixth-year medicine students at medical universities in Poland.
Results:
The study shows that most students graduating in medicine are satisfied with their choice and intend to work in the profession they have learned. In this study, the responders, on average, felt well prepared theoretically for their future profession, whereas when indicating their practical preparedness, it was much lower. One of the most important skills indicated by students participating in this study was communication with patients.
Conclusions:
Overall, the quality of medical studies in Poland is rated very high by the students. Nevertheless, there is a lack of or insufficient time spent on teaching and helping future doctors develop soft skills; therefore, more focus should be placed on this aspect of studies.
ACKNOWLEDGEMENTS
Funding source
This research received funding from the Ministry of Science and Higher Education in Poland under the programme "Regional Initiative of Excellence" 2019 – 2022 The study was also supported by the resources of the Wroclaw Medical University within the task recorded in the SIMPLE system: SUB.Z.260.22.074
REFERENCES (17)
1.
Wójcik J. Lekarz. Zawód czy powołanie? Postawy lekarzy wobec pracy zawodowej. Oficyna Wydawnicza Wacław Walasek; 2018. ISBN 9788365694560.
2.
Moffat KJ, McConnachie A, Ross S, Morrison JM. Undergraduate medical education first year medical student stress and coping in a problem-based learning medical curriculum. Med Educ Mar. 2004;38(5):482–91.
3.
Rozporządzenie Ministra Zdrowia z dnia 16 lipca 2020 r. w sprawie limitu przyjęć na studia na kierunkach lekarskim i lekarsko-dentystycznym [Regulation of the Minister of Health, on the admission limit for studies in medicine and medicine and dentistry. Jul 2020.]https://isap.sejm.gov.pl/isap.... (4.08.2020).
4.
OECD/Unia Europejska (2020), „Practising doctors per 1000 population, 2008 and 2018 (lub najbliższy rok)”. In : Accessibility: Affordability, Availability and use of services. Paris: OECD Publishing; https://doi.org/ 10.1787/d6dd5994-pl (8.08.2021).
5.
Ustawa z dnia 5 grudnia 1996 r. o zawodach lekarza i lekarza dentysty, DzU 1997 nr 28 poz. 152 [Act of December 5, 1996 on the professions of doctor and dentist, Journal of Laws 1996, 1997 No.28, item. 152] https://isap.sejm.gov.pl/isap.... (27.07.2021).
6.
Szemik S, Gajda M, Kowalska M. The review of prospective studies on mental health and the quality of life of physicians and medical students. Medycyna Pra. 2020;71(4):483–49.
7.
Chomątowska B, Grzebieluch J, Janiak-Rejno I, What Will You Be Like Doctor ‘Z’? – The Results of Research on Medical Students in Poland in Education Excellence and Innovation Management: A 2025 Vision to Sustain Economic Development during Global Challenges / Soliman Khalid S, editor. IBIMA – International Business Information Management Association. 2020; p. 6697–6706. ISBN 9780999855141.
8.
Dubas-Jakóbczyk K, Domagała A, Kiedik D, Pena-Sánchez JN. Exploring Satisfaction and Migration Intentions of Physicians in Three University Hospitals in Poland. Int J Environ Res Public Health. 2020 Jan;17(1):43.
9.
Goštautaite B, Bučiuniene I, Milašauskiene Ž, Bareikis K, Bertašiute E, Mikelioniene G. Migration intentions of Lithuanian physicians, nurses, residents and medical students. Health Policy. 2018 Oct;122(10):1126–1131.
10.
Győrffy Z, Dweik D, Girasek E. Willingness to migrate—A potential effect of burnout? A survey of Hungarian physicians. Hum Resour Health. 2018 Aug 10;16(1):36.
11.
Krajewski-Siuda K, Szromek A, Romaniuk P, Gericke CA, Szpak A, Kaczmarek K. Emigration preferences and plans among medical students in Poland. Human resources for health. 2012 Dec;10(1):1–6.x.
12.
Waszkiewicz L, Zatońska K, Einhorn J, Połtyn-Zaradna K, Gaweł-Dąbrowska D, Motywacje wyboru studiów medycznych na przykładzie studentów Akademii Medycznej we Wrocławiu [Motivations for choosing medical services at the Medical Academy in Wrocław]. Hygeia Public Health. 2012;74(2):223–226.
13.
Illing J, Morrow G, Kergon C, Burford B, Spencer J, Peile E, Davies C, Baldauf B, Allen M, Johnson N, Morrison J. How prepared are medical graduates to begin practice? a comparison of three diverse UK medical schools. Final report to GMC. 2008 April.
14.
Ranjan P, Kumari A, Chakrawarty A. How can doctors improve their communication skills? J Clin Diagnostic Res. 2015 Mar;9(3):JE01.
15.
Svirko E, Lambert T, Goldacre MJ, Gender, ethnicity and graduate status, and junior doctors’ self-reported preparedness for clinical practice: national questionnaire surveys. J Royal Soc Med. 2014 Feb;107(2):66–74.
16.
Ochsmann EB, Zier U, Drexler H, Schmid K. Well prepared for work? Junior doctors’ self-assessment after medical education. BMC Medical Education. 2011 Dec;11(1):1–9.
17.
Goldacre MJ, Taylor K, Lambert TW. Views of junior doctors about whether their medical school prepared them well for work: questionnaire surveys. BMC Medical Education. 2010 Dec;10(1):1–9.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.